
Chris Veitch
PhD Physiology, BBiomedSc (Hons)
Jump to:
Apart from effects on our heart and brain, sleep also has significant impacts on hormonal levels throughout the body.
This article highlights some of the effects that both a full night’s sleep and a short nap can have on some long-lasting hormonal systems.
Power Naps and Stress Hormones
Aside from nocturnal sleep, short power naps appear to have benefits on hormones commonly associated with stress such as
- cortisol
- epinephrine
- norepinephrine
Napping participants have been noted to have significantly decreased levels of cortisol and markers of inflammation during a nap, after these showed an increase due to sleep restriction.[1]
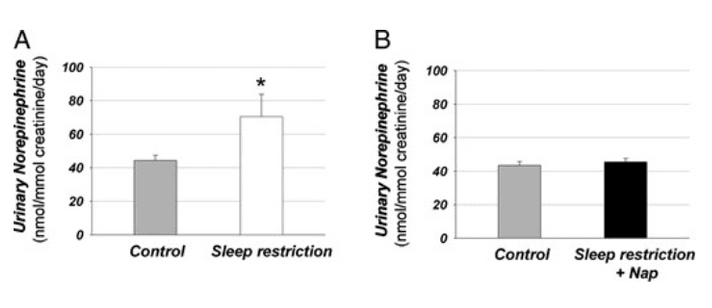
Another study also showed similar decreases in markers of inflammation following two 30-minute naps during the day after a night of sleep restriction, alongside a decrease in levels of norepinephrine, a marker of stress.[2]
A nap can reduce levels of cortisol and norepinephrine
Also, having a nap alongside sleep restriction was able to reduce levels of norepinephrine to similar levels as seen in individuals who had no sleep restriction. This suggests that having a nap or two following a night of poor sleep may be able to reduce the impact of hormonal stress on the body.
This change in cortisol levels also appears to be quite dynamic, with increased levels of cortisol following a nap associated with increased levels of both alertness and improved reaction times.[3]
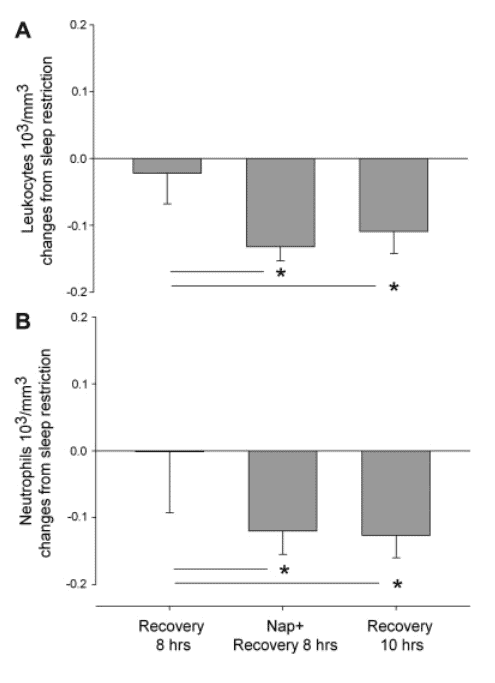
Daytime naps following sleep restriction appear to be able to improve immune function to a similar extent as a full 10 hour night of recovery sleep.
In a 2011 study, participants either had
- 8 hour recovery sleep
- 8 hour recovery sleep and a 30 minute nap
- 10 hour recovery sleep following their sleep restricted night of 2 hours[4]
Participants who napped showed similar decreases in immune cell count as the 10 hour recovery sleep, indicating that just the simple incorporation of a 30-minute nap is able to have similar effects of an extra 2 hours of nocturnal recovery sleep.[4]
Reduction in these cell levels indicate a return to pre-sleep restriction immune system functioning. These researchers also found that following the nap, salivary cortisol levels were reduced compared to those who did not nap.[4]
Hormones such as norepinephrine are known to increase during times of sleep restriction, with researchers suggesting that slow-wave sleep is interacting with the release of norepinephrine, causing a drop during sleep.[5]
This could lead to cardiac complications, as raised levels of norepinephrine are thought to increase risk of conditions such as heart attacks.
Napping might even be a good strategy to combat chronic sleep restriction, or sleep debt.
Individuals subjected to 6 nights of sleep restricted to 4 hours per night showed significant alterations to both metabolism and endocrine function.[6]
These participants exhibited
- impaired glucose metabolism
- raised cortisol levels
- increased activity of the sympathetic nervous system[6]
Based on the findings of the above studies, a short daytime nap may be able to help combat chronic sleep restriction and its impacts on the hormonal health of the body.
