
Joyce Roberts
BHSc Nsg, Post Grad Cert Adv Nsg, Post Grad Dip Adv Nsg, Accredited Diabetes Nurse Specialist
Type 1 diabetes is an autoimmune disease where the body attacks its own insulin-producing cells.
The individual cannot then regulate their own blood sugar levels, which over time, causes harm to the body.
Type 1 cannot be prevented and there is no cure. It is thought that a genetic predisposition triggered by environmental factors causes it.
In this article we take a look at who is most at risk of type 1 diabetes, which factors may play a part in triggering the disease, and how its prevalence is changing on a global scale.
What is Type 1 diabetes?
Type 1 diabetes is a chronic autoimmune condition whose cause remains unknown.[1]
The body’s immune system attacks itself, targeting insulin-producing beta cells, and it either destroys them or suppresses them.
Over time, the person with type 1 diabetes is left with no beta cells, and therefore cannot produce their own insulin.[2]
Type 1 diabetes is essentially absence of significant insulin secretion from the pancreas, eventually leading to total insulin deficiency.
Type 1 diabetes can be autoimmune or non-immune
Autoimmune type 1 results from an autoimmune attack on beta-cells, while non-immune type 1 diabetes is far less common and occurs secondary to other diseases such as pancreatitis.
Studies suggest that type 1 diabetes results from a genetic predisposition, typically combined with an environmental trigger.
When does Type 1 diabetes occur?

Anyone, at any age, can be diagnosed with type 1 diabetes.
With type 1 diabetes, the susceptibility to the disease is inherited, instead of the disease itself being hereditary.[3]
There is strong evidence that type 1 diabetes affects individuals who are born with the genetic tendency to destroy their own insulin-producing beta cells.[4]
Between 10% and 13% of individuals with newly diagnosed type 1 diabetes have a first-degree relative (parent or sibling) with type 1 diabetes.
Type 1 diabetes – New Zealand and worldwide statistics
In 2020, about 277,800 people in New Zealand were estimated as having diabetes, type 1 and type 2.
5-10% of the population have type 1 diabetes
The estimated rate of diabetes was 40 per 1000 population over the last 10 years, which is an increase from 34.3 per 1000 in 2011.
RELATED — Diabetes: Early Signs, Causes, Types and Treatment
The incidence of type 1 diabetes is also increasing – from 10.9 per 100,000 aged 0-14 years in 1990 to 22.5 per 100,000 in the same age group in 2009 globally.[5]
According to the International Diabetes Federation (IDF), there are 537 million adults living with diabetes in the world and that number is expected to increase to 783 million in 2045.[6]
3 in 4 people with diabetes live in low or middle income countries and 1 person is dying every 5 seconds due to diabetes.
In 2021, 6.7 million deaths were due to diabetes.
Top 10 countries with the highest incidence of type 1 diabetes in the 0–14 years age group are
- Finland
- Sweden
- Saudi Arabia
- Norway
- United Kingdom
- United States of America
- Australia
- Kuwait
- Denmark
- Canada
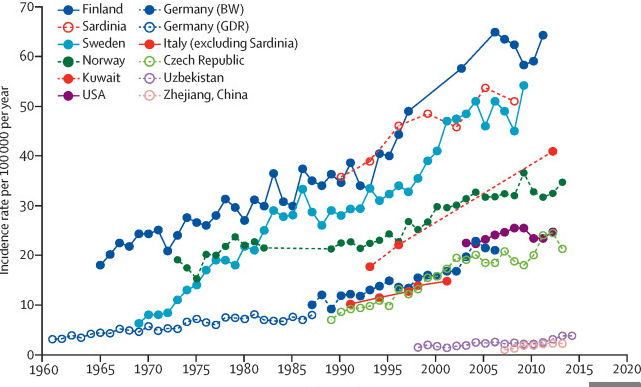
Source: Norris, J.M. Type 1 diabetes—early life origins and changing epidemiology. The Lancet. (2020)
Important note – New Zealand came joint 12th with Germany, and is steadily climbing.
