
Daniel Moore
(DO., MSc Pain Management)
Note — The article was checked and updated May 2023.
Having the ability to freely move is one of the greatest feelings in life. Many of us remember the joy of play, running and being active for hours on end when we were younger.
Today, our lives are in stark contrast – we barely move around, with research saying that we are physically active less than 15 minutes a day. This comes at a price.
Our range of movement and flexibility suffer, which reduces circulation and nutrient supply to many areas of our body, which in the long term will cause health issues.
That is why understanding how osteopathy can assist us with keeping our body healthy and diagnose, treat and prevent illnesses is important so we know how we can include it in our healthy lifestyle and routine.
What is osteopathy and how does it work?
Osteopathy is a continually evolving medical discipline that helps people make use of their natural healing capabilities and innate recovery mechanisms to create better wellness and overcome health challenges.[1,2]
It is based on four key holistic principles:
- The body is an integrated system, and a person is a unit of body, mind and spirit.
- The body is capable of self-regulation, self-healing and health maintenance.
- Structure (anatomy) and function (physiology) are reciprocally interrelated.
- Rational treatment is based upon an understanding of the basic principles of body unity, self-regulation and the interrelationship of structure and function.[3]
There are two classifications of osteopathy:
- osteopathic medicine
- osteopathic manual therapy
Both are based on the same core principles, but they differ in some important ways.
Practitioners of osteopathic medicine are qualified medical doctors and though they may use manual therapy techniques, they also prescribe drugs and perform surgery.[4] This type of osteopathy is only taught and practiced in the USA.
Practitioners of osteopathic manual therapy are typically known as osteopaths.[5] They only use manual therapy techniques to affect the body, such as:
- Massage
- Stretching
- Mobilization
- Manipulation
This type of osteopathy is taught and practiced in over 40 other countries worldwide.[6]
Osteopaths also provide lifestyle advice to support people’s health goals
There are two subsets of osteopathic manual therapy – cranial osteopathy and visceral osteopathy.
Cranial osteopathy aims to influence cerebrospinal fluid by applying a soft touch to the skull and other parts of the body while visceral osteopathy uses manual techniques to influence the body’s organs.[7,8]
History of osteopathy
Osteopathy was officially founded in 1874, in Kirksville Missouri, by physician Andrew Tayor Still, and his original inspiration for osteopathy can be traced back to a headache.[9]
When he was 10 years old, Still developed a severe headache and in an attempt to distract himself from the pain, he made himself a low-hanging rope swing. He put a blanket on it and laid down with his neck across the rope.
Later, Still acknowledged this as his first discovery in the science of osteopathy.[10]
Following in his father’s footsteps, Still became a preacher. He also studied engineering and eventually trained as a physician.
Although he studied medicine, Still did not like using drugs on patients. In those days, the drugs used were crude, often given in high doses, and could be extremely dangerous. For example, it was common to purge the body with mercury and to give opium-based drugs for many kinds of conditions.[11]
After spinal meningitis caused the death of his wife and three children, Still became disillusioned with the medicine of his day and devoted 10 years of his life to finding a better way to treat illnesses.
Inspired by his engineering background, Still concluded in 1874 that the body was like a machine and if all the parts of that machine were in proper relationships with each other, it would function at an optimal level. This marked the birth of the science of osteopathy.[12]
When Still announced his ideas to the medical profession, he was ridiculed and from that point onward was unable to get paid work as a doctor in his hometown. Undeterred, Still moved with his children and a new wife to Kirksville Missouri and started treating people for free using his newly developed techniques.
His patients got better, the word soon spread and people flocked to see him from all over the country.
