
Morgan Hancock
M.Ost, BAppSci (Human Biology & Physiology), BSc, PGCert (Western Medical Acupuncture)
The next time you’re on a train, bus, or sitting in a café, take a silent headcount: how many people around you are bent over their phones or tablets? This everyday snapshot illustrates the scale of a modern phenomenon — tech neck — a posture-related strain that’s crept into our daily lives over the past decade.
Tech neck describes the strain and microtrauma imposed on the cervical spine by sustained forward head posture (FHP) during the frequent use of smartphones, tablets, and other portable devices.
What’s unique about this phenomenon is its ubiquity and recurrence; billions of users worldwide spend hours daily hunched over screens, leading to a modern epidemic of posture-related cervical stress.
The Weight of Modern Posture
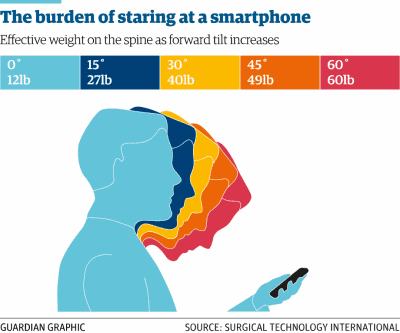
The human head weighs approximately 5 kg, but biomechanical modeling has demonstrated how the head’s effective weight increases dramatically with forward inclination—from 5 kg at neutral to 27 kg when tilted forward 60°, magnifying cervical loading nearly fivefold.[1]
That’s the equivalent of carrying a four-year-old child on your neck every time you’re on a phone or tablet.
Having your head tilted forward at 60°, increases its weight from 5kg to 27kg
Modern device use often involves holding screens far below eye level, forcing the neck into sustained flexion for extended periods. Unlike brief glances down while reading or writing, today’s digital engagement spans hours. This isn’t a short-lived phase—it’s a habitual posture repeated across thousands of hours per year.
Children as young as two are engaging with screens. People currently in their late 20s have been using mobile devices since their late teens, and early studies are already showing increased neck and back complaints in this demographic.[2]
Generation Alpha, growing up with tablets in hand from as young as primary school, and now Generation Beta, using devices while in the pram, may be the first groups with true lifelong exposure.
We are only just beginning to understand what this means for their future spinal health.
Structural and Physiological Adaptation
Time Under Tension
What once might’ve been a quick check of Instagram often stretches into hours daily and the chronic nature of device engagement has profound implications.
Earlier estimates suggested users might spend 2–4 hours daily on smartphones or tablets, but more recent data indicate that this significantly underestimates the true exposure—particularly among adolescents.
Surveys from 2025 report that teenagers average over 7 hours and 22 minutes of daily screen time, excluding school-related use.[3]
This level of usage translates to approximately 3,000 hours of sustained forward head posture per year, dramatically increasing cumulative mechanical stress on the cervical spine.
Such repetitive loading of the head and neck structures amplifies the risk of
- postural strain
- disc compression
- early degenerative change
Childhood diabetes was once dubbed the hidden epidemic, costing global healthcare systems hundreds of billions annually.[4] Tech neck may be next—not with the immediate, systemic threat of metabolic disease, but with a cumulative musculoskeletal toll that’s less dramatic, yet no less expensive over time.
With data showing that up to 93 % of young adult students already exhibiting signs of posture-related neck strain, and 69 % of children and adolescents reporting neck pain linked to screen use, the future financial implications are clear.[2]
Data suggest that 93 % of young adult students exhibit signs of posture-related neck strain
Adaptation vs Degeneration
We’ve had ergonomic challenges before. In the 1990s, the concern was being hunched over keyboards, but monitors were at least set at eye height. The tablet and smartphone revolution has merged the keyboard and the screen—then dropped it into our laps.
The body adapts to chronic posture—just not always in helpful ways. It’s like watching seedlings grow in a cardboard box with a single light hole—the stems stretch, bend, and shape around the light.
RELATED — Have you got poor posture? (18 long-term effects and health risks)
Our children’s necks are bending the same way—guided by hours spent at a 60° angle—that plant metaphor becomes alarmingly real.
In response to sustained forward head positioning, anterior cervical muscles shorten, posterior stabilisers weaken, and the natural lordotic curve of the neck begins to flatten.[5]
This is not theoretical; imaging studies confirm these changes even in young people with heavy device use.[6] Some show early kyphotic patterns—an outward bowing of the neck—once seen only in elderly patients with spinal degeneration.
Humans evolve slowly—over millennia. Yet, in just 20 years, we’ve shifted from keyboard-and-monitor posture to lap-held devices that trap our necks in flexion.
That shift is rapid, profound, and happening faster than our bones and muscles can hope to adapt.
Muscles: Design Mismatch
This phenomenon stems, in part, from the specific types of muscles we rely on for head and neck control. At the base of the skull lie small, deep muscles—like the suboccipitals and longus colli—whose job is to manage fine, reflexive head adjustments.