What causes Type 1 diabetes and who is most at risk?
Type 1 diabetes is one of the most well-characterized autoimmune diseases whose cause remains unknown, though multiple potential factors are thought to play a part.
Viruses as type 1 diabetes trigger
Viral disease induction of type 1 diabetes has been recognised as one of the main potential environmental triggers.
Certain types of viral infections such as
- Cytomegaloviruses
- Mumps
- Congenital rubella
- Epstein-Barr virus
have been implicated as potential triggers. The presence of a viral infection can lead to immune cell activation.
Imbalances within the immune system may promote immune activation while undermining immune regulation.
This is where stress has also been linked in advancing the development of type 1 diabetes given the effect it has on our hormones and lowering our immune system over the long term.
Stress may play a role in developing type 1 diabetes
Genetics and type 1 diabetes
Environmental factors and type 1 diabetes
Our environment and different environmental factors are thought to have a significant contribution to the development of type 1 diabetes.
Specific environmental factors that are being investigated include
- dietary compounds (including cow’s milk)
- wheat/gluten
- soy products
- fats
- coffee and tea
- vitamin deficiencies
- other toxins[9]
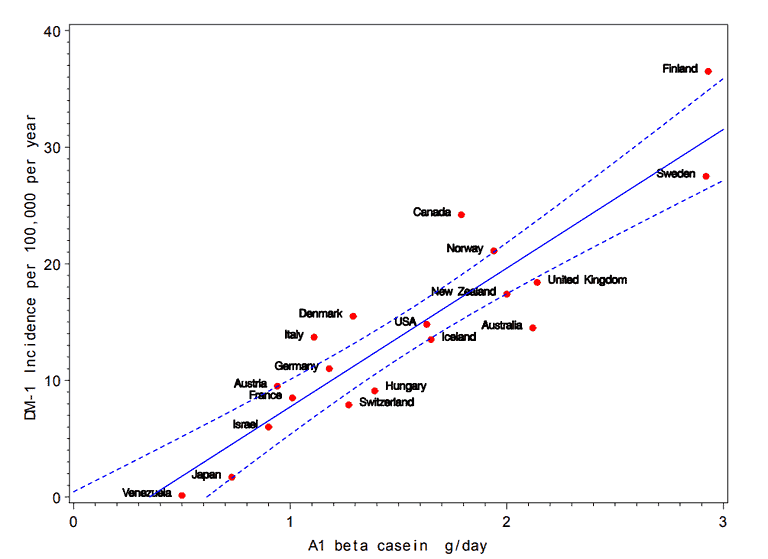
Source: Laugesen, M. Ischaemic heart disease, Type 1 diabetes, and cow milk A1 beta-casein. New Zealand medical journal. (2003)
Analytical epidemiological studies have also identified other environmental risk factors operating early in life, such as
- enteroviral infections (in pregnant women)
- older maternal age
- pre-eclampsia
- cesarean section
- early introduction of cow’s milk[10]
The TEDDY study (The Environmental Determinants of Diabetes in the Young) is an international multi-centre trial researching the potential causes of type 1 diabetes in children and is ongoing.
The study was designed to follow children with and without a family history of type 1 diabetes to understand the environmental factors that contribute to the disease.[11]
The hygiene hypothesis is another environmental trigger that is being studied. It proposes that decreased exposure to infectious agents at a young age results in an immaturity of the immune system and an increase in immune-modulated disorders.[12]
Geography and type 1 diabetes prevalence
There is a large geographical variation in the incidence of type 1 diabetes.
The DiaMond study – WHO multinational project for childhood diabetes – reported from 1990-1994 that the incidence rates of type 1 diabetes were highest in Sardinia and Finland.
These populations are 3000 km from each other and have different environments and distinctive genetic backgrounds.[13]
This shows that the impact and prevalence of geography on type 1 diabetes is less clear.
