
Vanessa Davies
BSc, MSc, BASES HPSA, Burrell education 3rd age Women Menopause transition online certification
Note — The article was checked and updated August 2023.
Menopause is a natural progression as women age. However, many of us think that hot flashes and poor sleep is the highlight of this hormonal transition.
To better understand menopause, we need to know the different stages:
- Perimenopause
- Menopause
- Postmenopause
and also the different causes to menopause, because menopause is not always naturally occuring with age.
What is menopause?
The menopause is a natural hormonal transition in a woman’s life that every woman goes through.[1]
A French physician coined the term menopause in 1821, and medical interest in menopause increased considerably in mid 19th century.[2]
The word “menopause” comes from the Greek words “menos”, meaning month, and “pause”, meaning to cease.[3]
Menopause refers to the final menstrual period a woman experiences.[4] Women are considered to have reached menopause a year after their last period.
When does menopause usually start (and how long does it last)?
Most women become menopausal naturally between the ages of 45 and 55 years. There is no way to predict the age at which a woman’s menopausal symptoms will start or how long they will last.[4]
The average age for menopause is 51 years old
The symptoms of the perimenopause and menopause last for four years on average, but once again, this is a huge spectrum with some women experiencing no symptoms at all and some women still having them in their 70s.[5]
Different stages of menopause
There are 3 different stages of menopause.
Perimenopause
Perimenopause is the phase leading up to the point of menopause.[5]
It begins with the first onset of menstrual irregularity and ends after 1 year an amenorrhea has occurred, thereby defining the final menstrual period.[6]
Perimenopause has two phases
The first phase is characterized by heavier periods or flooding periods, irregular period patterns (i.e long and heavy periods one month and short and light the next), irregular cycles or skipped periods.
The second phase is characterized by more infrequent periods – periods might be lighter, shorter or just spotting. This stage is the most symptomatic stage of the menopause due to the flutuations in the hormones.[1]
Menopause
Women are considered to have reached menopause one year after they had their last period. This is due to a woman’s ovaries no longer producing oestrogen and progesterone.

Postmenopause
When a woman has had no periods for 12 consecutive months, she is considered to be “postmenopausal”.[4] Women will remain postmenopausal for the rest of their lifes.
Three types of menopause
There are different types of menopause that women can go through, and we have discussed these in more detail below.
Artificial menopause
Some women go through an artifical menopause caused by having surgery or taking medication. This is known as surgical menopause or medical menopause.
Surgical menopause is when surgery rather than the natural aging process causes a women to go through menopause. Surgical menopause occurs after an oophorectomy, a surgery that removes the ovaries.[7]
Medical menopause occurs when women take certain medications that dramatically reduce levels of oestrogen. There are three types of medication that have this effect:
- Aromatase inhibitors
- Tamoxifen
- GNRH Agonists.[8]
Premature or early menopause
When the menopause occurs before the age of 45, it is called an early menopause.[9]
If there is no obvious medical reason for early menopause, the cause is likely genetic, meaning that the age of menopause onset is likely inherited.[10]
Conditions and lifestyle factors that influence menopause onset are discussed in more detail later in this article.
Natural menopause
Menopause happens naturally due to the ovaries slowly stopping to produce eggs / oocytes when getting over the age of 45, with the average age being 51.
What can cause an early start to menopause?
There are certain conditions and lifestyle choices that can influence when menopause will start.
Autoimmune conditions
These are a group of conditions where the immune system attacks the body’s own cells. For example
- HIV
- Thyroid disease
- Rheumatoid arthritis
- Type 1 diabetes
RELATED — Type 1 Diabetes: Autoimmune disease that is on the rise
Autoimmune conditions are associated with an earlier age of menopause. The reasons are likely complex and can vary from medical conditions, so more research is needed.[8]
Epilepsy
There is some evidence that menopause may occur a decade earlier in some women with epilepsy, especially those with
- Catamenial epilepsy (worsening of seizures near the time of menstruation)
- High seizure rates
Some doctors think this difference may be related to the effects of seizures on the brain structure called the hypothalamus or the pituitary gland, but more research is needed. Most women with epilepsy experience menopause at about the same age as other women.[11]
Genetics and chromosome issues (e.g. Turner syndrome, Fragile X, Gonadal dysgenesis)
Approximately 10% of women with primary ovarian insufficiency (menopause before the age of 40) will have a genetic cause identified, most commonly an abnormality involving the X chromosome.[8]
Two functioning X chromosomes appear necessary for normal ovarian function. The most obvious genetic cause of premature ovarian failure is Turner Syndrome, in which a complete or near-complete loss of the second X chromosome occurs.[12]
Lack of exercise
More research is needed in the area of exercise and its impact on early menopause.
