
Morgan Hancock
M.Ost, BAppSci (Human Biology & Physiology), BSc, PGCert (Western Medical Acupuncture)
Osteopathy is a holistic approach to healthcare that focuses on treating the body as a unified system, rather than addressing symptoms in isolation.[1]
By leveraging manual therapy techniques, osteopaths aim to
- improve overall body function
- reduce pain
- promote long-term health
Osteopathic treatment can effectively address a wide range of conditions that many people experience in their lives, which will be explored in more detail throughout this article.
Overview — Health benefits of osteopathy
Osteopaths are trained in and use a wide range of techniques aimed at addressing your specific presentation. The range of techniques that an osteopath may employ, and how they are applied, is outlined below.
Muscle energy
Increase range of motion of restricted areas, stretch tight muscles, reduce chronic pain, and improve circulation and lymphatic flow throughout the body.
Myofascial release
Release constricted tissues within the musculoskeletal systems to facilitate blood flow and lessen pain.
Balanced ligamentous tension
Increase range of motion in restricted joints in the whole body, such as the knee, TMJ ankle, shoulder, or fingers.
Diaphragm doming
Improve diaphragmatic excursion. Secondary uses: decrease cervical thoracic, and lumbar pain due to multiple attachments and improve circulation.
Indirect diaphragm release
Decrease cervical thoracic and lumbar pain due to multiple attachments and improve circulation.
High Velocity Low Amplitude (HVLA)
Decrease joint pain, improve mobility and improve range of motion.
Lymphatic pump
Used in gastrointestinal tract infections, respiratory infections and edema. Secondary uses: improve immune function and vaccination efficacy.
Rib raising
Decrease sympathetic nervous system activity, increase respiratory excursion, increase chest wall mobility and lymphatic flow.
Cranial osteopathy
Promote functioning of the primary respiratory mechanism, treats somatic dysfunction of the skull bones, tissues, dura, and overlying fascia, reducing symptom burdens related to concussions.
Sports injuries and rehabilitation
Osteopathy is an effective treatment for sports-related injuries.[2,3] By addressing musculoskeletal imbalances and improving joint mobility, osteopathic treatment can help athletes recover from injuries more quickly and efficiently.
Benefits of osteopathic treatment in sports injuries:
- Restores range of motion and function after injury
- Reduces inflammation and swelling
- Prevents re-injury by improving joint stability and muscular function
In addition to treating acute injuries, osteopathy can also be utilised for injury prevention.
After the initial recovery period is over, the risk of re-injury can be quite high for several months, as muscles complete the repair process, but the pain experienced is no longer present to serve as a warning about the weakened region.
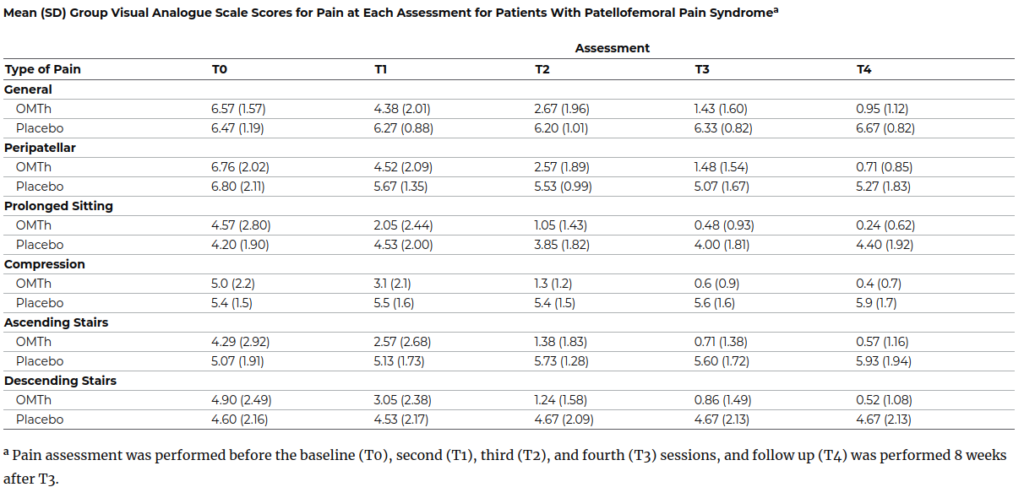
A 2020 study on osteopathy for patellofemoral pain, a common knee injury, showed an 85% reduction in general pain by treatment’s end, compared to no significant change in the placebo group.[4]
Specific improvements included a 90% decrease in pain from prolonged sitting and an 88% reduction during stair ascent, highlighting osteopathy’s effectiveness in alleviating pain and improving mobility.
