
Joyce Roberts
BHSc Nsg, Post Grad Cert Adv Nsg, Post Grad Dip Adv Nsg, Accredited Diabetes Nurse Specialist
Diabetes is a complex, chronic disease requiring continuous medical care with risk reduction strategies to aid in preventing and minimizing health complications.
The risk factors that affect development of complications are
- Length of time the person has had diabetes
- Genetic susceptibility
People with Type 1 or Type 2 diabetes have the same chances of developing long-term complications
Chronic complications of diabetes include
- Microvascular disease (microangiopathy or small vessel diseases)
- Macrovascular disease (coronary artery disease, stroke and peripheral vascular diseases)[1,2]
In this article, we will discuss in more detail about different microvascular diseases and possible health risks and complications.
Before we continue, important to note is that not everyone who has developed diabetes will develop other health complications.
What are microvascular diseases?
Microvascular diseases include retinopathy, nephropathy, and diabetic and autonomic neuropathy.
The central mechanism of microvascular diseases appears to be related to sorbitol (sugar alcohol which can be obtained by the reduction of glucose).
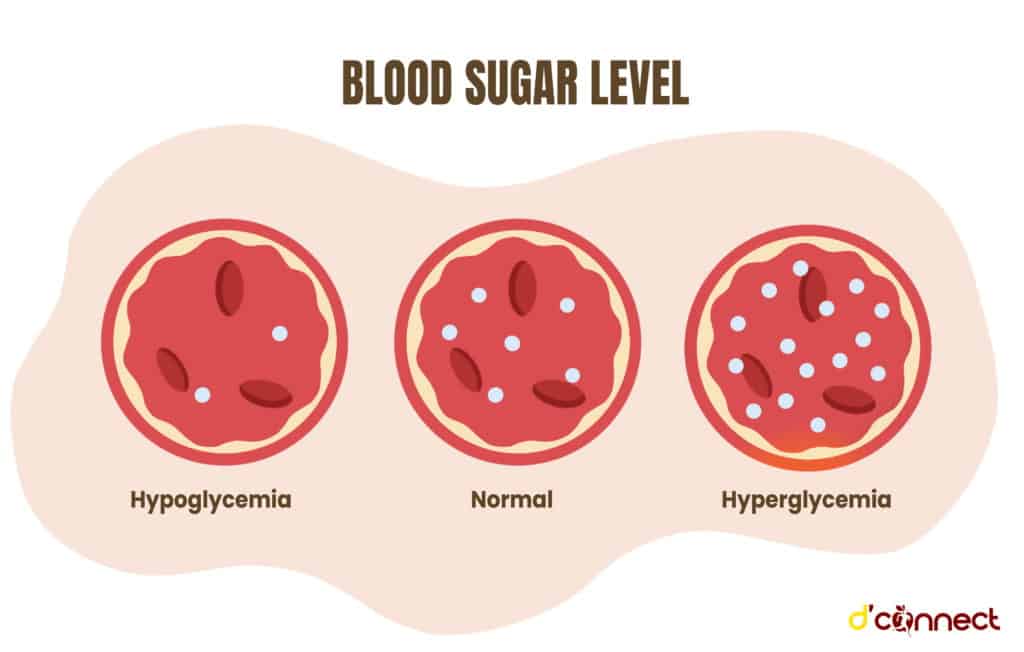
Hyperglycemia (high blood sugar) leads to increased accumulation of sorbitol which does not easily cross cell membranes, and this directly damages the proteins in the vessel walls, creating other issues and health complications.[3]
Diabetes and nephropathy - kidney disease
In New Zealand, diabetes is the leading cause of end stage renal failure.
Kidneys act as a filtering system. They clean our blood by removing water and waste from our body. Each of the kidneys contains up to one million nephrons, which are the filtering units.
