
Carly Hanna
BSc (Human Nutrition and Psychology)
Note — The article was checked and updated November 2023.
Jump to:
- What is Calcium?
- Calcium deficiency
- Different types of Calcium
- Health Benefits
- Health Claims
- Best sources of Calcium
- Daily requirements and intake
- How to take calcium supplements
- Signs and symptoms of deficiency
- Risks and side effects
- Interaction - herbs and supplements
- Interaction - medication
- Summary
- Related Questions
We’ve all heard that we need to drink milk to build strong bones. Yes, dairy is a rich source of calcium, but did you know that fortified non-dairy milk, such as
- Soy milk
- Almond milk
- Oat milk
- Rice milk
can provide just as much calcium, if not more, per 100ml!
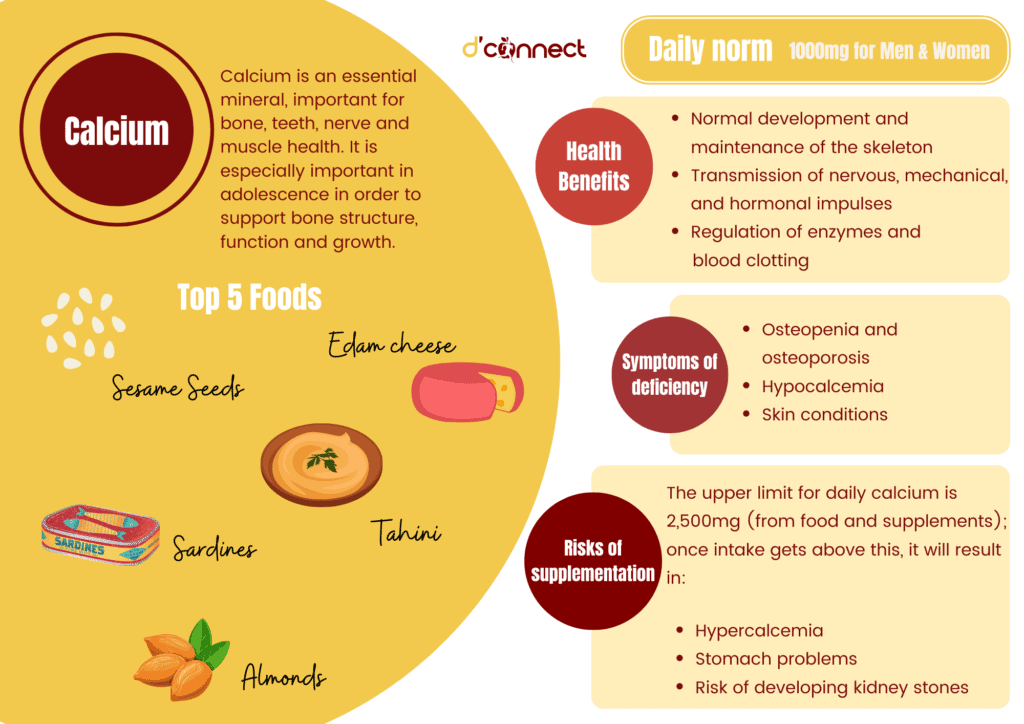
Calcium is important for bones and teeth as well as nerves and muscles. It is an essential nutrient for the body and there are certain signs to recognise if we are deficient or have too much of it in our diet.
It is also important to note that not all minerals are in isolation, as there are other vitamins and minerals that are essential in supporting calcium’s role in the body. So, how do we know if calcium supplements are a good choice for us? Let’s take a look.
What is Calcium?
Calcium is the most abundant nutrient stored in the body, important for bone and teeth health, as well as a wide range of other bodily functions including muscle contraction, blood clotting, regulating heart rhythm and nerve function.[1]
It was first discovered in the early 1800’s by chemist Sir Humphry Davy and is naturally occuring in shells, rocks, and minerals as well as teeth and bones.
In terms of food, it is commonly thought that calcium can only be found in dairy products. However, there are also a wide range of foods that are good sources of calcium. These include
- Sardines and salmon (with bones)
- Broccoli
- Sesame seeds and tahini (ground sesame seed paste)
- Dark leafy greens and soy products, such as edamame and tofu
Calcium is not a mandatory fortified nutrient to foods in New Zealand; however, it is often added to plant-based milks.

Fortified foods provide a wider variety of vitamins and minerals that the body needs, as opposed to supplements which are often isolated forms of nutrients.
Calcium carbonate is the most common calcium supplement
We know that calcium is good for us, but how do we know if we are getting enough of it through our diet? Also, when is it safe to use supplements?