These muscles contain a high proportion of fast-twitch (Type II) fibers, which are designed for quick, precise bursts of activity, such as keeping the head stable while we scan a room or track moving objects with our eyes.[7,8]
In contrast, muscles like the quadriceps and spinal erectors are rich in slow-twitch (Type I) fibers—engineered for endurance and capable of supporting load over long periods.[7]
The mismatch becomes clear: we’re asking quick-reacting, precision muscles to act like endurance stabilizers. As these muscles fatigue, the body recruits larger muscle groups—like the upper trapezius and levator scapulae—to help.
But these muscles aren’t meant to stabilise the neck either, leading to
- tension
- tightness
- further imbalance[9]
Over time, this becomes a self-sustaining feedback loop: poor posture leads to muscle dysfunction, which reinforces poor posture.
It’s worth reflecting on the evolutionary context. Our bodies adapted over millennia to look straight ahead, scan the horizon, and make short, purposeful head movements.[10]
The modern lifestyle asks these same tissues to sustain a bent position for hours—every day—something that no prior generation had to endure. The structural toll is inevitable.
Clinical Manifestations: When Posture Turns Painful
Local Pain and Muscular Strain
Fatigue in neck muscles is more than soreness—it’s a subtle overload. The most common early signs of tech neck are localized discomfort — an ache at the base of the neck, tightness between the shoulder blades, or a creeping tension that settles in the upper trapezius.
These symptoms tend to build gradually, often mistaken for the effects of a long workday or poor sleep. Headaches, particularly tension-type or cervicogenic headaches, are also frequent.
They often begin at the occipital base and radiate toward the forehead or temples, a pattern strongly associated with strain in the suboccipital muscles and upper cervical joints.[11]
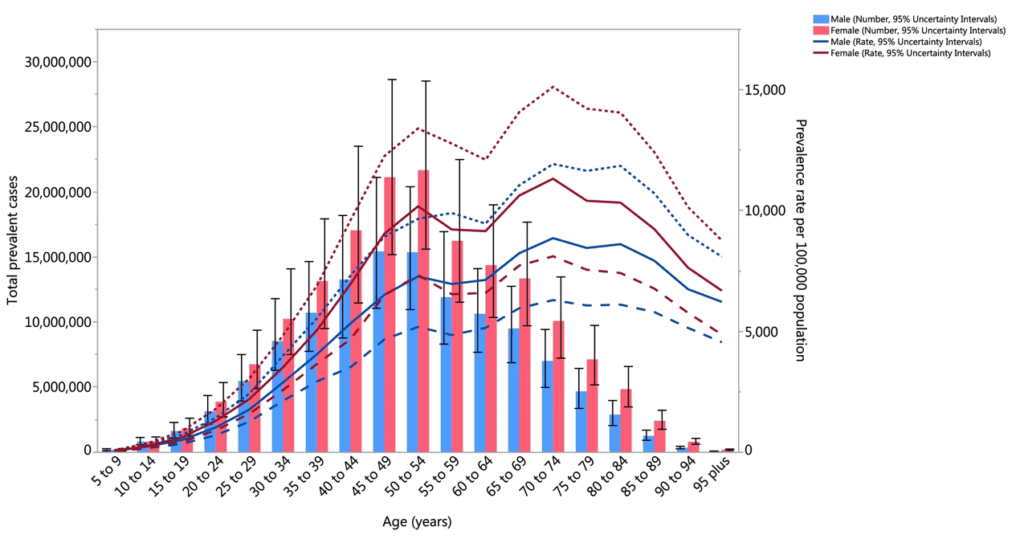
Dotted and dashed lines indicate 95% upper and lower uncertainty intervals, respectively. (Extracted from the study published by Safiri and colleagues).
For some, the pain remains mild and intermittent. For others, it becomes persistent—especially in people whose routines involve little variation in movement. A desk-based job, or student on a laptop, followed by hours of leisure screen time creates a near-continuous load on the same tissues.
When this cycle is repeated daily, the discomfort begins to set in earlier and resolve more slowly, if at all.
Radiating Symptoms and Fatigue
As symptoms progress, they may extend beyond the neck and shoulders. Numbness, tingling, or a dull ache in the arms or hands can occur when nerve roots become irritated or compressed, particularly in the lower cervical spine.[12]
These neurological symptoms often emerge in those who spend long periods in static positions with minimal movement or stretching throughout the day.
Another common complaint is fatigue—not just general tiredness, but a sense that the muscles in the upper back, shoulders, and neck are “worn out” by early afternoon. This isn’t fatigue in the athletic sense but rather a sign of muscular inefficiency.
As stabilisers become overworked and strained, they lose their endurance, and what used to be a passive task—like holding the head upright—starts to feel effortful.
Impaired Postural Stability
Some people with tech neck also experience subtle changes in balance and body awareness. These symptoms are rarely recognised for what they are and may show up as
- clumsiness
- poor posture during walking
- feeling “off-centre”
Research has shown that habitual forward head posture can disrupt the proprioceptive feedback loop between the cervical spine and postural control systems.[13]
In other words, the body begins to lose its ability to accurately sense and respond to changes in position. Although this doesn’t affect everyone, it appears more commonly in those with long-standing postural habits and may be exacerbated by concurrent inactivity or lack of exercise.
