
Kelly Wright
CNC (Certified Nutrition Consultant - pregnancy, postpartum & baby nutrition), Certified Holistic Nutrition Coach
Pregnancy greatly increases nutritional needs and places extra demands on the body that food alone can’t always cover.
This article will help you understand where the most common nutritional gaps are and how to nourish yourself and your baby with confidence.
In a 2022 Vancouver study, iron deficiency among pregnant women increased from 28% in early pregnancy to 81% in late pregnancy, despite daily supplementation with 27mg of elemental iron, the amount recommended in standard prenatal guidelines.[1]
Participants were consuming a prenatal vitamin that technically met the RDA, yet most still became deficient as pregnancy progressed.
Only 41% of women who were iron deficient in late pregnancy reported taking any additional iron beyond what was provided in their prenatal.[1]
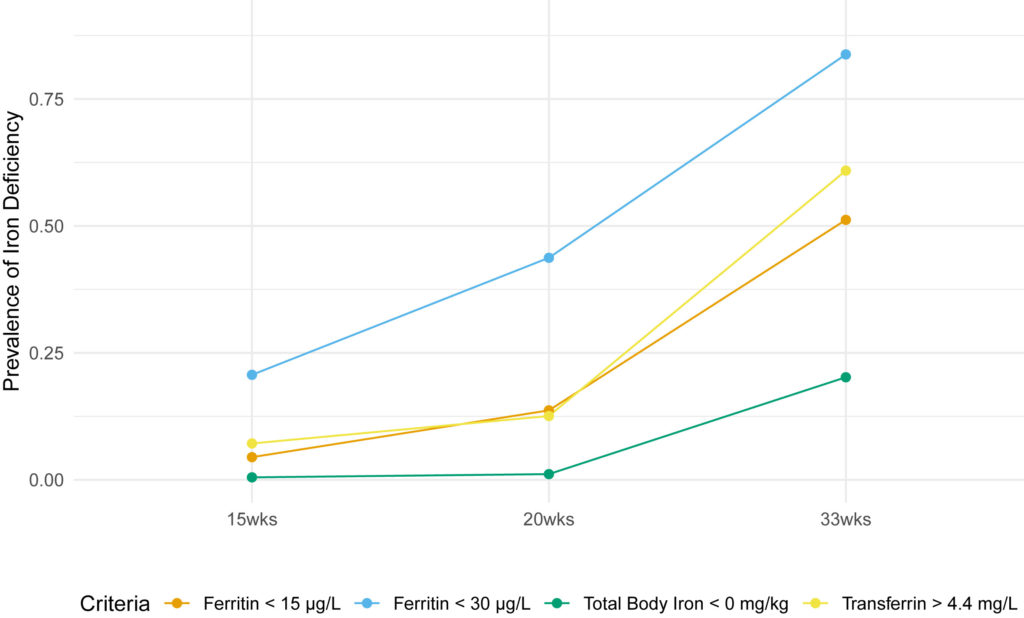
Longitudinal evaluation of iron status during pregnancy: a prospective cohort study in a high-resource setting McCarthy, Elaine K et al. The American Journal of Clinical Nutrition, Volume 120, Issue 5, 1259 - 1268
These findings highlight a concerning gap between guideline-based intake and actual iron status, suggesting that the current RDA may not be sufficient for many women in later pregnancy.
This is especially the case when demands for iron significantly increase due to fetal growth and expanded maternal blood volume.[1]
A Brazilian study found that 6.2% of 676 pregnant women had vitamin A deficiency, even though they received prenatal care that included prenatal vitamin supplementation, classifying it as a mild public health issue.[2]
This mirrors broader global concerns, with the World Health Organisation estimating that nearly 19 million pregnant women worldwide are affected.[2]
RELATED — Vitamin A (for healthy eyes, glowing skin and strong immunity)
During pregnancy, vitamin A requirements rise, particularly in the third trimester when fetal organ development accelerates. Infection, inflammation, and gestational conditions like diabetes can further increase risk.[2]
Vitamin A requirements increase in the third trimester when fetal organ development accelerates
Low maternal vitamin A has been linked to a higher risk of fetal growth restriction and impaired development of organs such as the kidneys and pancreas.[2]
In a 2024 study, 57.7% of pregnant women were vitamin D deficient.[4] Despite daily supplementation with 1000 IU, 67% of those initially deficient remained so, 30% of those with insufficiency became deficient, and 26.5% of those with sufficient levels at 12 weeks had dropped to insufficient by 28 weeks.[4]
These results highlight concerns that low-dose supplementation may not be adequate for many pregnant women, even in regions with abundant sunlight.