Calcium deficiency
Nutrient deficiencies, such as calcium deficiency, can be a result of
- Insufficient dietary intake
- Low absorption rates
- High excretion rates
- Lifestyle factors
- Life stage/age
- Disorders and diseases[2]
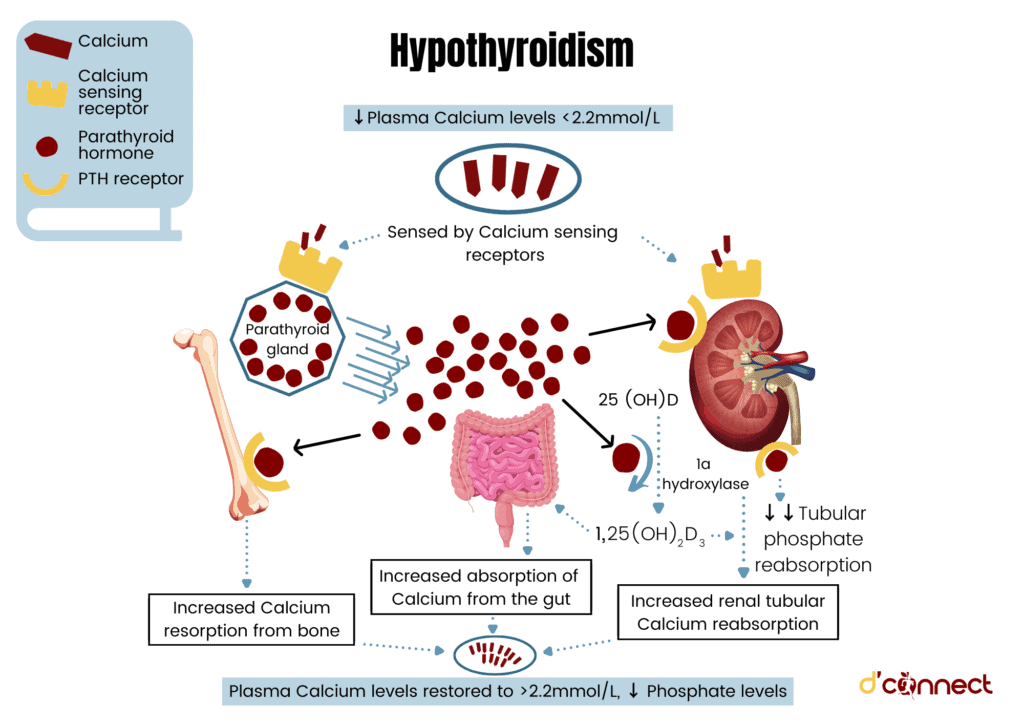
If calcium blood levels are too low, our bones start to release calcium. This is signalled by the parathyroid hormone.
Typical calcium deficiency symptoms are bone and teeth deteriorations, skin and hair problems, digestive issues, and muscle and nerve effects.
It is widely known that being deficient in calcium can increase our risk of osteoporosis, though there are several other risk factors for certain groups of people. We talk about this in more detail below.
Who is most at risk of calcium deficiency?
Growing "youngsters", especially teenagers
Bone mass is exponential during adolescence, up to seven times the amount. Children need a higher calcium intake to support building strength in their bones and skeleton.[1]
Men over 70
Calcium loss from bones is accelerated with older age, so men over 70 and women after menopause (around 50+) require higher amounts of calcium in their diet.[1]
Menopause and calcium levels
As we get older, our body is less able to absorb calcium.[3] For women especially, estrogen (sex hormone) decreases during menopause which causes bones to deteriorate faster.
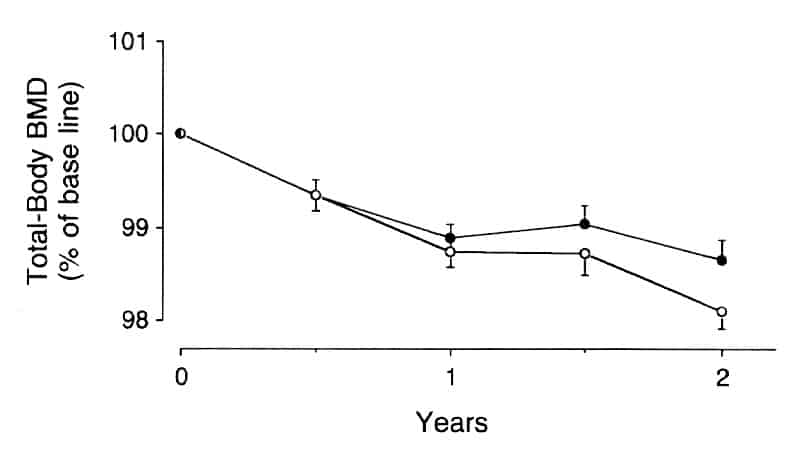
Source: Reid IR, et al. Effect of Calcium Supplementation on Bone Loss in Postmenopausal Women. The New England Journal of Medicine (February 1993).