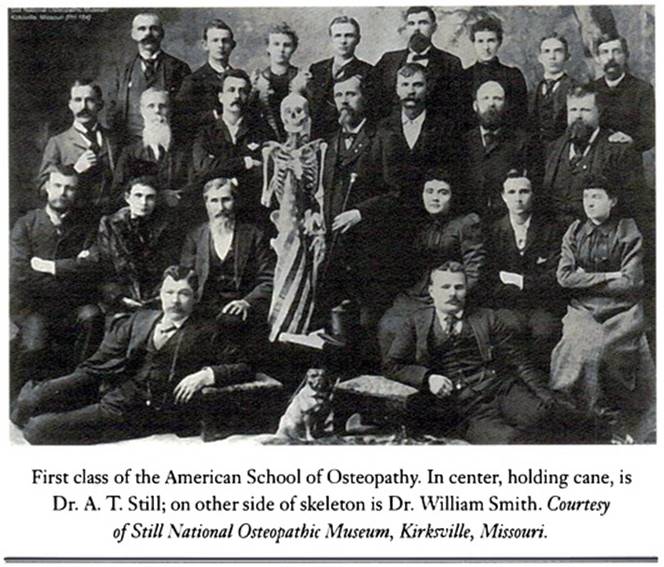
Eventually, the demand for his services became so great, Still could not cope, so he opened the first osteopathy school. Over time, many schools of osteopathy were set up across America.
One of Still’s first students was J Martin Littlejohn, who founded the first school of osteopathy in Europe in 1917.
By 1930, osteopathy had reached New Zealand, and by 2020, nearly 200,000 clinicians were delivering osteopathic care in 46 countries worldwide.[13]
How effective is osteopathy - what does research say
Numerous studies have been conducted over the years that demonstrate osteopathic management has been effective in treating both acute (new onset) and chronic (ongoing) spinal pain.[14,15]
Clinical trials examining the use of osteopathy for headaches and migraine showed that it resulted in lower pain intensity and a reduction in the use of medication.[16,17]
Also, research confirmed the effectiveness of osteopathic treatment as an effective way of managing:
- musculoskeletal conditions
- non-musculoskeletal conditions (irritable bowel syndrome, constipation, diarrhoea).[18]
What are the health benefits of osteopathy?
Osteopaths do not treat medical conditions; instead, they work with people who may or may not have a medical condition.
To find health should be the object of the practitioner. Anyone can find disease.
―Andrew Tayor Still
Osteopathy provides personalized healthcare that takes into account the individuality of the patient, such as:
- who they are
- what they want
- what they need
- what would be best for them given their current situation.
This means that in addition to treating the person physically, the osteopath will also aim to address what is going on in their lives psychologically and socially.
Improved movement and flexibility
When a person becomes unwell or gets injured, muscles can become tight and joints stiff, and movement can become difficult.
Osteopathy uses a combination of hands-on techniques and individually tailored exercises designed to restore range and quality of movement. Many patients report that after osteopathic treatment, they feel looser and generally more comfortable in their bodies.
Pain reduction
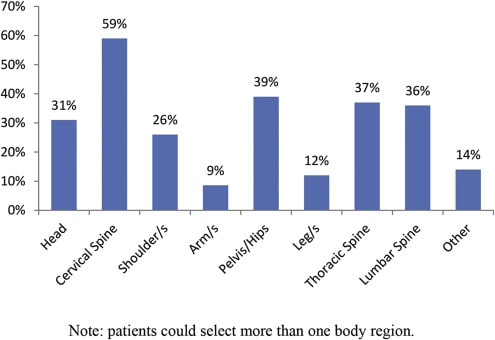
Pain reduction is the main reason why people seek help from osteopaths.
In addition to hands-on techniques, many osteopaths use other approaches such as exercise prescription, breathing techniques, relaxation, mindfulness, graded motor imagery (GMI) and acceptance and commitment therapy (ACT).
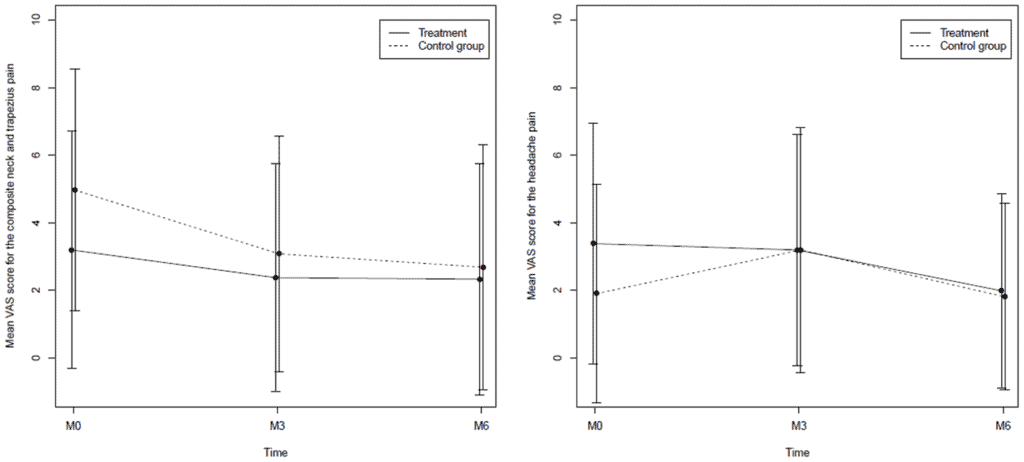
Source: Hubert, D. Impact of Osteopathic Treatment on Pain in Adult Patients with Cystic Fibrosis – A Pilot Randomized Controlled Study. (2014)
Increase in energy levels
Being in pain and having tension in the musculoskeletal system can be physically and mentally draining. A welcome bonus that goes with resolving these problems is that in a number of cases, the person’s energy will improve, and this will help motivate them to get more active and start exercising again, which will in turn help their energy levels to gradually pick up.