RELATED — Vitamin D: The sunshine hormone for stronger bones
The study also found that over 80% of participants reported consuming a diet rich in vitamin D, and 90% adhered to the supplement regimen more than three times per week, yet meaningful improvements in vitamin D status were not observed.[4]
At 28 weeks, nearly half the cohort remained deficient, and fewer than one in four had achieved sufficient levels.[4]
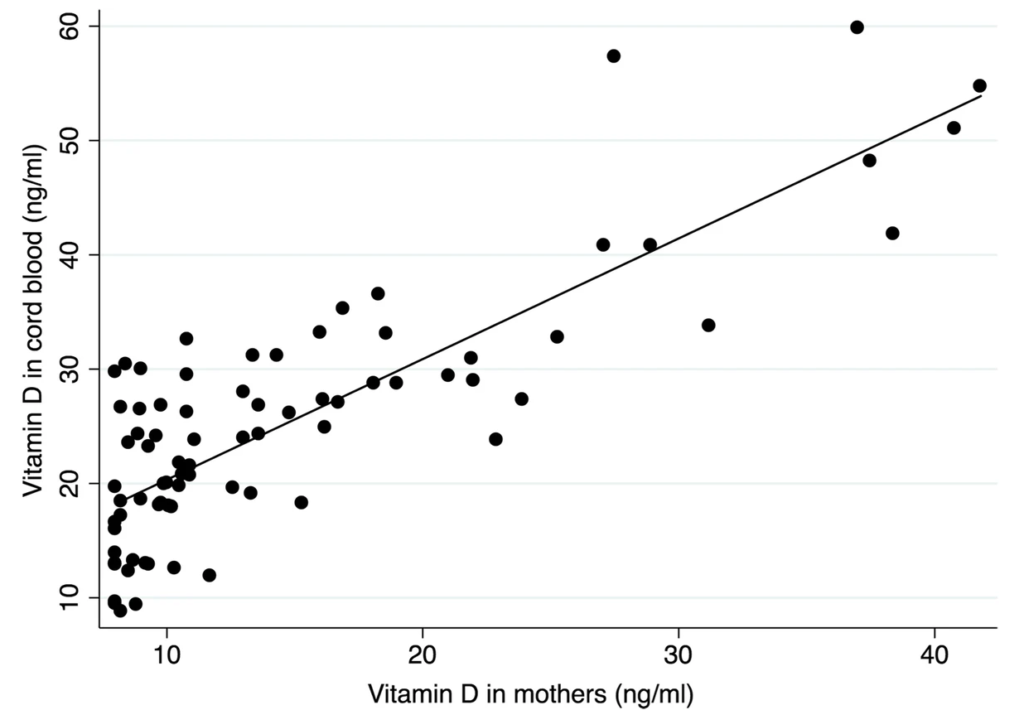
Shrestha, D., Budhathoki, S., Pokhrel, S. et al. Prevalence of vitamin D deficiency in pregnant women and their babies in Bhaktapur, Nepal
These findings reflect a growing body of evidence questioning whether current prenatal vitamin D guidelines, often based on prevention of rickets rather than optimising maternal-fetal outcomes, are sufficient to meet physiological demands in pregnancy.
Despite being recognised as an essential nutrient for over 25 years, choline remains one of the most overlooked micronutrients in prenatal care.
Choline plays a foundational role in
- fetal brain development
- neural tube formation
- methylation
- liver function
yet most pregnant women are not meeting their daily needs.