RELATED — Training and menopause: How can exercise positively affect your transition?
However, a study by Zhao et al found that although physical activity has been shown to have wide ranging positive health effects overall, results of this large, prospective study do not support an important role of physical activity with regard to risk of early menopause.[13]
Lack of sun exposure (low levels of vitamin D)
There are suggestions that lower levels of vitamin D are associated with early menopause.
A study by Purde-Smithe et al evaluated how intakes of vitamin D and calcium are associated with the incidence of early menopause and they found that women with the highest intake of dietary vitamin D (quintile median: 528 IU/d) had a significant 17% lower risk of early menopause than women with the lowest intake (quintile median: 148 IU/d).
Higher levels of vitamin D are associated with lower risk of early menopause
Associations were stronger for vitamin D and calcium from dairy sources than from non dairy dietary sources, whereas high supplement use was not associated with lower risk.[14]
RELATED — Vitamin D: The sunshine hormone for stronger bones
Body mass index (BMI)
It seems that being underweight is associated with an earlier menopause.[8]
A study collating data from 11 prospective studies found that underweight women had over twice the risk of experiencing early menopause, while overweight and obese women had over 50% higher risk of experiencing late menopause.[15]
Endocrine-disrupting chemicals
These chemicals are found in the environment and can interfere with hormones.
Higher levels of the endocrine disrupting synthetic chemicals known as PFAS are linked with an earlier menopause.[8]
Smoking
Smoking has the next biggest impact after genetics, lowering the age by approximately 2 years, and it also shortens the menopause transition, also referred to as perimenopause.
RELATED — Anxiety and Smoking: How it affects our Mental Health
Quitting smoking remains the best health intervention a women can do for menopause.[8]
Why does menopause occur?
Declining reproductive hormones
Menopause naturally happens when ovulation no longer occurs and production of oestrogen and progesterone ceases.[4] This is because hormones oestrogen and progesterone work together to regulate the menstrual cycle.
During perimenopause, the levels of these hormones fluctuate greatly, and it is often their imbalance that leads to symptoms of the menopause occurring.[9]
Women also produce testosterone in the ovaries and adrenal glands, and research shows that they produce three times as much testosterone than estrogen before the menopause.
Levels of testosterone in the body drop more sharply around the time of the perimenopause and menopause and stay low thereafter.[16]
Levels of FSH (follicle-stimulating hormone also known as gonadotropin) and LH (luteinising hormone) increase during perimenopause and menopause.
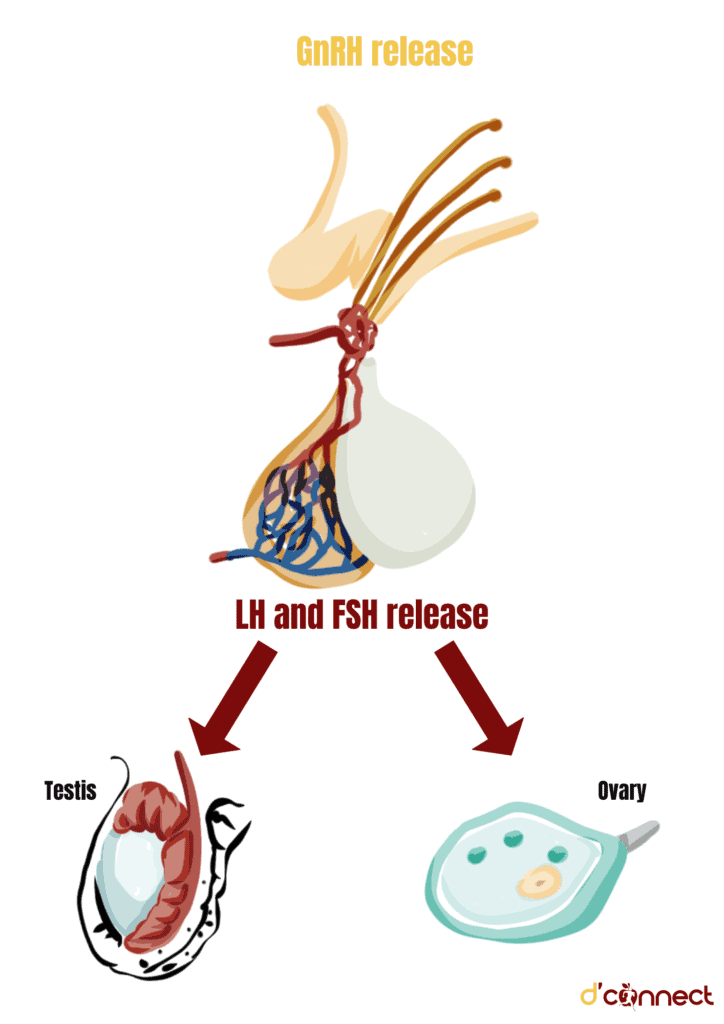
FSH causes ovarian follicles to enlarge and produce estrogen. Decline in estrogen leads to an increase in FSH as there is not enough estrogen being produced to “turn off” the brain’s production of FSH.[17]
Removing of ovaries (oophorectomy)
As mentioned before, oophorectomy is when one or both of the ovaries are removed. The ovaries contain eggs and produce sex hormones that control the menstrual cycle.