Age and type 1 diabetes
In the past type 1 diabetes was described as a disease of childhood and early adulthood, most people being younger than 20 years of age at diagnosis.[14]
Although the incidence peaks in puberty and early adulthood, new onset type 1 diabetes occurs in all age groups.
There is a significant trend in decreasing age at presentation of type 1 diabetes, particularly in the children younger than 5 years.
Type 1 diabetes incidence peaks at puberty age
A New Zealand study conducted over a 20 year period (1990-2009) in Auckland looked at the incidence of type 1 diabetes in children under the age of 15 years.
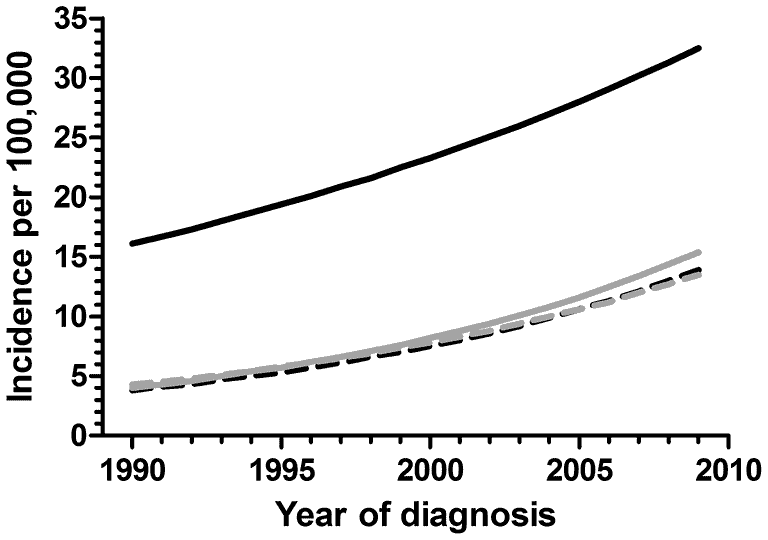
Source: Reed, P.W. Increasing Incidence and Age at Diagnosis among Children with Type 1 Diabetes Mellitus over a 20-Year Period in Auckland (New Zealand). Plos One. (2012)
There were 884 new cases covered by the study and they found that the yearly increase was the greatest in the 10-14 year age group. The research team also discovered the new cases were moderately more frequent in winter and less frequent in spring.[15]
Can Type 1 diabetes be prevented?
Type 1 diabetes is neither preventable or curable at the moment, and the cause remains unknown.
There is some hope in preventing type 1 diabetes through preliminary work looking at interfering with the autoimmune process by expanding specific cells or by blocking antibodies.
Two studies, the Diabetes Prevention trial (DPT) that ran from 1996-2000 and the European Nicotinamide Diabetes Intervention Trial (ENDIT) that ran from 1990-1995, looked at
- using high dose nicotinamide therapy
- the efficacy of low dose insulin injections
in first-degree relatives of patients with type 1 diabetes, who are deemed at high risk of developing diabetes. Neither study, however, showed any promising data.[16]
New areas of research include stem cell therapy, non-immunomodulatory adjunctives and immune focused therapies.[17]
Related Questions
1. What is DKA – Diabetic acidosis and is it dangerous?
Diabetic Ketoacidosis (DKA) is a life threatening but preventable acute complication of type 1 diabetes, characterized by hyperglycemia, metabolic acidosis and ketosis.[18]
2. What is diabetes life expectancy?
Males with type 1 diabetes live 7 years less, while women live 8.5 years less than their non-diabetic counterparts.
Prior to the discovery of insulin a century ago, type 1 diabetes was associated with a life expectancy as short as a few months.[19]
3. What is the difference between type 1 diabetes and type 2 diabetes?
Type 1 diabetes individuals are dependent on injected insulin as a life-long therapy, while with type 2 there is no requirement for insulin to preserve one’s life.