Women over 50 are more at risk of being calcium deficient and at a higher risk for osteoporosis.[4]
RELATED — Menopause Revealed: Signs, Stages, Types and Treatment
Individuals with dairy intolerance or milk allergy
As dairy foods are a rich source of calcium, those who are intolerant or allergic to dairy, or choose to avoid dairy due to ethical/environmental reasons (vegans), are less likely to meet their calcium requirements.
These individuals need to make sure they substitute dairy products with appropriate plant-based rich calcium sources.
Seniors and dietary deficiency
Adolescence is a stage of life that has a higher energy requirement, and hence needs more nutrients such as calcium, which makes this group at risk.
In late adulthood, the elderly are more likely to have a reduced calcium absorption (due to age and likelihood of being on multiple medications) as well as a reduced appetite (which could reduce their calcium intake).
Individuals who are diagnosed with eating disorders
Having a restricted intake of food is always going to result in an increased risk of nutrient deficiencies.
Eating disorders can be associated with perfectionism, body image, wanting to gain control, and are affected by social stereotypes, media, and other associated mental health conditions.
RELATED — Understanding Eating Disorders: History, Types and Statistics
Women exhibiting physical hyperactivity with female athlete triad syndrome
The female athlete triad is a syndrome often found in women participating in sports, which causes
- Irregular or lack of menstruation
- Low energy
- Decreased bone density
This can be a result of overexercising and potentially undereating (with or without an eating disorder) as there is not enough nutrient availability for activity requirements.
Lifestyle factors, such as smoking and diet
Tobacco cigarettes and diets high in caffeine, sodium (salt), and protein can all contribute to an increased loss of calcium from the body.
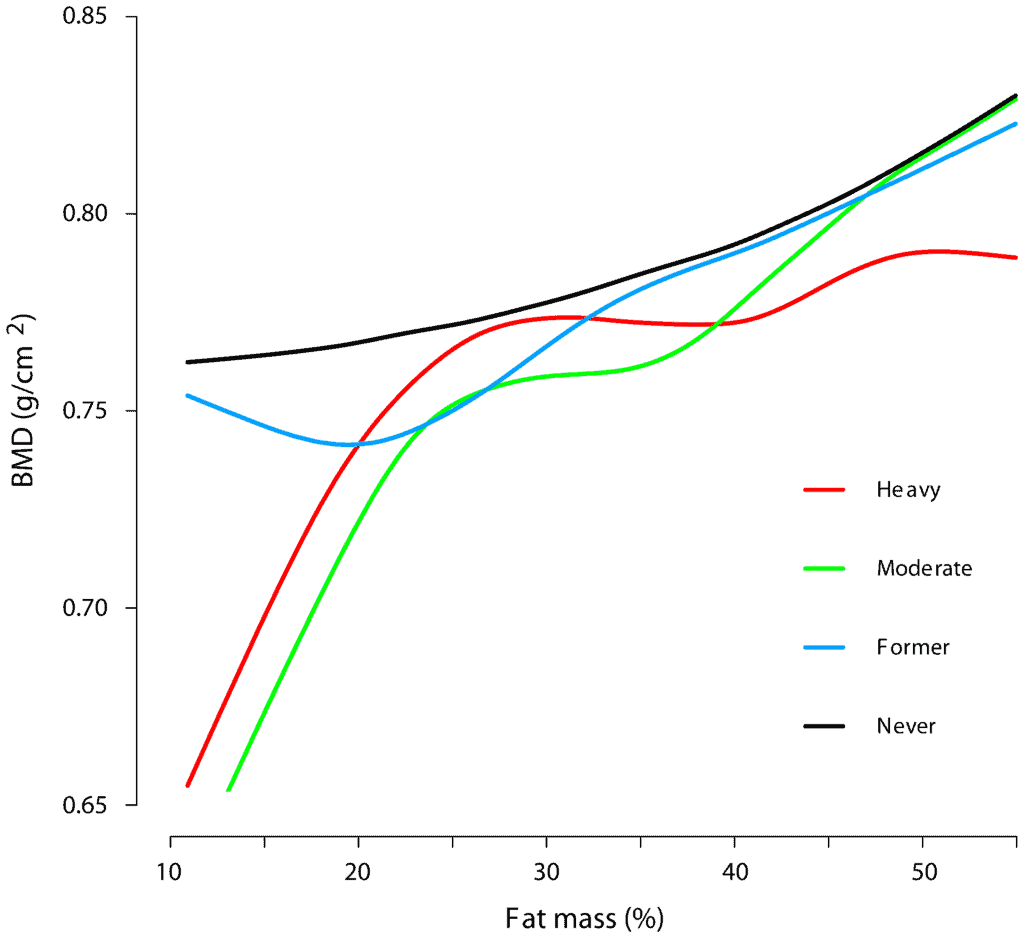
Source: Nygard C.G., et al. Smoking and Body Fat Mass in Relation to Bone Mineral Density and Hip Fracture: The Hordaland Health Study. (Plos One, March 2014).