These hormonal changes may even be impacted by the environment in which we sleep, as a review examining children napping at either daycare or at home showed that children who napped at daycare didn’t experience the same decrease in cortisol levels that a home nap did.[7]
The researchers suggest that the daycare environment could be influencing these cortisol levels apart from the unfamiliarity of daycare compared to home. Waking up from a nap is often followed by resuming physical activity and social interactions, which could be increasing the levels of cortisol in these children.
We might even be able to manipulate these changes in hormonal levels to our advantage in stressful situations.
Researchers in a 2022 study exposed individuals to a stressor (being instructed to prepare a speech on a topic unknown to them), and then either napped or stayed awake.
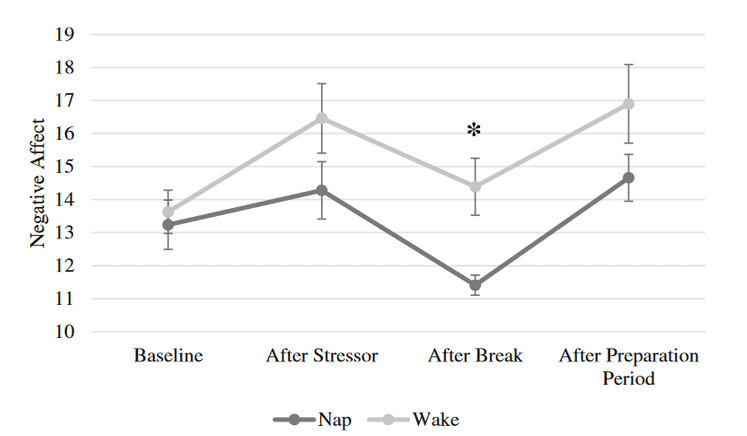
At the end of the study, participants who napped exhibited a significantly decreased negative mood compared to those who didn’t nap.[8]
Power Naps and Growth Hormone
Growth hormone is integrally important for regulating growth and metabolism within the human body.
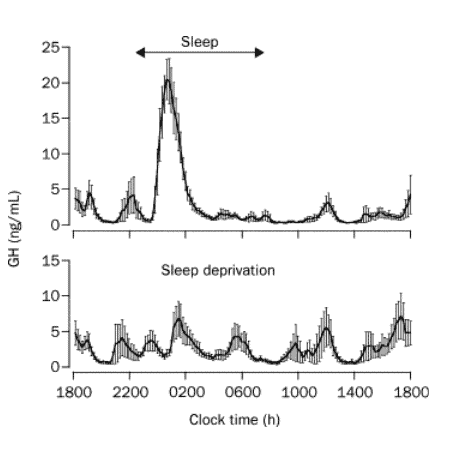
Research shows that it appears to be interlinked with sleep, as this is a time when significant levels of growth hormone are secreted by the body. Growth hormone appears to be most associated in adults with the first cycle of slow wave a.k.a deep sleep.[9]
Growth hormone is important for deep sleep
Given the important impacts of growth hormone on development, it has been thought that this is an important reason for children to get adequate sleep each night.
Studies of children suffering from Growth Hormone Deficiency (GHD) have shown that this can alter sleep structure and quality in children, with limited data showing that treating these children with growth hormone may be able to improve sleep quality.[10]
Interestingly, a study examining sleep restriction showed that young adults who were completely sleep restricted showed compensated levels of growth hormone secretion throughout the day.
This resulted in a not-significantly different level of total growth hormone secretion between those who were sleep restricted, and those who weren’t.[11]
It should be noted that this study was done in adults, not children, so it is hard to say whether children’s growth hormone secretion would compensate in a similar way.
Growth hormone secretion also appears to depend on what time of day a nap occurs. Subjects who napped during the afternoon (4pm-6pm) showed a significantly greater release of GH than subjects who napped in the morning (8am-10am).
Afternoon nap causes a high release of growth hormone than a morning nap
This seemed to correlate with greater amounts of slow-wave sleep (deep sleep) being seen in the group who napped during the afternoon.[12]
Power Naps and Insulin
Sleep has a significant role in regulating levels of insulin, a hormone responsible for sugar uptake. Developing a long-term resistance to insulin is known to lead to Type 2 Diabetes Mellitus.
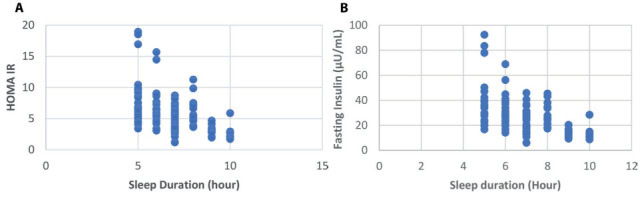
Short sleep duration (<7 hrs a day) was shown to be associated with developing insulin resistance, in a systematic review comprising 10 independent research studies.[13]
Short sleep duration is associated with developing insulin resistance
This association has also been seen in other independent studies, which showed that sleeping >8 hrs was associated with significantly lower levels of HbA1C (a marker of blood sugar levels), compared to those who slept between 6-8 hrs.[14]
This relationship appears to extend to earlier in life as well, with adolescents showing a strong relationship with shorter sleep duration and insulin resistance. Insulin levels were significantly higher in adolescents who slept <8 hrs per night, compared to those who slept >8 hrs.[15]
Less significant loss of sleep for longer periods of time appears to have similar impacts on insulin resistance. In a 6-week timeframe, adults had their sleep restricted to 6.2 hrs per night, mimicking the median sleep duration of US adults who were classed as having a short sleep duration.