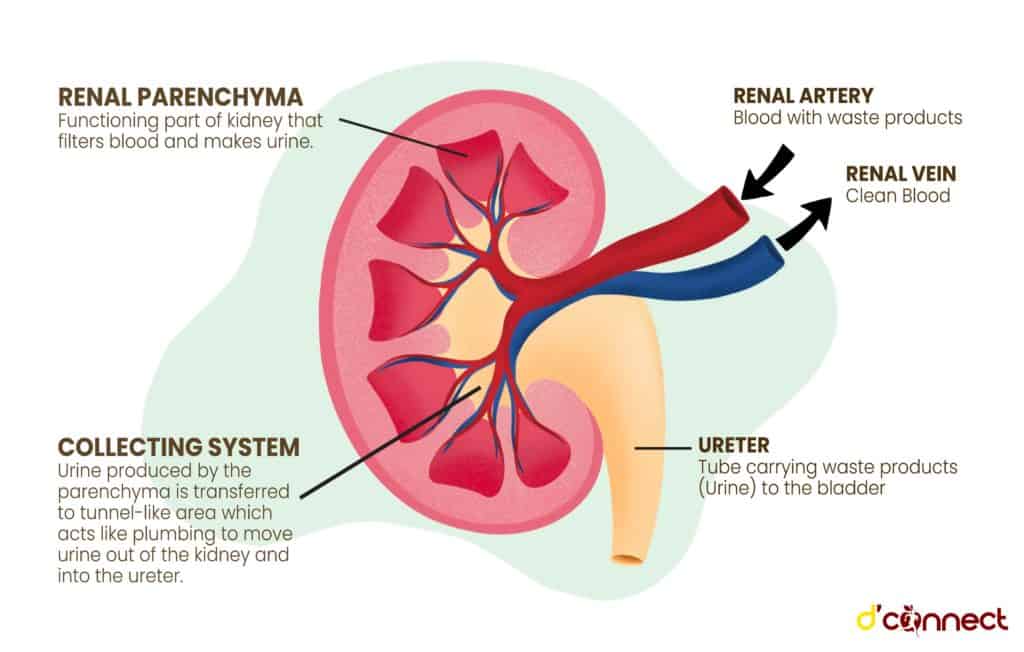
Inside a nephron is a tiny set of looping blood vessels called the glomerulus. Diabetes damages these filtering membranes, reducing their capacity.
One in three people with diabetes will have kidney damage
Once enough of the filters have been damaged the body will fill up with excess water and wastes.[4]
Diabetic nephropathy is characterized by
- Presence of protein in the urine
- Lesions on the glomerulus
- Loss of glomerular filtration
The presence of protein in the urine can indicate the extent of damage to the kidneys’ filters.
Diabetes and retinopathy - disease of the retina
The retina is the thin, light-sensitive membrane that covers the back of the eye. Our sense of vision is produced by the energy being conveyed to our brain via retinal cells, the optic nerve and the visual nerve pathways.
Diabetic retinopathy appears to be caused by retinal ischemia, or lack of blood to the retina. In turn, ischemia is caused by changes in the blood vessels and aggregation of red blood cells.[5]
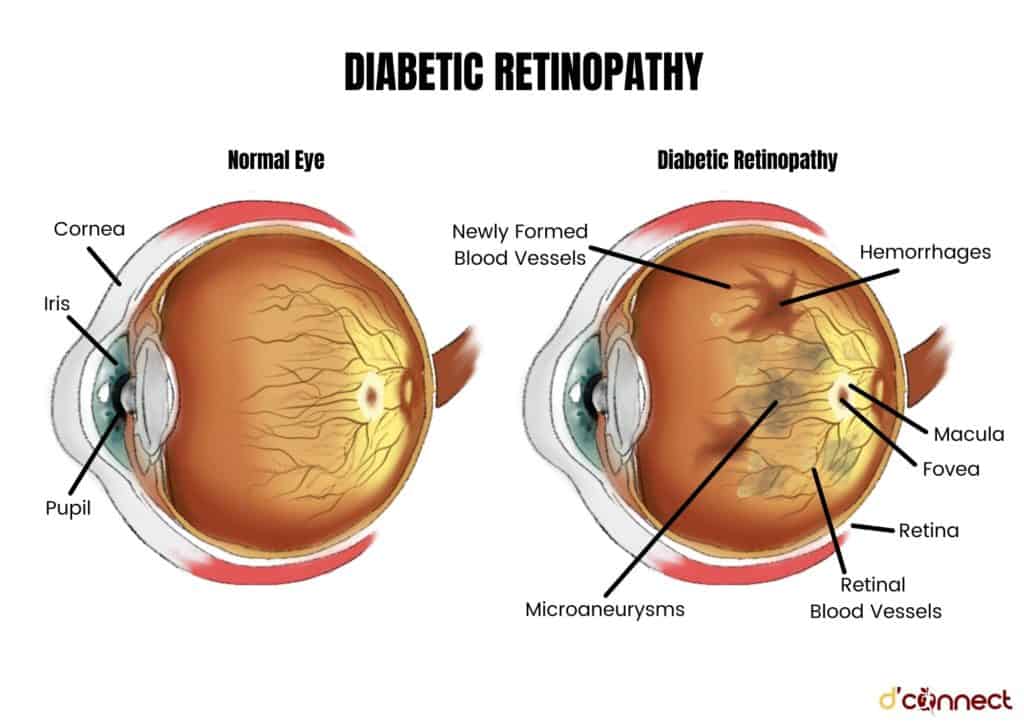
The longer the person has diabetes, the more likely they are to develop retinopathy.