Improved quality of sleep
Although it’s uncommon for a patient to seek osteopathy as a primary treatment for sleep disorders, it is not uncommon for osteopathic patients to report that their sleep has improved.
Osteopathic treatment aims to reduce muscular tension, and this can result in improved sleep. Many osteopaths will also teach stress management and relaxation techniques that can further enhance sleep.
RELATED — Why we sleep: The role of sleep in our healthy life
Stress reduction
Stress and pain can make one another worse, creating a perpetuating loop, such as increasing one’s blood pressure. Osteopaths will look for evidence of stress and work with the patient to bring it down, or they may refer the patient for additional specialist help.
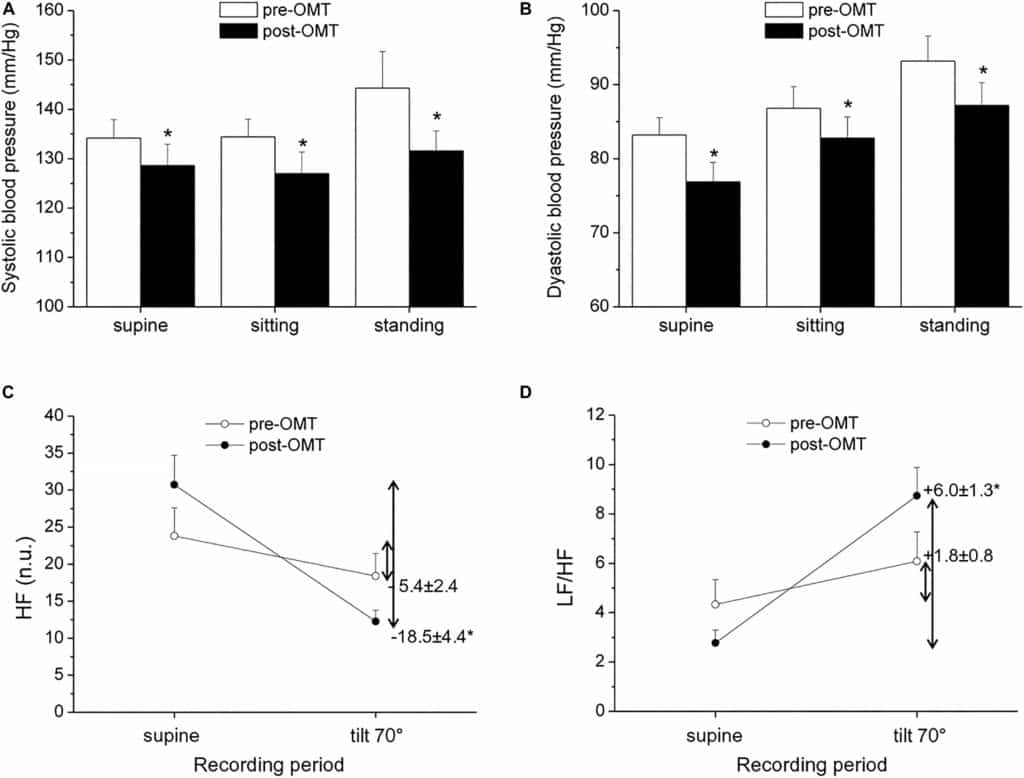
Source: Lombardi, L. Exploring the Effects of Osteopathic Manipulative Treatment on Autonomic Function Through the Lens of Heart Rate Variability. (2020)
Improvement in poise and posture
Osteopaths are keen to help patients optimize their poise and posture.
