Anishka Ram
(NZRD, MSc. Nutrition and Dietetics)
For the newest articles on coeliac disease, we suggest to start with Coeliac Disease: Symptoms and Effects on our health and body, which is the first article in a 3-part series.
There are several medications currently in clinical trials and testing such as Budesonide, Larazotide acetate, Prolyl Endopeptidases (PEP), Latiglutinase and Nexvax2, but they are yet to be approved for human use.
The best treatment currently for managing Coeliac Disease is a gluten-free diet, ensuring that there is no food cross-contamination.
However, Kivela’s study (2021) cited that although you might be doing everything in your power to reduce exposure and cross-contamination of gluten, it may not be enough.[1]
This is because the chances of accidentally consuming gluten are high and it can still lead to the small intestine’s lining being damaged in up to 60% of individuals.[1]
How the Gluten-Free Diet began
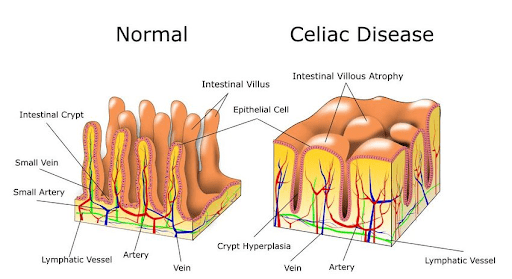
Patients with coeliac disease were showing signs of discomfort, stomach pain and a few other key symptoms after eating which led to specialists taking biopsies and scans of the small intestine.
They concluded that the villi found in the lining of the small intestine were damaged and could not continue its function of sorting out what can enter and exit the gut. This is also known as intestinal permeability.
The patients were told to follow a gluten-free diet, and practice food safety when preparing meals to avoid cross-contamination of gluten-containing foods with gluten-free foods.
When the specialists then performed another biopsy and scan they found that the villi in the small intestine grew again, as opposed to being blunt, and the entire lining almost returned to its original state.
Current medication available for Coeliac Disease
Budesonide is a corticosteroid usually given in capsule form which coats the damaged area of the small intestine to allow the villi to recover. Budesonide has been used as a drug to treat inflammation in pneumonia, asthma and has now shown to be effective in people with coeliac disease.[2]
It is prescribed to people with coeliac disease who complain of severe, short-term symptoms as a result of accidental gluten exposure.[2]
Coeliac Disease Medication under trial
Larazotide acetate is a Zonulin antagonist. This means that it can block the pathway for gluten to cross the intestinal mucosal barrier so that gluten can’t cause damage.[3] This drug can control gluten related symptoms, but it can’t restore the small intestinal lining.
At the moment, this drug is currently in a Phase III trial since Larazotide acetate could potentially remove symptoms after having small amounts of gluten.[3]
There would be less restrictions in the diet as people could choose foods that “may contain traces of gluten” and not worry about their meals being cross-contaminated while eating out.[3]
Prolyl Endopeptidase (PEP) can break down gluten whereas AN-PEP can break down gliadin and get rid of the T-cell parts of gluten that signals the body to have an autoimmune response.[4,5]
PEP cannot survive in high pH environments like the stomach. This is a problem as PEP must be able to pass through the stomach and into the small intestine to break down gluten.[5]
Gluten Degrading Enzymes for Treatment of Coeliac disease study has shown that in three small Phase I trials AN-PEP could not significantly degrade gluten.[5]
Latiglutinase is a mixture of enzymes that have made it to Phase 2b trials. This enzyme can break down gluten and allow it to pass through the gut without causing symptoms. Unfortunately, latiglutinase did not show a significant effect and the trial has stopped.[4]
However, since Latiglutenase showed promise up to this point, researchers would like to develop it further to see if it can still be used to break down gluten through other pathways.[4]
The Coeliac (Disease) Vaccine
The Nexvax2 was the most promising vaccine to be placed under trial. It was a peptide-based vaccine that could reduce the response of T cells when gluten was present in the body.[4]
The Nexvax2 also showed signs of improving the duodenal mucosal histology.[4]
It was in Phase II trials, however, Nexvax2 did not show significant results as the vaccine wasn’t able to greatly stop gluten from causing an autoimmune response.[4]
Join us… it’s free… and become a part of our healthy and knowledgeable community by Subscribing to our Newsletter. That way, you will always be informed when a new article, regarding the topics that you are interested in, will be published.
References
(1) Kivelä, L., Caminero, A., Leffler, D. A., Pinto-Sanchez, M. I., Tye-Din, J. A., & Lindfors, K. (2020). Current and emerging therapies for coeliac disease. Nature Reviews Gastroenterology & Hepatology, 1-15.
(2) Therrien, A., Silvester, J. A., Leffler, D. A., & Kelly, C. P. (2020). Efficacy of Enteric-Release Oral Budesonide in Treatment of Acute Reactions to Gluten in Patients With Celiac Disease. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association, 18(1), 254–256. https://doi.org/10.1016/j.cgh.2019.03.029
(3) Caio, G., Volta, U., Sapone, A., Leffler, D. A., De Giorgio, R., Catassi, C., & Fasano, A. (2019). Celiac disease: a comprehensive current review. BMC medicine, 17(1), 142. https://doi.org/10.1186/s12916-019-1380-z
(4) Yoosuf, S., & Makharia, G. K. (2019). Evolving Therapy for Celiac Disease. Frontiers in pediatrics, 7, 193. https://doi.org/10.3389/fped.2019.00193
(5) Wei, G., Helmerhorst, E. J., Darwish, G., Blumenkranz, G., & Schuppan, D. (2020). Gluten Degrading Enzymes for Treatment of Celiac Disease. Nutrients, 12(7), 2095. https://doi.org/10.3390/nu12072095