Two common forms of retinopathy are non-proliferative (early stage with mild symptoms) and proliferative (advanced stage with possible loss of vision).
Diabetes and maculopathy - macular degeneration of the eye
Maculopathy is another eye health condition that can result from retinopathy.
The part of the eye which provides us with our central vision is called the macula.
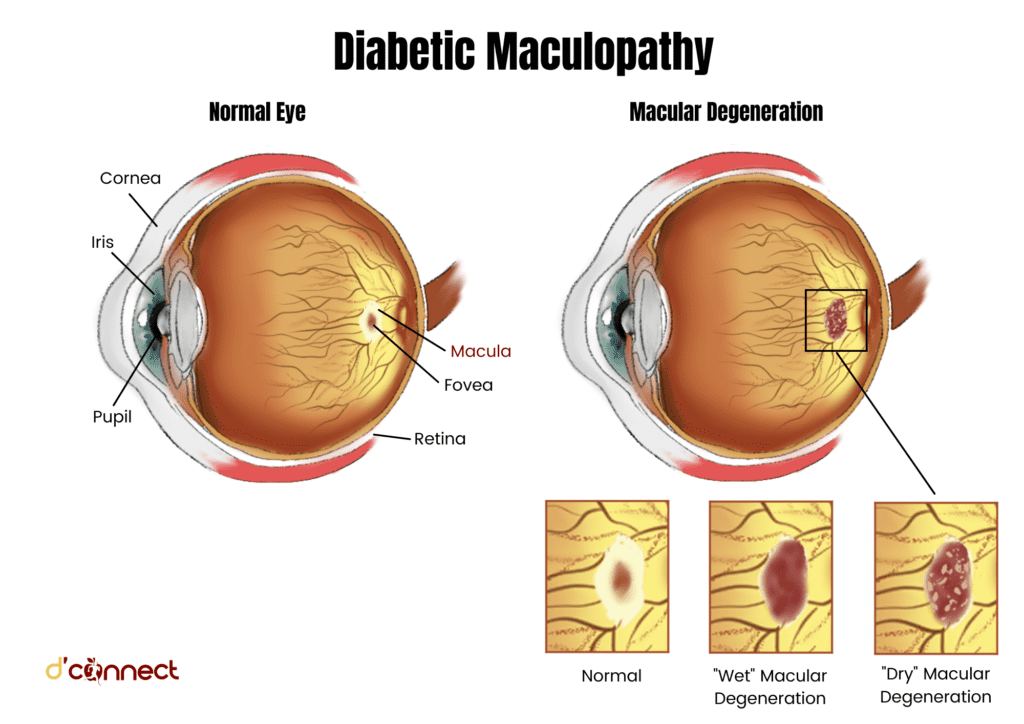
Damage to the macula occurs from blocked vessels that have become leaky due to enlargement. Fluid has built up at the macula which then leaks into the retina.