This can have a number of benefits, including feeling more comfortable, having a sense of increased confidence, feeling more attractive and having less strain on the body.
Which conditions can osteopathy help with?
Osteopathy can support a person who may be suffering from almost any health condition, but in this article we will focus on the most common conditions an osteopath treats.
Back pain
Back pain is one of the most common conditions that cause people to seek medical help.[19]
Most back pain, although very uncomfortable, is not usually serious and only a small number of cases (1–3%) are related to urgent medical conditions.[20,21]
The most common back pain is called non-specific back pain

This condition has no clear medical cause such as inflammation, injury, infection or disease.
However, because of the way osteopaths assess patients, they will often find mechanical issues that may be the cause of the pain, such as:
- excessive muscle tension
- poor alignment of joints
- poor posture
that affect the blood flow and circulation.[22] Osteopathy is also used to treat acute (sudden onset) back pain.[23]
Neck pain
Neck pain is another very common condition but is rarely a serious medical issue and is usually very responsive to treatment.[24]
Neck pain can also be a cause of many types of headaches
This means that in addition to treating neck pain, osteopathy can also help to address many types of headaches.[25]
Joint pain (shoulder, elbow, knee)
Joints often get injured due to sporting activity or even just everyday life. Sometimes joints can become painful for no apparent reason: frozen shoulder, for example, is a painful condition in which the capsule of the shoulder joint becomes inflamed and causes restriction of movement and pain.[26]
Osteopaths can treat many joint conditions like
- frozen shoulder
- tennis elbow
- carpal tunnel syndrome
- knee and ankle injuries
and even joints that have become painful due to arthritic changes.[27]
Sciatica
Sciatica is a neuropathic (nerve-based) pain condition that can last for months or even years.
In the old days, it was mostly attributed to bulging discs, but now we know it can be caused by other factors such as a tight piriformis (a deep muscle in gluteus) that can press into the nerve.[28]

Some of the other conditions that osteopathy may be able to help with are:
- Arthritis
- Scoliosis
- Stress and tension in the body
- Irritable bowel syndrome
- Unexplained pain
- Back pain in pregnancy
Osteopaths will work on the muscles to help reduce tension and release the compression of the nerve and may also do some manipulation and adjustment to the lower back and pelvis to help create better and less stressful alignment of joints.
What are the risks of osteopathy?
Every medical procedure carries some risk of harm. The risks associated with manual therapy and osteopathy are very small.[29,30] We have listed below some of the most common ones.
Pain after the session
The most common risk is increased pain following treatment, which can affect up to 20% osteopathic patients.[31]
This reaction is often called a treatment reaction and usually lasts for 24 hours or less. Also, most people who experience it report they feel better than they did before the treatment started.
Possibility of a stroke
The most serious risk associated with manual therapy is damage caused to the vertebral artery by high-velocity neck manipulation (cracking the neck joints).
If the vertebral artery becomes damaged during neck manipulation, it can result in a brain hemorrhage, stroke or in rare and extreme cases, death.
Research suggests that somewhere between 1 in every 100,000 and 1 in every million neck manipulations could lead to some kind of serious adverse effect.
To put this into perspective, death from neck surgery has been reported to occur in around 1 in every 145 cases.[32]
About risk factors
These risk factors apply to all forms of manual treatment, not just osteopathy. The key to minimizing risks is to take a thorough medical history and perform a full examination.
Typically, if this is done properly, the risk factors mentioned above will be identified, and the patient would not be given a treatment that would be likely to cause an unwanted response.
Related Questions
1. What should I expect during my first osteopathic session?
The osteopath will begin with an assessment of your medical history, general health and the issue you want help with.
Then they will conduct a physical examination to assess how your body is functioning and assess tissue damage, strength, coordination and nerve conduction. Afterwards, assuming there is enough time left, the osteopath will begin treatment.
2. What does treatment involve?
Treatment may include hands-on techniques like massage, mobilization, manipulation and stretching.
RELATED — Introduction to massage: Holistic medicine and antidote to stress
3. How many osteopathic sessions are usually needed?
Most patients get some improvement after 3–5 sessions.