While there may be sufficient intake and normal absorption, high excretion rates of calcium are likely to cause deficiency.[1]
Different types of Calcium
Absorption rates of calcium supplements are about 30%, but can vary between each type. It is also important to note that the elemental calcium (total calcium within the compound) differs between types of calcium.[2]
Calcium supplements are also likely to be bound with compounds that contain magnesium and/or vitamin D.
RELATED — Magnesium: For a great night of sleep
Calcium carbonate
This is a supplement that has the highest amount of elemental calcium (40%). It is best absorbable with food. However, this form is also more likely to cause constipation as a side effect.[5]
Calcium chloride – anhydrous and solution form
Anhydrous means without water, so this form of calcium chloride is usually in tablet or powder form. The solution form of calcium chloride is often given by infusion.
Both forms are quite likely to have side effects, such as an upset stomach, allergic reactions and/or mood changes.
Calcium citrate
Calcium citrate contains about 21% of elemental calcium and is well absorbed in the body. This supplement form works well when taken with or without food.[5]
Calcium gluconate
While calcium gluconate has a high bioavailability, the supplements only contain about 9% elemental calcium. This means that we may have to take a few tablets to get the required amount of calcium, which makes this a more expensive supplement option.[6]
Calcium glycerophosphate
Calcium glycerophosphate is a form of calcium salt that can be found in foods and dental and oral hygiene products. It is not generally consumed as a supplement.
Calcium lactate
Lactate is the enzyme that is found in dairy and is commonly used as a preservative in food products. Calcium lactate has high bioavailability, 13% elemental calcium, and is similar to calcium gluconate where we may need to take a few tablets to get an adequate dose of calcium.[6]
Calcium sodium lactate
Calcium sodium lactate is also found in dairy products, but the isolated form (supplement) is not the most effective.
Calcium oxide
Calcium oxide is a food additive that can be toxic to humans if consumed in high amounts, so it’s not recommended to take.
RELATED — What are Food Additives and why are they in our food?
Calcium phosphate, tribasic and microcrystalline hydroxyapatite (MCHC)
Calcium phosphate is also found in cow’s milk, along with calcium lactate. In supplement form, it can come as either tricalcium phosphate (tribasic) or MCHC – however, these aren’t well absorbed and can be quite expensive.[7]
Calcium sulphate
Calcium sulphate is a commonly permitted additive in foods and originates from calcium salts. Because of this, it is not considered safe in high doses.
Calcium ascorbate
Calcium ascorbate contains 10% elemental calcium and is combined with ascorbic acid (vitamin C) which helps with the absorption of the calcium. However, this form has low elemental calcium.[6]
RELATED — Vitamin C: Immunity and Collagen booster
Summary - The best form of Calcium
Most absorbable – calcium carbonate and calcium citrate
Least absorbable – calcium sulphate, calcium oxide, calcium sodium lactate, calcium glycerophosphate
Most expensive – calcium MCHC, calcium gluconate, and calcium lactate
Least expensive – calcium carbonate
Most safe – calcium citrate and calcium carbonate
Least safe – calcium chloride.
Health benefits of Calcium
Calcium is essential in muscle, nerve and hormone function, enzyme regulation, and can be protective against some cancers, cardiovascular disease, and obesity. Let’s go into more detail of how and why.
Normal development and maintenance of the skeleton
More than 99% of calcium in our body is stored in the bones and teeth, with the remaining <1% in extracellular serum. Having sufficient calcium levels is essential for the development and maintenance of bone structure and function.[2]
Proper functioning of neuromuscular and cardiac systems
Calcium is one of the body’s electrolytes, alongside
- Magnesium
- Sodium
- Chloride
- Potassium
that are all important for muscle function, vascular contraction and vasodilation.
RELATED — Potassium (for blood pressure, heart rhythm and pH balance)
This includes pumping blood from the heart to around the body. An imbalance of calcium can cause heart issues such as ectopic beats (extra heart beats) and arrhythmias (abnormal heart rhythms).[2]
Imbalance in calcium levels can cause heart issues
Transmission of nervous, mechanical, and hormonal impulses
Calcium is involved in hormone secretion and intracellular signalling which is important for communication between different organs, muscles, and nerves in the body. [2]
Regulation of enzymes and blood clotting
Calcium is a key signaling molecule that is important for several intracellular processes and enzyme functions such as being a cofactor for coagulation, otherwise known as blood clotting.[8]
Protective against colorectal cancer
Evidence shows that taking 1,200mg of calcium daily decreases our risk of colorectal tumours by 26% (only some are cancerous).[9]
Protective against cardiovascular effects
Healthy calcium levels help reduce high blood pressure.