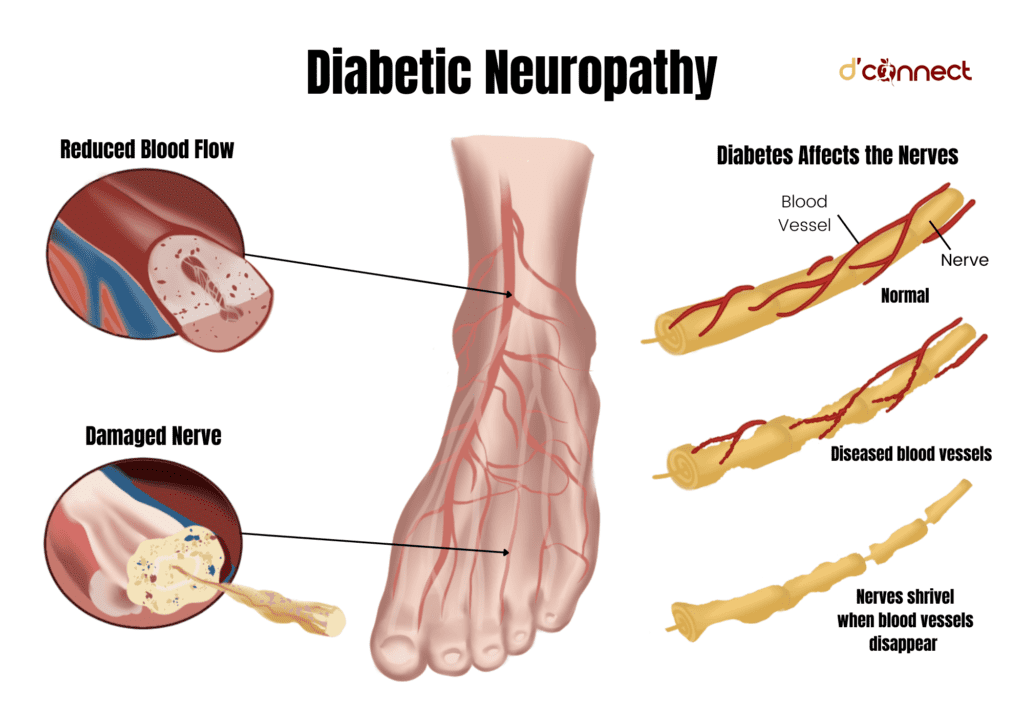
Diabetes and neuropathy - damage of the nerves
Neuropathy is the medical term for describing diseases affecting mostly the peripheral nerves.
Peripheral nerves are responsible for connecting the brain and spinal cord to muscles and to sensory cells. These sensory cells detect sensations such as
- Touch / Pressure
- Pain
- Heat / Cold
- Sound
Our nerves are vulnerable to the effects of hyperglycemia
Diabetic neuropathy is defined as the presence of symptoms and/or signs of peripheral nerve dysfunction and is often a late health complication due to damage caused by diabetes.
Diabetic neuropathies can be classified into 4 key types:
- Hyperglycaemic
- Peripheral or sensorimotor
- Mononeuropathies (focal)
- Autonomic
Diabetic neuropathies are the most common complications of diabetes.
Hyperglycaemic neuropathy
Hyperglycaemic neuropathy is the tingling and pain commonly felt in the feet due to the slowing of the nerve conductors. It resolves itself with the return to good glycemic control / blood sugar levels.
Sensorimotor neuropathy
Sensorimotor neuropathy refers to a peripheral neuropathy that damages the motor nerves which control muscles, and the sensory nerves which carry touch, temperature, pain and pressure information from the body to the brain.
The most common symptoms of sensorimotor neuropathy are
- Burning pain
- Electrical or stabbing sensations
- Paresthesia (commonly felt in the feet and lower limbs)
Due to minimal or lack of sensation, it is not uncommon for the person with diabetes to have an active foot ulcer without being aware of it.
Mononeuropathy
Mononeuropathy can occur as a result of nerve damage due to diabetes, as well as compressed or trapped nerves.
Common nerves involved are
- Median
- Ulnar
- Radial
- Peroneal.