A 2022 German study revealed that 93% of pregnant women had inadequate choline intake despite 97% using supplements during pregnancy; only 5% were taking supplements that contained choline.[5]
This aligns with broader evidence showing that choline is rarely included in prenatal vitamins, and dietary intakes in pregnancy often fall well below recommended levels.[5]
Insufficient intake of choline has been associated with
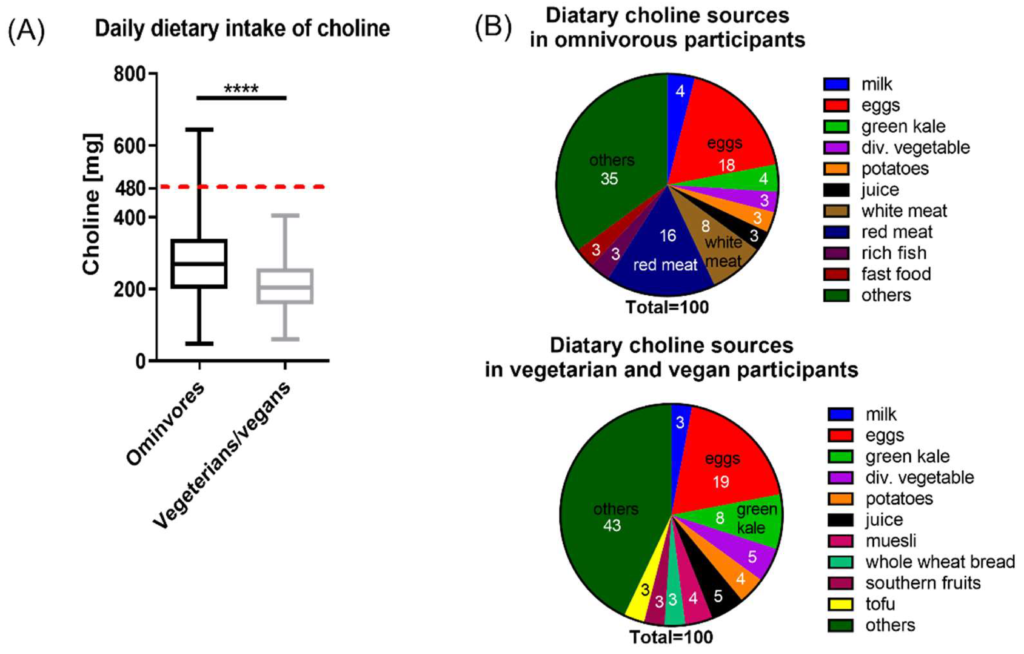
Roeren, M., Kordowski, A., Sina, C., & Smollich, M. (2022). Inadequate Choline Intake in Pregnant Women in Germany. Nutrients, 14(22).
As research continues to reinforce the importance of choline, it is essential to consider both food-based and supplemental sources to close this critical gap.
In a 2022 Portuguese study, 81.6% of pregnant women were taking the recommended 200 μg/day iodine supplement, yet only 20.7% reached adequate iodine status, and 18% remained severely deficient.[7]
Despite adherence to supplementation guidelines, the majority of women had insufficient levels, highlighting that iodine intake from supplements alone may not be enough to meet pregnancy demands.
The study also found that women who began supplementation earlier, ideally before conception, had better iodine status overall, suggesting timing matters as much as dosage.[7]
Iodine is essential for fetal brain and thyroid development
Since iodine is essential for fetal brain and thyroid development, these findings raise important questions about whether current public health strategies effectively address this critical nutrient gap.
A Canadian study found that even with daily supplementation of 400mg DHA during pregnancy, some infants still showed signs of inadequate omega-3 status at birth.[8]
Mothers who did not supplement had babies who were more than three times as likely to experience delayed language development and 2.5 times as likely to show a reduction in visual clarity.[8]
While DHA supplementation is commonly recommended, this study highlights a key concern, consistent supplementation may not fully bridge the gap.[8]
Blood levels of DHA at delivery remained suboptimal in many cases, pointing to broader issues in absorption, individual nutrient demands, and dietary intake throughout pregnancy.
Omega-3 fatty acids, especially DHA, are critical for the
- developing brain
- eyes
- nervous system
Yet, average dietary intakes in pregnancy often fall short, particularly where fish consumption is low or highly processed diets are common.[9,10]
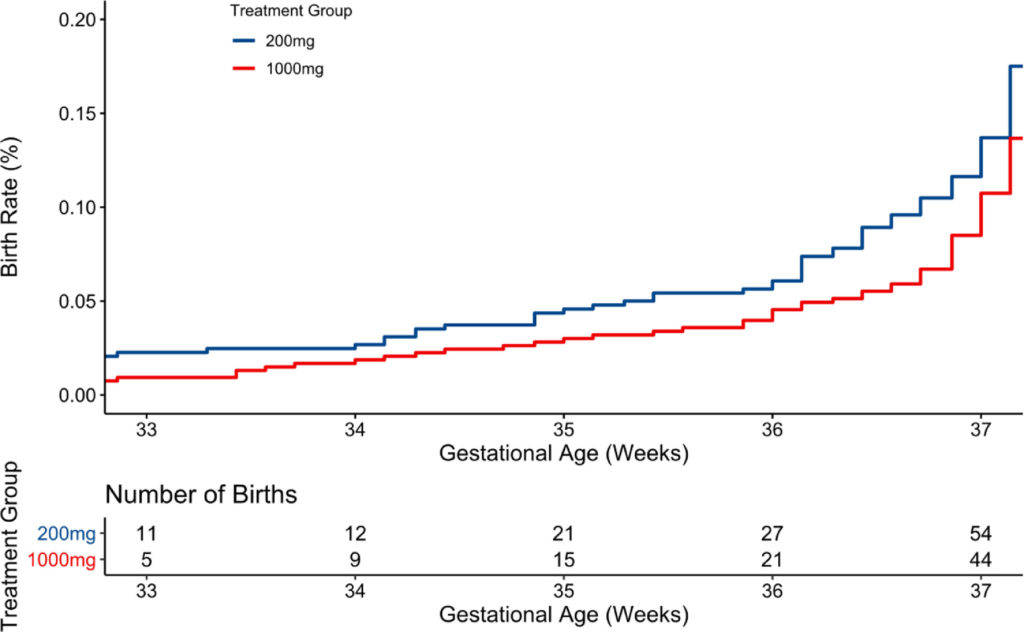
Higher dose docosahexaenoic acid supplementation during pregnancy and early preterm birth: A randomised, double-blind, adaptive-design superiority trial. Carlson, Susan E et al. ClinicalMedicine, Volume 36.