Maintaining a healthy blood pressure helps keep the heart healthy and can protect against cardiovascular diseases.[2]
Helps maintain weight and reduce risk of obesity
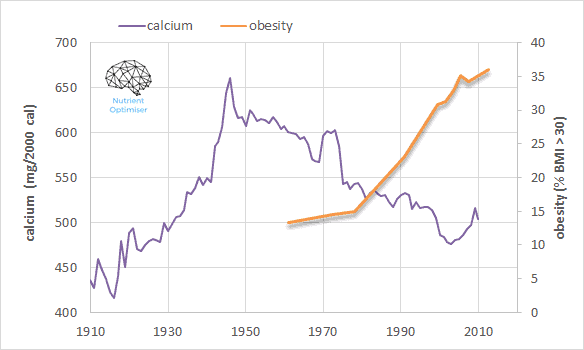
Research shows that a higher total calcium intake is associated with a 22% reduced risk of obesity. The relationship between calcium levels and maintaining weight are more likely to be mediated by healthy eating habits and meeting nutrient requirements.[2]
Health claims that still need more evidence and research
Helps with PMS symptoms
Research has shown that 500mg of daily calcium supplements improved mood and reduced fluid retention in women experiencing PMS symptoms.[4]
Helps against mood disorders (such as depression)
While more research is needed to understand the relationship between calcium and depression, one study has shown that higher levels of calcium intake is associated with lower self-reported scores of depression in middle-aged females.[10]
Adequate calcium intake can help with depression
RELATED — Introduction to: Depression
Protective against diabetes
Calcium may have a role in insulin secretion and sensitivity. One meta-analysis of studies has shown that a calcium intake of 600-1,200mg a day can reduce the risk of Type II Diabetes Mellitus.[11]
RELATED — Diabetes: Early Signs, Causes, Types and Treatment
Lowers blood pressure
Some evidence suggests that a higher total calcium intake (higher than the recommended daily allowance) can help maintain healthy blood pressure.
While evidence in the research has several design problems, larger trials are needed to investigate calcium’s effect on lowering blood pressure.[9]
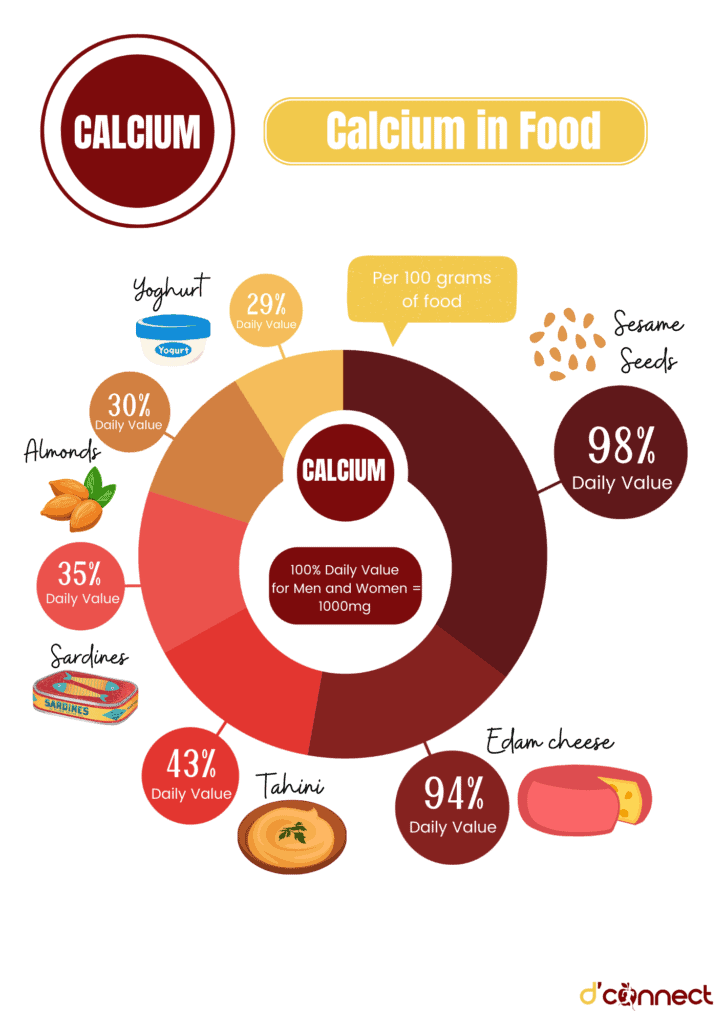
Best sources of Calcium
Dairy sources (milk, cheese, yoghurt) often have high amounts of calcium and are easily absorbed by the body.
There are also plant-based foods and other sources that are good sources of calcium.
RELATED — What is a plant-based diet: Vegan or Vegetarian?
See the table below for the top 15 food sources of calcium, per 100g (serving size indicated also).