This resulted in impaired insulin sensitivity, suggesting that long-term mild sleep deprivation could lead to insulin resistance.[16]
Interestingly, in individuals who already have type 2 diabetes, longer nap duration could influence the management of diabetes and blood sugar levels. Researchers found that type 2 diabetics who napped in the morning or for >60 minutes were more likely to have poor control of blood sugar.[17]
Power-naps as opposed to longer naps may also be a great way to incorporate napping, without increasing the risk of insulin resistance.
A 2024 review article examined nap duration and its effect on the development of type 2 diabetes. It was found that napping for <30 minutes did not increase the risk of type 2 diabetes, whilst napping >30 minutes increased the risk of developing type 2 diabetes by 8-21%.[18]
The authors suggest that longer naps might impact the quality of nocturnal sleep, leading to increased risk of type 2 diabetes.
Power Naps and Ghrelin & Leptin
Along with impacts on insulin, lack of sleep affects our bodies hormones associated with metabolism, such as
- ghrelin (a hormone stimulating hunger)
- leptin (a hormone signalling fullness)
Short sleep duration (<8 hrs per night) is significantly associated with reduced levels of leptin and increased levels of ghrelin.
This suggests that these individuals would have an increased appetite, which is further supported by the association of increased BMI with short sleep duration.[19]
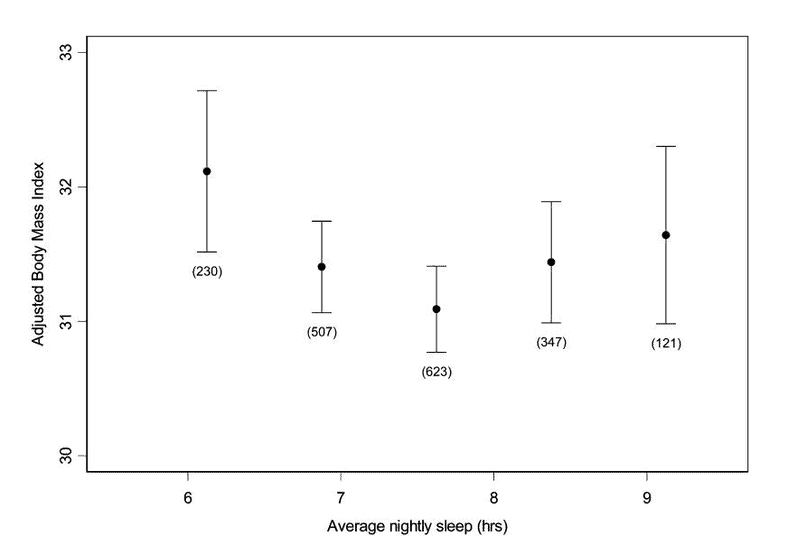
This association appears to affect self-reported appetite, with individuals who had 2 nights of only 4 hours in bed exhibited increased hunger, appetite and ghrelin, along with a decrease in leptin compared to those who had 2 nights of 10 hours in bed.[20]
Further studies have shown that sleep deprivation is associated with obesity, which itself is associated with obstructive sleep apnea.
RELATED — Sleep apnea: How to cure it and get your sleep back
The authors suggest that alongside treating obstructive sleep apnea, increasing sleep duration may be able to prevent the further progression of obesity, which may prevent sleep apnea from growing in severity.[21]
Power Naps and Testosterone
Sleep is also important for levels of testosterone, with its production being linked to the duration of slow wave/deep sleep.
There is some suggestion that lower testosterone levels are linked to worse sleep quality, although the research surrounding this is still unclear.[22]
Testosterone does seem to impact the timing of sleep/circadian rhythms, with rats lacking the ability to produce testosterone showing an almost complete lack of usual night-time behaviour.
Studies have shown that obstructive sleep apnea (OSA) is associated with lower levels of testosterone, however, high doses of testosterone appear to be able to induce OSA, although this may be a short-term effect.[23]
Regardless of the lack of clarity within the research for the exact effects of testosterone on sleep, it is documented that sleep deprivation does significantly reduce levels of testosterone in males. Curiously, this effect only seems to occur within full sleep deprivation as opposed to partial sleep deprivation (~4 hrs a night).[24]
Sleep deprivation significantly reduces levels of testosterone in men
Daytime naps also increase levels of testosterone leading to other positive effects, such as increased bone density and a decreased risk of developing osteoporosis.[25]
Researchers found that daytime naps increased bone mineral density in both the femoral neck and lumbar spine, two key bone structures in the lower body.