The entrapment of these nerves results in developing either a wrist drop or a foot drop.[6]
Autonomic neuropathy
Autonomic neuropathy occurs due to damage to the sympathetic and parasympathetic nerves and it affects multiple nerves including
- Gastrointestinal enteric
- Genitourinary tract
- Sudomotor
- Cardiovascular[7]
Autonomic neuropathy can be one of the early signs of serious diabetes complications
The manifestations of autonomic neuropathy are numerous and include postural hypotension, gastroparesis, neurogenic bladder, and silent myocardial infarct to name a few.
Diabetic gastroparesis
Diabetic gastroparesis is characterized by delayed gastric emptying of solid food in the absence of a mechanical obstruction of the stomach. It is mostly a result of ongoing poor glycaemic control and is more common in Type 1 diabetes.
Postural hypotension
Postural hypotension is a lower than normal blood pressure defined as a fall in blood pressure of 20/10mmHg on standing for three minutes.
When a person with diabetes is standing, the buildup of blood in their legs causes the blood pressure to decrease as there is less blood circulating back to their heart.
The body naturally counteracts this by increasing the heart rate, so that more blood is pumped around the body to stabilize the blood pressure.[8]
If you are interested in reading second part of the article, you can find it here – Diabetes untreated (Part 2).
Related Questions
1. What is HbA1C?
The HbA1c is measuring our average blood glucose control over the preceding 8-12 weeks.
HbA1c or A1c is a variant of haemoglobin HbA. It’s formed during glycosylation, the process of glucose binding with HbA, and it is the only marker used to test the blood-glucose control of a person with diabetes.
2. What is a normal blood sugar level?
For a person who does not have diabetes, the recommended range is between 4.0mmol/l – 9mmol/l.
For a person who has Type 2 diabetes it is recommended that you aim to stay
- between 4.0mmol/l – 7mmol/l before meals
- under 8.5mmol/l after meals.
For a person who has Type 1 diabetes it is recommended that you aim to stay
- between 4.0mmol/l – 7mmol/l before meals
- under 5.0mmol/l – 9mmol/l after meals
providing it is safe for you to do so as an individual.
3. What is Diabetes Insipidus?
Diabetes insipidus is a disorder of salt and water metabolism and a completely separate condition from diabetes.
Diabetes insipidus can be found in two forms
- Neurogenic / central
- Nephrogenic / renal
Diabetes insipidus is caused by a deficiency of the antidiuretic hormone (ADH). This deficiency causes a person to pass too much urine which then leads to excessive thirst and fluid intake.
For more similar articles, please see our page on Health Conditions. Also, you might be interested in our previous article on Diabetes – Early Signs, Causes, Types and Treatment.
Joyce has been nursing since the 1980s, and for the past 20 years she has been focusing on patients with diabetes.
Given that diabetes can be a debilitating disease if not managed properly, Joyce’s focus is to ensure that individuals with diabetes have all the correct information. She works diligently and her focus is to prepare, inform and make sure that the individuals are well equipped with knowledge and support to live with the disease 24 hours a day.
References
(1) King, P. (1999) The UK Prospective Diabetes Study (UKPDS): clinical and therapeutic implications for Type 2 diabetes. Journal Clinical Pharmacology. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2014359/
(2) Fowler,M. (2008). Microvascular and Macrovascular Complications of Diabetes. Clinical Diabetes. Retrieved from https://www.researchgate.net/publication/244935925_Microvascular_and_Macrovascular_Complications_of_Diabetes
(3) McDowell, J. (2007) Diabetes: a handbook for the primary healthcare team.
(4) American Diabetes Association. (2021) Chronic Kidney Disease and Type 2 Diabetes. Retrieved from https://professional.diabetes.org/sites/professional.diabetes.org/files/media/ckd_compendium_fin_2_web.pdf
(5) Diabetes NZ. Eyes – complications. Retrieved from https://www.diabetes.org.nz/complication-eyes
(6) McCance, K. (2010) Pathophysiology: The Biologic Basis for Disease in Adults and Children.
(7) National Institute of Diabetes and Digestive and Kidney Diseases. Autonomic Neuropathy. Retrieved from https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/nerve-damage-diabetic-neuropathies/autonomic-neuropathy
(8) Diabetes UK. Postural Hypotension (2019). Retrieved from https://www.diabetes.co.uk/diabetes-complications/postural-hypotension.html