Food Sources | Concentration (mg/100g) | Daily Value (DV) %RDI (1000mg) |
Sesame seeds | 978mg (11 tablespoons) | 98% |
Edam Cheese | 938mg | 94% |
Tahini | 426mg (1/3 cup) | 43% |
Sardines | 350mg (5 sardines) | 35% |
Almonds | 300mg (100 raw nuts) | 30% |
Yoghurt | 290mg (2/3 pottle) | 29% |
Light blue top milk | 144mg (100ml) | 14% |
Dark leafy greens | 141mg (1/2 cup cooked) | 14% |
Brazil nuts | 136mg (20 raw nuts) | 14% |
Non-dairy soy milk (fortified) | 120mg (100ml) | 12% |
Tofu (firm) | 105mg | 11% |
Broccoli | 97mg (2/3 cup cooked) | 10% |
Cottage cheese | 88mg (6 tablespoons) | 9% |
Sour cream | 87mg (7 tablespoons) | 9% |
Whole Grain bread | 73mg (2 slices) | 7% |
Note – please ensure not to overindulge in Brazil nuts since they have high amounts of Selenium which can be toxic.
Usually, you should limit your consumption of Brazil nuts between 2-5 per day.
Daily requirements and recommended intake
Our calcium requirements may differ throughout different stages of our life and depending on our biological sex.
See the table below for the recommended dietary allowance, based on age and sex.[1]
Age (years) | Male (mg) | Female (mg) |
1-3 years | 500mg | 500mg |
4-8 years | 700mg | 700mg |
9-11 years | 1000mg | 1000mg |
12-18 years | 1300mg | 1300mg* |
19-49 years | 1000mg | 1000mg* |
50-70 years | 1000mg | 1300mg |
>71 years | 1300mg | 1300mg |
*Pregnant and breastfeeding females have the same requirements. No need to increase calcium intake as absorption rate of calcium increases.[2]
How to take calcium supplements
For best absorption it is recommended to take calcium supplements in small doses (<500mg) and with food.
Taking a calcium supplement with a vitamin D supplement can help with the absorption.
Vitamin K2 can also help with the processing of calcium into the body without causing calcium deposits (which can have adverse effects on health).
Supplements to avoid taking at the same time are
- Magnesium
- Zinc
- Iron
as these nutrients all compete with calcium for absorption.
Common signs and symptoms of calcium deficiency
Calcium deficiency can show up as multiple types of symptoms.
While it is commonly known that a lack of calcium in the diet will have effects on bone and teeth health, there is also loss of function in the skin, muscles, nerves, and digestive system. These can manifest as symptoms including the following listed below.
Osteopenia and osteoporosis
Osteopenia is the loss of nutrients from the bone which can result in osteoporosis (a skeletal disorder that is characterized by weakened bones). This means that we are more prone to injury and vulnerable to fractures.[4]
Hypocalcemia
Hypocalcemia can be classified as having a total serum calcium concentration of less than 2mmol/L (normal serum calcium levels are between 2-2.5mmol/L).
Having low calcium levels in the blood is a serious deficiency of calcium and can result from kidney failure, diuretics, and/or gastric bypass surgery. This can lead to a variety of symptoms such as
- Muscle aches and spasms – around all areas of the body and can also include cramps or muscle weakness
- Pain in the thighs and arms while walking or moving – this could also be due to muscle fatigue and aches
- Numbness and tingling – in the limbs (arms and legs), extremities (hands and feet) and around the mouth
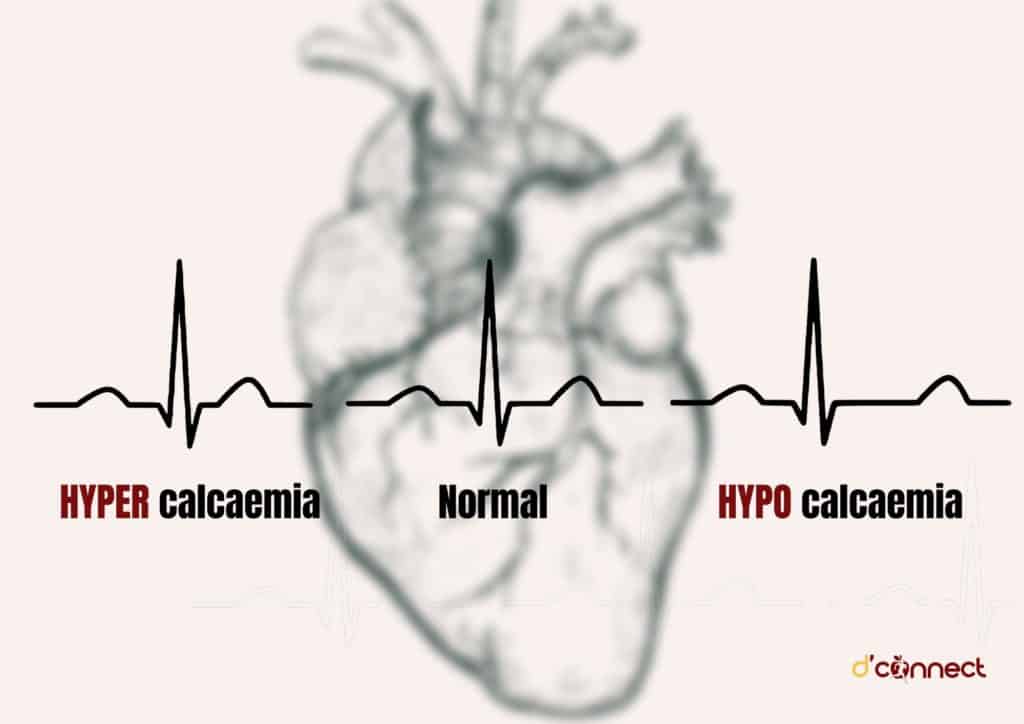
- Abnormal heart rhythms – differences in ECG patterns (pictured below). In severe cases, hypocalcemia can lead to irregular heart patterns or even death.