Osteopathy can also be used for injury prevention
Regular osteopathic treatment helps maintain body balance and alignment, reducing strain on muscles and joints. This proactive approach decreases the likelihood of overuse injuries supporting long-term musculoskeletal health.[1]
Acute injuries
Whether from a fall, car accident, or sudden trauma, acute injuries often involve pain, inflammation, and restricted movement.
Osteopathic treatment can support the healing process facilitating natural recovery mechanisms and, if applicable, by addressing the underlying cause of the injury.
Osteopathy aids in acute injury recovery by[5,6]
- Promoting circulation to speed healing
- Reducing muscle tension and joint stiffness
- Supporting the body’s inflammatory response to control pain and swelling
The body attempts to adapt to injuries while healing, such as limping from ankle pain. After healing, addressing the muscles and joints that compensated is crucial for a proper recovery.[7]
Chronic pain management
Chronic pain, defined as pain persisting beyond the expected healing time or without a clear cause, can significantly impact an individual’s quality of life.[8]
Unlike acute pain, which serves as a protective mechanism, chronic pain often becomes a persistent issue that requires comprehensive management.
The following table shows how different parts of the nervous system contribute to chronic pain and how we experience it.
The forebrain deals with the emotional side of pain, like fear, anxiety, and stress. The spinal cord and pain pathways can make injuries feel worse by increasing sensitivity to pain.
RELATED — Understanding Stress: The Silent Killer
Lastly, changes in how the brain senses and controls the body can lead to things like altered movement or a distorted sense of body size and position.[9]
| Forebrain (medial pain system) | Spontaneous fluctuations in pain. Motivation is oriented to avoidance and escape from pain. Psychological aspects related to pain include fear-avoidance, anxiety, depression, catastrophization, somatization, worry, increased vigilance. |
| Descending pain modulatory systems | Sensitization. Increase/exaggerated pain perception in the area of injury (hyperalgesia). Cutaneous stimuli perceived as painful (allodynia). Pain thresholds may be decreased (pressure and thermal). |
| Dorsal Horn of the Spinal cord | |
| Somatosensory cortex | Altered Two Point Discrimination. Impaired performance in the Left Right Judgement Task. Change in perception of body image including size of the limb, altered body midline. |
| Primary motor cortex | Changes in motor control including co-contraction and loss of ability to selectively recruit individual muscles. |
Osteopathic treatment offers a unique approach to addressing chronic pain by integrating manual therapy with a thorough understanding of pain mechanisms.
Osteopaths use a range of techniques to alleviate chronic pain. These include:
- Helping patients understand pain mechanisms and management strategies
- Tailoring exercises to improve function and decrease pain
- Understanding that chronic pain often involves more than just the injured area to help address underlying issues
Osteopaths are among the few healthcare professionals who specialise in pain science. This specialisation in pain management allows osteopaths to offer nuanced and effective care for those struggling with chronic pain, contributing to better long-term outcomes for their patients.[10,11]
Lower back pain is one of the most common chronic pain conditions, affecting an estimated 20% of adults worldwide at some point in their lives.
Research, including systematic reviews and meta-analyses, indicates that osteopathic treatment can significantly reduce pain intensity, with results comparable to those of nonsteroidal anti-inflammatory drugs.
Additionally, long-term follow-ups show that individuals receiving osteopathic treatment often have a reduced reliance on prescription medications for managing low back pain.
Headaches and migraines
Headaches and migraines are often linked to tension in the neck, shoulders, or cranial muscles.
Several studies have shown that osteopathic techniques that relieve this tension can reduce both the frequency and intensity of headaches.[12,13]
Osteopathy’s impact on headaches:
- Releases muscle tension in the neck and shoulders
- Improves spinal alignment, reducing strain on cranial nerves
- Enhances blood flow to the head and neck, reducing inflammation
Osteopathy can be a valuable tool in long-term management of headaches, especially for individuals suffering from chronic migraines.
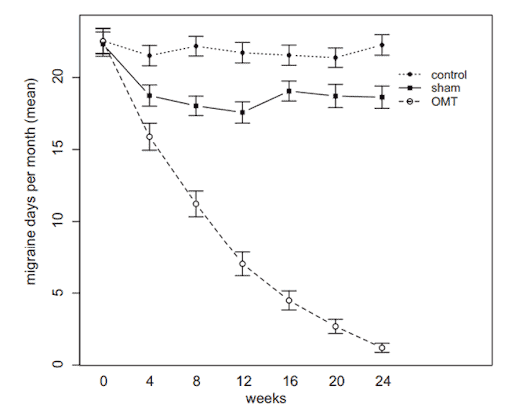
A 2015 study showed significant improvements in migraine frequency, with a reduction from over 20 days per month to less than 2 days per month by the study’s end.[13]
In contrast, the control group saw no change, and the sham group plateaued after an initial reduction.