Hysterectomy
If a womb (uterus) was removed by an operation, women can also experience early menopause even if the ovaries remain intact.
The ovaries will still produce some oestrogen after the hysterectomy, but it is common that the levels of oestrogen fall earlier than usual due to reduced blood flow.[9]
Primary ovarian insufficiency (POI)
Loss of ovarian function occurring in women younger than 40 years of age is called premature ovarian insufficiency (POI).[8]
If menopause happens before the age of 40, it is classed as Premature Ovarian Insufficiency (POI). Early menopause or POI can sometimes run in the family.[18]
Chemotherapy and radiation therapy
Chemotherapy or radiation therapy can cause early menopause because these treatments are toxic to the ovaries, especially when used at high doses to treat cancer.
Menopause signs and symptoms
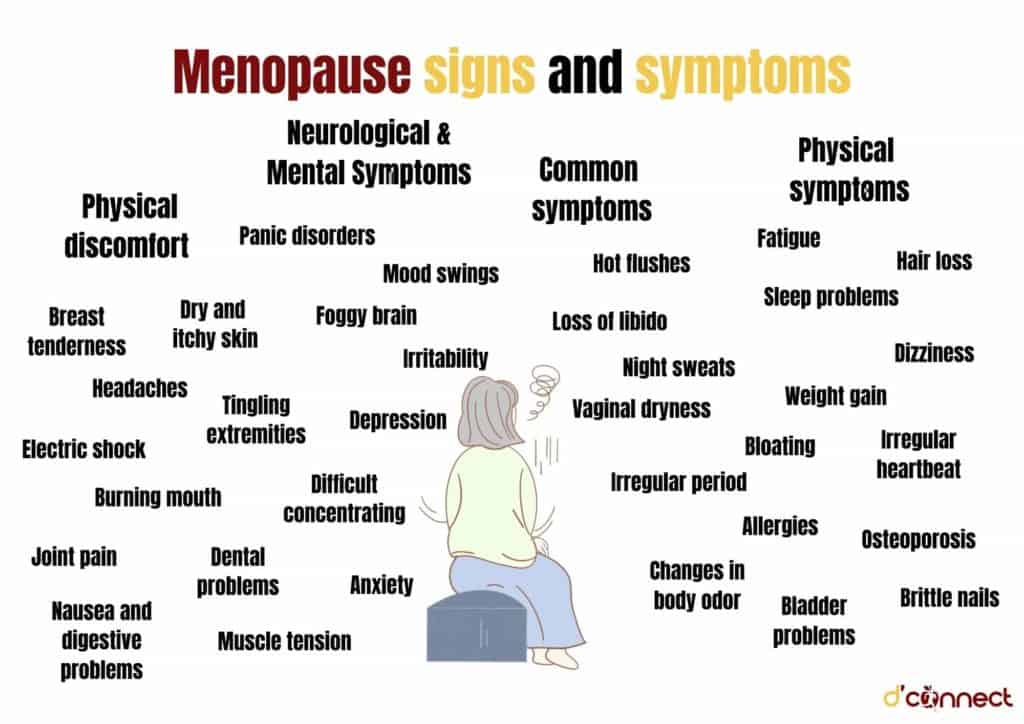
Women have oestrogen receptors throughout their bodies. Oestrogen protects a number of different organs and areas such as
- Brain
- Heart
- Skin
- Bones
- Urinary functions
- Genital area
Low levels of oestrogen can affect all parts of our body
This is why there are many different symptoms of menopause that can be experienced through perimenopause and into postmenopause.