Misclassification of type 1 diabetes in adults is common and over 40% of those developing type 1 diabetes after age 30 years are initially treated as having type 2 diabetes.
Recommended reading for the person with type 1 diabetes: Adam Brown’s Bright Spots and Landmines.
If you are interested in learning more about diabetes, we suggest checking our section on Health Conditions.
Joyce has been nursing since the 1980s, and for the past 20 years she has been focusing on patients with diabetes.
Given that diabetes can be a debilitating disease if not managed properly, Joyce’s focus is to ensure that individuals with diabetes have all the correct information. She works diligently and her focus is to prepare, inform and make sure that the individuals are well equipped with knowledge and support to live with the disease 24 hours a day.
References
(1) Beyond Type 1 diabetes site: https://beyondtype1.org
(2) Drury, P., Gatling, W. (2005) Diabetes. Your Questions Answered.
(3) McDowell, Joan,Matthews, David,Brown, Florence. (2007) Diabetes: a handbook for the primary healthcare team.
(4) McCance, K., Huether, S., Brashers, V., Rote, N. (2010) Pathophysiology.The Biologic Basis for Disease in Adults and Children.
(5) Soltesz, G., Patterson, CC., Dahlquist, G. (2007). Worldwide childhood type 1 diabetes incidence – what can we learn from epidemiology? Pediatric Diabetes.
(6) Diabetes now affects 1 in 10 adults worldwide. IDF site.
(7) Pociot, F., Akolkar, B et al. (2010). Genetics of type 1 diabetes: What’s Next? Diabetes journal. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2889752/
(8) Katsarou, A., Gudbjornsdottir, S., et al. (2017). Type 1 diabetes mellitus. Nature reviews/Disease Primers.
(9) Morran, M., Omenn, G., Pietropaolo, M. (2008). Immunology and Genetics of Type 1 Diabetes. Mount Sinai Journal of Medicine.
(10) Viskari, H., Knip, Mikael., et al (2012). Maternal Enterovirus Infection as a Risk Factor for Type 1 Diabetes in the Exposed Offspring. Diabetes Care. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3357251/
(11) The TEDDY study (The Environmental Determinants of Diabetes in the Young). https://teddy.epi.usf.edu/
(12) Effect of standard nicotinamide in the prevention of type 1 diabetes in first degree relatives of persons with type 1 diabetes by Eduardo Cabrera-Rode et al. In the Autoimmunity paper June 2006.
(13) Karvonen, M., Vilik-Kajander,. Moltchenova, E. et al. (2000). Incidence of childhood Type 1 diabetes worldwide. Diabetes Mondiale (DiaMond) Project. Diabetes Care.
(14) Soltesz, G., Patterson, CC., Dahlquist, G. (2007). Worldwide childhood type 1 diabetes incidence – what can we learn from epidemiology? Pediatric Diabetes.
(15) Derraik, J., Reed,P., Jeffries, C., et al. (2012). Increasing Incidence and Age at Diagnosis among Children with Type 1 Diabetes Mellitus over a 20 year Period in Auckland (New Zealand) https://doi.org/10.1371/journal.pone.0032640
(16) Gale, E., Bingley, P., Emmett, C. Collier, T. (2004). European Nicotinamide Diabetes Intervention Trial (ENDIT): a randomized controlled trial of intervention before the onset of Type 1 diabetes.
(17) Von Scholten, Bernt Johan., Kreiner, Frederik., Gough, Stephen., von Herrath, Matthias. (2021). Current and future therapies for Type 1 diabetes. Diabetologia.
(18) Umpierrez, G., Korytkowski, M. (2016). Diabetic emergencies-ketoacidosis, hyperglycemic hyperosmolar state and hypoglycemia. National Review Endocrinology.
(19) McCance, K., Huether, S., Brashers, V., Rote, N. (2010). Pathophysiology. The Biologic Basis for Disease in Adults and Children.