Your osteopath may also arrange imaging to investigate reasons for your headaches or neck tension that go beyond stress or work. In modern society, “Tech Neck” is now a common issue, in particular for teenagers.[14]
Osteopathy has proven to be efficient in reducing migraine frequency
Hours a day hunched over a device and laptop causing constant compression of the cervical nerves results in a range of long term physical issues.
These can include chronic headaches, numbness in the hands, persistent neck pain and cervical disc damage.
References
(1) Johnson, A. (2024). Osteopathic medicine: A holistic approach to healthcare. Current Research: Integrative Medicine, Volume 9(01): 1-2 https://www.pulsus.com/scholarly-articles/osteopathic-medicine-a-holistic-approach-to-healthcare.pdf
(2) Delgadillo, B. E., Bui, A., Debski, A. M., Miller, B., & Wu, DO, S. S. (2024). Efficacy of Osteopathic Manipulative Treatment for Pain Reduction in Patients With Patellofemoral Pain Syndrome: A Meta-Analysis of Randomized Controlled Trials. Cureus. https://doi.org/10.7759/cureus.59439
(3) Yao, S. C., Zwibel, H., Angelo, N., Leder, A., & Mancini, J. (2020). Effectiveness of osteopathic manipulative medicine vs concussion education in treating student athletes with acute concussion symptoms. Journal of Osteopathic Medicine, 120(9), 607–614. https://www.degruyter.com/document/doi/10.7556/jaoa.2020.099/html
(4) Tramontano, M., Pagnotta, S., Lunghi, C., Manzo, C., Manzo, F., Consolo, S. & Manzo, V. (2020). Assessment and management of somatic dysfunctions in patients with patellofemoral pain syndrome. Journal of Osteopathic Medicine, 120(3), 165-173. https://doi.org/10.7556/jaoa.2020.029
(5) Verzella, M., Affede, E., Di Pietrantonio, L., Cozzolino, V., & Cicchitti, L. (2022). Tissutal and Fluidic Aspects in Osteopathic Manual Therapy: A Narrative Review. Healthcare (Basel, Switzerland), 10(6), 1014. https://doi.org/10.3390/healthcare10061014
(6) Waxenbaum, J. A., Woo, M. J., & Lu, M. (2024). Physiology, Muscle Energy. In StatPearls. StatPearls Publishing.
(7) Halson w, Glasgow P. Recovery. In: Brukner P, Clarsen B, Cook J, Cools A, Crossley K, Hutchinson M, McCrory P, Bahr R, Khan K. eds. Brukner & Khan’s Clinical Sports Medicine: Injuries, Volume 1, 5e. McGraw-Hill Education; 2017.
(8) Licciardone, J. C., Schultz, M. J., & Amen, B. (2020). Osteopathic manipulation in the management of chronic pain: Current perspectives. Journal of Pain Research, Volume 13, 1839–1847. https://doi.org/10.2147/JPR.S183170
(9) René Pelletier, Daniel Bourbonnais, Johanne Higgins, Nociception, pain, neuroplasticity and the practice of Osteopathic Manipulative Medicine, International Journal of Osteopathic Medicine,Volume 27,2018,Pages 34-44, https://doi.org/10.1016/j.ijosm.2017.08.001
(10) Cicchitti, L., Martelli, M., & Cerritelli, F. (2015). Chronic Inflammatory Disease and Osteopathy: A Systematic Review. PLOS ONE, 10(3), e0121327. https://doi.org/10.1371/journal.pone.0121327
(11) Gillan, R., Bachtel, G., Webber, K., Ezzair, Y., Myers, N. E., & Bishayee, A. (2024). Osteopathic manipulative treatment for chronic inflammatory diseases. Journal of Evidence-Based Medicine, 17(1), 172–186.
(12) Cerritelli, F., Lacorte, E., Ruffini, N., & Vanacore, N. (2017). Osteopathy for primary headache patients: a systematic review. Journal of Pain Research, Volume 10, 601–611. https://doi.org/10.2147/JPR.S130501
(13) Cerritelli, F., Ginevri, L., Messi, G., Caprari, E., Di Vincenzo, M., Renzetti, C., … Provinciali, L. (2015). Clinical effectiveness of osteopathic treatment in chronic migraine: 3-Armed randomized controlled trial. Complementary Therapies in Medicine, 23(2), 149–156.
(14) Tsantili AR, Chrysikos D, Troupis T. Text Neck Syndrome: Disentangling a New Epidemic. Acta Med Acad. 2022 Aug;51(2):123-127. doi: 10.5644/ama2006-124.380. PMID: 36318004; PMCID: PMC9982850. https://pmc.ncbi.nlm.nih.gov/articles/PMC9982850/