There are many factors that can affect the treatment and recovery, such as the type of problem, how long it has been present, age, fitness and stress levels, and whether other medical conditions are involved (i.e., diabetes).
4. Should I rest after an osteopathic session?
Usually you can go about business after osteopathic treatment.
If you have just finished your first visit, you may feel tired afterwards. Also, if the problem you are being treated for was damaged-tissue related, then you may be asked to take it easy until the tissues repair.
Disclaimer
Every patient and presenting case is different and while some people may find osteopathy helpful, others with the same condition may find it offers them no benefit at all. In order to find out if osteopathy could help you, you would need to discuss your individual case with an osteopath and your GP.
Are there any pains and aches that you are experiencing and are wondering what to do about them? Would this be from exercise or lack of movement? If it’s the latter, it might be wise to check with your GP or osteopath, and you can let us know in the comments how your first session went.
Daniel found his way into osteopathy through dance, after incurring a serious knee injury, while pursuing his career of becoming a contemporary dancer. Being introduced to an osteopath, who not only helped him to recover from the injury but also inspired him to change his career direction, Daniel decided that osteopathy would become his calling, and he’s been a practicing osteopath since 1989…
If you would like to learn more about Daniel, see Expert: Daniel Moore.
References
(1) Smith, D. (2019). Reflecting on new models for osteopathy – it’s time for change. International Journal of Osteopathic Medicine, 31, 15–20. Retrieved from https://doi.org/10.1016/j.ijosm.2018.10.001
(2) AOA. (2022). 2020-21 report tracks increased growth in the osteopathic profession. Retrieved from https://doi.org/https://osteopathic.org/about/aoa-statistics/
(3) Paulus, S. (2013). The core principles of osteopathic philosophy. International Journal of Osteopathic Medicine, 16(1), 11–16. Retrieved from https://doi.org/10.1016/j.ijosm.2012.08.003
(4) American Osteopathic Association. (2022) What is osteopathic medicine? Retrieved from https://osteopathic.org/what-is-osteopathic-medicine/
(5) NHS. (n.d.). NHS England: The 14 allied health professions. Retrieved from https://www.england.nhs.uk/ahp/role/
(6) Alliance, O. (2020). Osteopathic healthcare: Global review of osteopathic medicine and osteopathy 2020. Retrieved from https://oialliance.org/wp-content/uploads/2021/02/OIA_Report_2020_FINAL_Summary.pdf
(7) Osteopath SCCO. (n.d.). What is cranial osteopathy? Retrieved from https://scco.ac/osteopathy/what-is-cranial-osteopathy/
(8) TDUK. (n.d.). Visceral osteopathy: What is it, symptoms and treatment. Retrieved from https://doi.org/https://www.topdoctors.co.uk/medical-dictionary/visceral-osteopathy
(9) Institute of Osteopathy. (n.d.). History of osteopathy. Retrieved from https://www.iosteopathy.org
(10) Still A. T. (1908). Autobiography of Andrew Taylor Still. Retrieved from https://archive.lib.msu.edu/DMC/Osteopathy/autobiographystill1908.pdf
(11) Kang, L., & Pedersen, N. (2017). Quackery: A brief history of the worst ways to cure everything. Workman Publishing.