Common symptoms
- Hot flushes
- Night sweats
- Loss of libido
- Vaginal dryness
- Irregular period
Physical symptoms
- Fatigue
- Hair loss
- Sleep problems
- Dizziness
- Weight gain
- Bloating
- Allergies
- Brittle nails
- Osteoporosis
- Irregular heartbeat
- Changes in body odor
- Bladder problems
Neurological / Mental Symptoms
- Anxiety
- Irritability
- Panic disorders
- Difficult concentrating
- Mood swings
- Foggy brain
- Depression
Physical discomfort
- Breast tenderness
- Headaches
- Joint pain
- Electric shock (sensation feels like a ‘snap, crackle and pop’ under the skin)
- Burning mouth
- Nausea and digestive problems
- Dental problems
- Muscle tension
- Dry and itchy skin
- Tingling extremities[5]
RELATED — Menopause: Guide to Signs and Symptoms
Menopause treatments
There are a number of options available to women to help them through the menopause transition.
Hormone replacement therapy (HRT)
Medical intervention is one way to treat menopause symptoms. There are different types of hormone replacement therapy available such as
- Bio-identical hormones (synthetic hormones)
- Body identical hormones (natural hormones)
It is advised for women to speak to their GP about the different options available in order to see what would suit them best.
Lifestyle changes
There are many lifestyle choices that women can make to help manage their menopause symptoms. The aim of these lifestyle choices is to reduce inflammation in the body.
These include:
Diet – a well balanced diet for overall health is always recommended. Certain foods can help to manage symptoms and you may find some foods that can trigger symptoms.
RELATED — The Healthy Plate Model: Essentials of Healthy Eating
Hydration – hot flashes and night sweats can lead to dehydration and being hydrated can help manage such instances.
Reducing alcohol intake – alcohol impacts sleep which in many women is affected during perimenopause and menopause. Alcohol can also impact hot flushes and other menopause symptoms.
RELATED — Different types of sleep: which one do we need the most?
Reducing caffeine intake – caffeine can trigger hot flashes in women.
Exercise – exercise can help to manage symptoms of menopause and is also beneficial for overall health, including cardiovascular health and bone health.
Reducing stress – during times of stress our bodies produce cortisol from the adrenal glands. The adrenal glands also produce oestrogen and progesterone but at much lower levels than the ovaries.
RELATED — Psychological benefits of Yoga: what does science and research say (Part 1)

When stressed, the adrenal glands prioritize producing cortisol over oestrogen and progesterone
Reducing endocrine disrupting hormones – these can be found in the environment. For example, pesticides on food or in plastic we use.
When these get into our body they have the ability to mimic our natural hormones, for example oestrogen.
Focus on good sleep – progesterone helps with sleep, and as its levels decline during perimenopause and menopause, sleep can get disturbed.
RELATED — Magnesium (for a great night of sleep)
These lifestyle choices are great to help women with their long term health.
Related Questions
1. What are the worse symptoms of menopause?
Menopause is very individual and everyone will have different experiences with type of symptoms and severity of symptoms.
Some might suffer from bad hot flashes and find this to be a debilitating symptom, while others may find that brain fog is their most difficult symptom to deal with.
2. What is the safest treatment for hot flashes?
A study by Herber-Gast et al showed that consumption of Mediterranean-style diet decreased the risk of reporting vasomotor symptoms.[20]
RELATED — What is a plant-based diet: Vegan or Vegetarian?
On the other hand, consumption of a high-fat and sugar diet increased the risk of vasomotor symptoms. Reducing alcohol and caffeine has also shown to be beneficial.
3. What foods can make menopause worse?
Spicy foods and foods high in sugar as well as alcohol and caffeine can make symptoms worse.
4. What are the signs of coming to an end of menopause?
Once you are postmenopause (it has been 12 months since your last period), symptoms that you have been experiencing will become milder and disappear completely.