Daily Function and Quality of Life
While tech neck is often viewed as a musculoskeletal problem, its consequences ripple into daily life.
People report difficulty concentrating, irritability, and poor sleep — often driven by unrelieved pain, discomfort, or the mental fatigue of dealing with symptoms that don’t fully resolve.
In occupational settings, productivity can suffer, particularly in jobs that involve screen-based or seated work. Some individuals begin modifying their routines — not attending events, avoiding physical activity, or giving up hobbies that require movement or sustained attention — simply because they’re too uncomfortable to engage fully.
The sleep impact is particularly important. Disrupted sleep, whether from stiffness or nocturnal pain, makes recovery harder. It also lowers tolerance to pain, creating a cycle that amplifies both physical and psychological strain.
RELATED — Great Sleep means Great Health: 17 Health Benefits of Good Sleep
In adolescents and young adults, this combination of
- disrupted rest
- poor posture
- reduced physical activity
can have long-term implications for health and wellbeing.[14]
Asymptomatic Presentations and Early Changes
It’s important to note that pain isn’t always the first—or only—sign of a tech neck. Some people, especially younger users, may appear symptom-free, yet still demonstrate early functional changes.
These can include reduced muscular endurance, altered head positioning at rest, or proprioceptive delay. Left unchecked, these seemingly minor changes can develop into more disruptive symptoms over time, particularly as daily screen time increases and movement variability declines.
Unlike childhood diabetes, the physical impact of the tech neck won’t truly show the damage it’s done until the individual’s adult years, at which point recovery or reversal of the changes becomes difficult.
Early recognition, therefore, isn’t just about managing pain—it’s about identifying and addressing patterns before they become chronic and life changing.
Related Questions
1. How should I hold a phone or tablet to avoid tech neck?
Hold the device higher by bending your elbows and avoiding resting hands on your thighs.
Using a pillow under your arms (when convenient) can lift the screen further, reducing neck flexion and easing strain during screen use.
2. Can I reverse or undo the damage from Tech Neck?
In most cases, yes.
Physical therapy, posture retraining, and short daily use of a neck orthotic can help restore the curve. While not all symptoms may reverse, these steps can maintain function and prevent further damage.
References
(1) Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. 2014;25:277–279. PMID:25393825
(2) Neupane S, Ali U, Mathew A. Text neck syndrome–systematic review. Imperial J Interdiscip Res. 2017;3(7):141–148.
(3) Twenge JM, Spitzberg BH, Campbell WK. Less in-person social interaction with peers among US adolescents in the 21st century and links to loneliness. J Soc Pers Relatsh. 2019;36(6):1892–1913. doi:10.1177/0265407519836170
(4) Cho NH, Shaw JE, Karuranga S, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi:10.1016/j.diabres.2018.02.023
(5) Kamel M, Moustafa IM, Kim M, et al. Alterations in cervical nerve root function during different sitting positions in adults with and without forward head posture: A cross-sectional study. J Clin Med. 2023;12(5):1780. doi:10.3390/jcm12051780
(6) Kim SY, Jin YS, Lee JB, et al. The relationship between forward head posture and cervical disc degeneration. J Korean Neurosurg Soc. 2015;58(5):357–362. doi:10.3340/jkns.2015.58.5.357
(7) Schiaffino S, Reggiani C. Fibre types in mammalian skeletal muscles. Physiol Rev. 2011;91(4):1447–1531. doi:10.1152/physrev.00031.2010
(8) Larivière C, Nelson RT, Janjatovic IA. Fiber composition and fiber transformations in neck muscles of patients with cervical dysfunction. J Orthop Res. 1995;13(2):240–246. doi:10.1002/jor.1100130212
(9) Szeto GPY, Straker L, O’Sullivan PB. A comparison of symptomatic and asymptomatic office workers performing monotonous keyboard work—2: Neck and shoulder kinematics. Man Ther. 2005;10(4):281–291. doi:10.1016/j.math.2005.01.005
(10) Lieberman DE. Human head stabilization: Evolution, development, and biomechanics. In: Vinyard CJ, Ravosa MJ, Wall CE, eds. Primate Craniofacial Function and Biology. Boston, MA: Springer; 2008:417–435. doi:10.1007/978-0-387-74527-3_17
(11) Fernández-de-las-Peñas C, Cuadrado ML, Arendt-Nielsen L, et al. Myofascial trigger points and sensitization: An updated pain model for tension-type headache. Cephalalgia. 2007;27(5):383–393. doi:10.1111/j.1468-2982.2007.01303.x
(12) Zarei M, Pourahmad S, Jalali M, et al. The effect of forward head posture on nerve root function and cervical mechanosensitivity: A cross-sectional study. J Manipulative Physiol Ther. 2021;44(5):349–356. doi:10.1016/j.jmpt.2020.11.008
(13) Quek J, Pua YH, Clark RA, et al. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man Ther. 2013;18(1):65–71. doi:10.1016/j.math.2012.07.005
(14) Finan PH, Goodin BR, Smith MT. The association of sleep and pain: An update and a path forward. J Pain. 2013;14(12):1539–1552. doi:10.1016/j.jpain.2013.08.007