(12) Western University of Health Sciences. (n.d.). Osteopathic philosophy. Retrieved from https://www.westernu.edu/osteopathic/about/osteopathic-philosophy/
(13) Pollock, K. (2018). Chiropractic, osteopathy and massage. InTe Ara – Encyclopedia of New Zealand. Retrieved from https://teara.govt.nz/en/alternative-health-therapies/page-2
(14) Cruser, D. A., Maurer, D., Hensel, K., Brown, S. K., White, K., & Stoll, S. T. (2012). A randomised, controlled trial of osteopathic manipulative treatment for acute low back pain in active duty military personnel. Journal of Manual & Manipulative Therapy, 20(1), 5–15. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3267441
(15) Lafans, K., & Troncoso, V. (2021). Osteopathic manipulative treatment: Muscle energy procedure: lumbar vertebrae. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK564342
(16) Burch, R,. Rizzoli, P., & Loder, E. (2021). The prevalence and impact of migraine and severe headache in the United States: Updated age, sex, and socioeconomic-specific estimates from government health surveys. Headache, 61(1), 60c–68. Retrieved from https://doi.org/10.1111/head.14024
(17) Whalen, J., Yao, S., Leder, A. (2018). A short review of the treatment of headaches using osteopathic manipulative treatment. Current Pain and Headache Reports, 22(12), 82. Retrieved from https://doi.org/10.1007/s11916-018-0736-y
(18) Müller, A., Franke, H., Resch, K.-L., & Fryer, G. (2014). Effectiveness of osteopathic manipulative therapy for managing symptoms of irritable bowel syndrome: A systematic review. Journal of Osteopathic Medicine, 114(6), 470–479. Retrieved from https://doi.org/10.7556/jaoa.2014.098/html
(19) Wu, A., March, L., Zheng, X ., Huang, J., Wang, X., Zhao, J., Blyth, F. M., Smith, E., Buchbinder, R., & Hoy, D. (2020). Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Annals of Translational Medicine, 8(6), 299. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32355743
(20) Henschke, N., Ostelo, R. W., Van Tulder, M. W., Vlaeyen, J. W., Morley, S., Assendelft, W. J., & Main, C. J. (2010). Behavioural treatment for chronic low‐back pain. Cochrane Database of Systematic Reviews , 2010(7), CD002014.
(21) Ingram, J. (2022, September 20). Complete guide to low back pain: An extremely detailed guide to the myths, controversies, and treatment options for low back pain. Retrieved from https://www.painscience.com/tutorials/low-back-pain.php
(22) Grace, S., Orrock, P., Vaughan, B., Blaich, R., & Coutts, R. (2016). Understanding clinical reasoning in osteopathy: a qualitative research approach. Chiropractic & Manual Therapies, 24(1), 1-10. Retrieved from https://chiromt.biomedcentral.com/articles/10.1186/s12998-016-0087-x
(23) Cruser, D. A., Maurer, D., Hensel, K., Brown, S. K., White, K., & Stoll, S. T. (2012). A randomized, controlled trial of osteopathic manipulative treatment for acute low back pain in active duty military personnel. Journal of manual & manipulative therapy, 20(1), 5–15. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3267441
(24) Hoy, D. G., Protani, M., De, R., & Buchbinder, R. (2010). The epidemiology of neck pain. Best Practice & Research Clinical Rheumatology, 24(6), 783–792. Retrieved from https://doi.org/10.1016/j.berh.2011.01.019
(25) Cerritelli, F., Lacorte, E., Ruffini, N., & Vanacore, N. (2017). Osteopathy for primary headache patients: A systematic review. Journal of pain research, 10, 601. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5359118
(26) McKone, W. L. (2013). Osteopathic athletic health care: Principles and practice. Springer.
(27) DiGiovanna, E. L., Schiowitz, S., & Dowling, D. J. (2005). An osteopathic approach to diagnosis and treatment. LWW.
(28) Pande, A., Gopinath, R., Ali, S., Adithyan, R., Pandian, S., & Ghosh, S. (2021). Piriformis syndrome and variants: A comprehensive review on diagnosis and treatment. Journal of Spinal Surgery, 8(4), 7–7.
(29) Carnes, D., Mars, T. S., Mullinger, B., Froud, R., & Underwood, M. (2010). Adverse events and manual therapy: a systematic review. Manual Therapy, 15(4), 355–363. Retrieved from https://www.sciencedirect.com/science/article/pii/S1356689X09002112
(30) Hu, J. (2015). Potential risks and side effects of osteopathic manual therapy. Retrieved from https://nationalacademyofosteopathy.com/wp-content/uploads/2019/12/Potential-Risks-and-Side-Effects-of-Osteopathic-Manual-Therapy.pdf
(31) Degenhardt, B. F., Johnson, J. C., Brooks, W. J., & Norman, L. (2018). Characterizing adverse events reported immediately after osteopathic manipulative treatment. Journal of Osteopathic Medicine, 118(3), 141–149. Retrieved from https://doi.org/10.7556/jaoa.2018.033/html?lang=en
(32) National Council for Osteopathic Research[NCFO]. (n.d.). Risks of osteopathic treatment. Retrieved from https://www.ncor.org.uk/practitioners/practitioner-information-communicating-benefit-and-risk-in-osteopathy/risk-and-patient-incidents/#question4