- Fatigue, insomnia, lightheadedness, dizziness, and brain fog – being low in calcium may cause us to feel psychological and neurological effects such as being unable to concentrate and feeling dizzy
- Poor appetite and nausea – along with fatigue, lack of appetite and feeling sick can be associated with being low in calcium levels[9]
Dry and brittle nails and coarse hair
A more chronic calcium deficiency can lead to breakdown of nails and hair.[4]
Skin conditions
Calcium deficiency can manifest with skin problems such as eczema, skin inflammation, skin itchiness, dry skin, and psoriasis.[4]
Severe premenstrual syndrome (PMS)
One study showed that having low levels of calcium (and vitamin D) during the second half of the menstrual cycle contributes to symptoms such as headaches, bloating and cramps.[4]
Dental problems
As calcium is important for the formation and maintenance of bones and teeth, deficiency can lead to
- tooth decay
- brittle teeth
- irritated gums
- weak tooth roots.[4]
Hypoparathyroidism
Hypothyroidism is a hormone disorder where the parathyroid hormone (which controls calcium levels in the body) production is reduced.[4]
Rickets in young children
Being low in calcium also increases the risk of being deficient in vitamin D, which in children, can cause rickets. This is a rare condition where the bones are softened and weakened which could result in deformities.
Calcium risks and side effects
The upper limit for daily calcium is 2,500mg (from food and supplements); once intake gets above these limits results in toxicity.[9]
Hypercalcemia (high blood levels of calcium)
Mild hypercalcemia is when serum calcium levels are between 2.5-3mmol/L; any level above this can be life threatening. Hypercalcemia can include several symptoms including
- weakness and fatigue
- nausea and vomiting
- shortness of breath
- chest pain
- heart palpitations/abnormal heart rate.[9]
Maximum intake of calcium should not exceed 2.5 grams a day
Urinary calcium
In order to maintain homeostasis (balance in the body), if there is too much calcium in the blood, the kidneys will excrete more through urine.[2]
Risk of developing kidney stones (nephrolithiasis)
Taking a calcium supplement, when we already have sufficient levels, can lead to a buildup of calcium deposits. When the body tries to excrete these deposits, it is commonly known as kidney stones, which can be incredibly painful.[3]
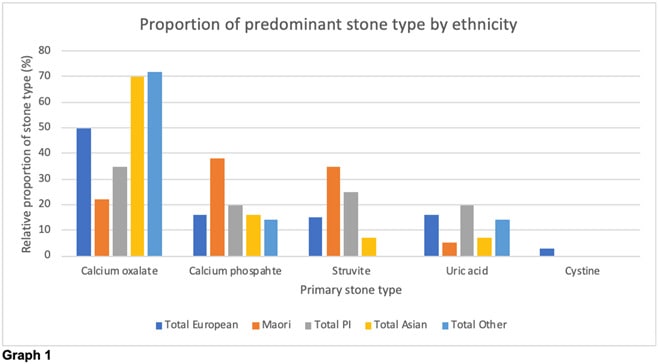
Source: Hunter, J., et al. Effect of ethnicity on stone composition and outcomes in New Zealand (Journal of Urology, April 2020)
Stomach problems
Taking excess calcium supplements can lead to stomach problems such as bloating and constipation.[3]
Spike in blood calcium levels
As supplements are high concentrations of nutrients, this can cause our blood concentration levels to spike higher than what they normally would when obtaining the nutrient from food.[3]
Possible interactions with herbs and supplements
Zinc, magnesium and iron all compete for absorption with calcium, so it is best to avoid taking these supplements at the same time as calcium.
RELATED — Iron (for immunity support and energy production)
This is often why vegetarians are more at risk of iron deficiency than vegans because they often eat lots of dairy (as a protein source), as opposed to vegans who do not.
Having a high calcium intake can inhibit iron absorption.