Recognising where these shortfalls occur empowers mums to make food-first choices that fill the gap, like regularly including oily fish such as salmon, sardines, and mackerel, which offer highly bioavailable DHA.
Related Questions
1. What is the best nutrition for a pregnant woman?
A diet emphasising whole, nutrient-dense foods, pasture-raised meats, eggs, wild fish, fermented foods, seasonal produce, and healthy fats supports the baby’s development and maternal health and wellbeing.
2. What are prenatal nutrients?
Prenatal nutrients are essential vitamins and minerals required during pregnancy.
They include folate, iron, choline, B12, vitamin D, magnesium, omega-3s (DHA), and iodine, to support fetal development and maternal health.
3. Should I avoid bananas during pregnancy in the first trimester?
No, bananas can be nourishing in the first trimester.
They provide vitamin B6, potassium, and gentle energy. Pair them with quality protein or healthy fats to support blood sugar balance.
Kelly is a Certified Nutrition Consultant specialising in pregnancy, postpartum, and infant nutrition. With a strong foundation in both modern nutritional science and ancestral food wisdom, she supports women through the critical perinatal period with an emphasis on real food, bioavailable nutrients, and practical, evidence-based care…
If you would like to learn more about Kelly, see Expert: Kelly Wright.
References
(1) Cochrane, K.M., Hutcheon, J.A., & Karakochuk, C.D. (2022). Iron-deficiency prevalence and supplementation practices among pregnant women: a secondary data analysis from a clinical trial in Vancouver, Canada. The Journal of Nutrition.
(2) Maia, S.B., Souza, A.S.R., Caminha, M.F.C., da Silva, S.L., Cruz, R.S.B.L.C., et al. (2019). Vitamin A And Pregnancy: A Narrative Review. Nutrients. https://www.mdpi.com/2072-6643/11/3/681
(3) Jouanne, M., Oddoux, S., Noël, A., & Voisin-Chiret, A.S. (2021). Nutrient Requirements During Pregnancy And Lactation. Nutrients. https://www.mdpi.com/2072-6643/13/2/692#
(4) Abdelmageed, R.M., Hussein, S.M.M., Anamangadan, S.M., et al. (2024). Prospective Cohort Study of Vitamin D Deficiency in Pregnancy: Prevalence And Limited Effectiveness of 1000 IU Vitamin D Supplementation. Women’s Health. https://journals.sagepub.com/doi/full/10.1177/17455057231222404
(5) Roeren, M., Kordowski, A., Sina, C., & Smollich, M. (2022). Inadequate Choline Intake in Pregnant Women in Germany. Nutrients. https://journals.sagepub.com/doi/full/10.1177/17455057231222404
(6) Derbyshire, E.J. (2025). Choline in Pregnancy And Lactation: Essential Knowledge for Clinical Practice. Nutrients. https://pmc.ncbi.nlm.nih.gov/articles/PMC12073457/
(7) Lopes, C.A., Prazeres, S., Martinez-de-Oliveira, J., Limbert, E., & Lemos, M.C. (2022). Iodine Supplementation in Pregnancy in an Iodine-Deficient Region: A Cross-Sectional Survey. Nutrients. https://www.mdpi.com/2072-6643/14/7/1393
(8) Mulder, K.A., King, D.J., & Innis, S.M. (2014). Omega-3 Fatty Acid Deficiency in Infants Before Birth Identified Using a Randomized Trial of Maternal DHA Supplementation in Pregnancy. PLoS One. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0083764
(9) Brown, B., & Wright, C. (2020). Safety And Efficacy of Supplements in Pregnancy. Nutrition Reviews. https://academic.oup.com/nutritionreviews/article/78/10/813/5700577
(10) Basak S, Mallick R, Duttaroy AK. Maternal Docosahexaenoic Acid Status during Pregnancy and Its Impact on Infant Neurodevelopment. Nutrients. https://pmc.ncbi.nlm.nih.gov/articles/PMC7759779/