5. Are there benefits to having menopause?
Some benefits include not having any periods or PMS, fibroids shrink and often get better. Endometriosis also disappears, as well as hormonal headaches (menstrual migraines).[5]
Vanessa Davies is a female health coach who is passionate about helping women to achieve their health, wellbeing and performance goals. Originally from the UK, Vanessa has 18 years experience working in high performance sports, supporting Olympic/Paralympic and Commonwealth athletes.
She is also trained in postnatal exercise and the 3rd age women, where with her holistic approach she assists women to understand and work with their bodies so they can live their lives to the fullest.
References
(1) Devin , R. (2022). Getting up to speed with the menopause. Nursing in Practice. Retrieved from https://www.nursinginpractice.com/clinical/womens-health/up-to-speed-menopause/
(2) Singh, A., Kaur, S., Walia, I. (2002). A historical perspective on menopause & menopausal age. Bull Indian Inst Hist Med Hyderabad. 32(2):121-35. Retrieved from http://ccras.nic.in/sites/default/files/viewpdf/jimh/BIIHM_2002/121%20to%20135.pdf
(3) Hailes, J. (2022). Menopause.
(4) What is menopause? Australasian Menopause Society. Retrieved from https://www.menopause.org.au/hp/information-sheets/what-is-menopause
(5) Matthews, M. (2020). Taking on the menopause with attitude and style the new hot. London. Vermilion.
(6) Santoro, N. (2016). Perimenopause:from research to practice. Journal of Women’s Health. Apr 1; 25(4):32-339. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4834516/
(7) Nwadike, V.R.(2020). Surgical menopause. Healthline. Retrieved from https://www.healthline.com/health/surgical-menopause
(8) Gunter, J. (2021). The Menopause Manifesto. London. Piatkus.
(9) Newson, L. (2020). What is the menopause? Newson Health Limited. Retrieved from https://www.newsonhealth.co.uk/uploads/2021/07/What-is-the-Menopause-v21-02.pdf
(10) Watson, S. (2022). What causes early menopause? Healthline. Retrieved from https://www.healthline.com/health/menopause/causes-early
(11) Schachter, S.C., Sirven, J.I. (2013). Menopause & Epilespy. Epilepsy Foundation. Retrieved from https://www.epilepsy.com/living-epilepsy/epilepsy-and/women/menopause-and-epilepsy
(12) Santoro, N. (2003). Mechanisms of premature ovarian failure. Ann Endocrinol. Apr; 64(2): 87-92.
(13) Zhao, M et al. (2018). Physical activity is not related to risk of early menopause in a large prospective study. Human reproduction. 33(10):1960-1967. Retrieved from https://academic.oup.com/humrep/article/33/10/1960/5077232
(14) Purdue-Smithe, A.C. et al. (2017). Vitamin D and calcium intake and risk of early menopause. The American journal of clinical nutrition. 105 (6): 1493-1501. Retrieved from https://academic.oup.com/ajcn/article/105/6/1493/4633994
(15) Zhu, D et al (2018). Body mass index and age at natural menopause: an international pooled analysis of 11 prospective studies. Eur J Epidemiol. 33 (8): 699-710.
(16) Newson, L. (2022). Testosterone. Newson Health Limited. Retrieved from https://www.newsonhealth.co.uk/uploads/2021/07/Testosterone-FINAL-22.pdf
(17) Menopause. Penn Center for Women’s Behavioral Wellness. Perelman School of Medicine. Retrieved from https://www.med.upenn.edu/womenswellness/menopause.html
(18) Webber L, Davies M, Anderson R, et al. (2016). ESHRE Guideline: management of women with premature ovarian insufficiency. Hum Reprod 31(5): 926-37.
(19) Early menopause – chemotherapy and radiation. Australasian Menopause Society. Retrieved from https://www.menopause.org.au/health-info/fact-sheets/early-menopause-chemotherapy-and-radiation-therapy
(20) Herber-Gast G-MC, Mishra G D (2013). Fruit, Mediterranean-style, and high-fat and sugar diets are associated with the risk of night sweats and hot flushes in midlife: results from a prospective cohort study. The American Journal of Clinical Nutrition 97 (5): 1092–1099. Retrieved from https://academic.oup.com/ajcn/article/97/5/1092/4577089







Great reading thanks Ness. Enjoy learning and understanding more about menopause with helpful ideas to help us older gals manage this crazy space us.
Nice work 👌