Possible interactions with medications
Calcium supplements can interact with medications such as blood pressure medication and antibiotics (tetracycline).[12]
Calcium supplements can also interact with hypothyroidism medication such as levothyroxine.
In order to avoid negative side effects, we can still take calcium supplements with one of these medications, just make sure you take them hours apart.[5]
If you are on calcium channel blockers, which are commonly used to treat high blood pressure, you should not take calcium supplements. 800mg of calcium supplement a day can increase your risk of cardiovascular events, such as a heart attack, by 85%.
Alcohol, oxalates (naturally occurring compounds in plants), and corticosteroids, such as prednisone, can increase our needs for calcium due to them having an effect on lowering absorption rates.[9]
Summary
- It is recommended to eat 2-3 servings of dairy products (or non-dairy alternatives) a day, as seen in the table of calcium sources.[1]
- Having a higher intake than the RDA does not provide “extra” bone protection.[12]
- Staying active, especially doing weight-bearing exercise, can help maintain healthy bones along with good calcium intake.
- Like any other nutrient, sourcing our vitamins and minerals from food first, before any supplement, is always best.
However, if your diet alone is not sufficient, then it may be worth talking to a health professional about supplementing.
Related Questions
1. Can calcium supplements cause stomach pain?
Stomach pain is a common side effect of taking calcium supplements and can be a sign that your intake is too high.
2. Is calcium good for menopause hot flashes?
While there has been some evidence that calcium supplements can help with PMS symptoms, this may not necessarily be the case for everyone.
RELATED — Menopause: How to deal with Hot Flushes
3. Should you take vitamin D and calcium together?
Vitamin D helps with calcium absorption, so it is recommended to take these supplements together (if the calcium supplement doesn’t already have vitamin D added to it).
RELATED — Vitamin D: The sunshine hormone for stronger bones
If you have any questions about calcium supplements or getting enough calcium from your current diet, please let us know in the comments, and we’ll share additional information and point you in the right direction.
Having passion for mental health and nutrition, Carly’s goal is to become a registered psychologist with a focus on self-care – food, exercise, and sleep. She has a special interest in various mental health disorders, plant-based diets, and the relationship between food and mood.
Through evidence-based research, holistic approach to health and personal experience, Carly hopes to empower others’ well-being.
Carly is a part of the Content Team that brings you the latest research at D’Connect.
References
(1) Nutrition Foundation. Calcium. 2018 . Accessed 28/2/22; Retrieved from https://nutritionfoundation.org.nz/nutrition-facts/minerals/calcium.
(2) Beto, J.A., The role of calcium in human aging. Clinical nutrition research, 2015. 4(1): p. 1-8. Available from https://doi.org/10.7762/cnr.2015.4.1.1
(3) Health Navigator. Calcium. 2021 11.11.21; Available from https://www.healthnavigator.org.nz/healthy-living/c/calcium/.
(4) Times of India. Common signs and symptoms of calcium deficiency. 2021 Accessed 28/02/22; Retrieved from https://timesofindia.indiatimes.com/life-style/health-fitness/health-news/common-signs-and-symptoms-of-calcium-deficiency/photostory/87332132.cms.
(5) Harvard Health Publishing. 2020. Accessed 28/02/22; Retrieved from https://www.health.harvard.edu/nutrition/choosing-a-calcium-supplement.
(6) PPT Health. Types of Calcium Supplements Matter! 2022. Accessed 03/04/22; Retrieved from https://www.ppt-health.com/osteoarthritis/types-of-calcium-supplements-matter/.
(7) AlgaeCal. Types of Calcium Used in Food Supplements. 2022. Accessed 03/04/22; Retrieved from https://www.algaecal.com/calcium/types/.
(8) Robinson R (2010) Structure of Signaling Enzyme Reveals How Calcium Turns It On. PLoS Biol 8(7): e1000427. Retrieved from https://doi.org/10.1371/journal.pbio.1000427
(9) Harvard School of Public Health. The Nutrition Source – Calcium. 2022. Accessed 15/03/22; Retrieved from https://www.hsph.harvard.edu/nutritionsource/calcium/#:~:text=Calcium%20is%20a%20mineral%20most,heart%20rhythms%20and%20nerve%20functions.
(10) Bae, Y.-J. and S.-K. Kim, Low dietary calcium is associated with self-rated depression in middle-aged Korean women. Nutrition research and practice, 2012. 6(6): p. 527-533. Retrieved from 10.4162/nrp.2012.6.6.527
(11) Ahn, C., J.-H. Kang, and E.-B. Jeung, Calcium homeostasis in diabetes mellitus. Journal of veterinary science, 2017. 18(3): p. 261-266. Retrieved from 10.4142/jvs.2017.18.3.261
(12) Mayo Clinic. Calcium and calcium supplements: Achieving the right balance. 2022. Accessed 11/03/22; Retrieved from https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/calcium-supplements/art-20047097