This was associated with increased levels of testosterone throughout the body, which appeared to reduce the risk of osteoporosis.[25]
Power Naps and Progesterone
Progesterone, an important hormone within the menstrual cycle appears to also have measurable impacts on sleep.
Studies in adult women tend to show the most sleep disturbances occurring in the last premenstrual days of their cycle, and the first few menstrual days.[26]
This coincides with a significant drop in the levels of estrogen and progesterone.
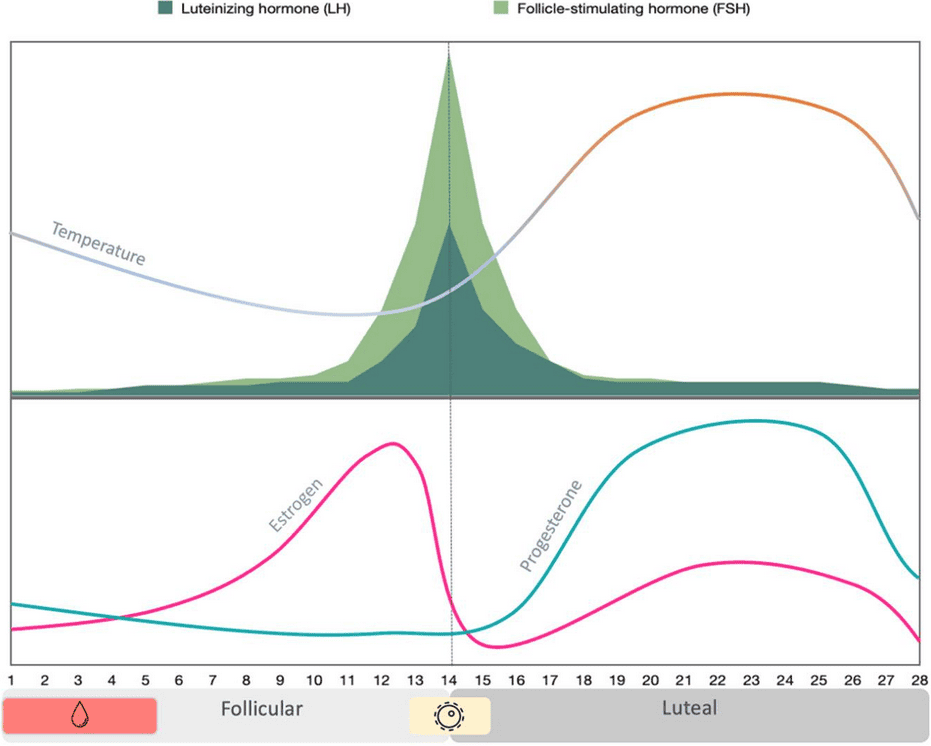
Alongside these reports, progesterone has been shown to have sleep inducing effects in healthy male subjects, along with a significant increase in the amount of non-REM sleep.[27]
Treatment of post-menopausal women with progesterone has even been shown to reduce mild OSA, suggesting that progesterone might protect pre-menopausal women from developing OSA.[27]
Women taking progesterone also exhibit greater levels of sleep spindles than those not taking progesterone.[28]
Sleep spindles are thought to be an important marker of memory consolidation during sleep, and could play a role in learning pathways.
Conclusion
The above studies show that both night-time sleep and power-naps have the ability to significantly impact your endocrine system.
Having good quality sleep could have long-lasting impacts on your hormonal systems, which may prevent the development of disease long-term.
Overall, sleep no matter the duration is much more likely to have a positive influence on your endocrine system than negative.
The next time you feel strung-out or stressed, perhaps increasing your time in bed or a power-nap could be just what you need?
RELATED — Power Naps and Brain Health
Chris is currently working as a clinical physiologist, specialising in sleep medicine. He is also currently studying towards his Postgraduate Diploma in Medical Technology endorsed in sleep medicine…
If you would like to learn more about Chris, see Expert: Chris Veitch.
References
(1) Vgontzas, A. N., Pejovic, S., Zoumakis, E., Lin, H. M., Bixler, E. O., Basta, M., Fang, J., Sarrigiannidis, A., & Chrousos, G. P. (2007). Daytime napping after a night of sleep loss decreases sleepiness, improves performance, and causes beneficial changes in cortisol and interleukin-6 secretion. American Journal of Physiology – Endocrinology and Metabolism. https://journals.physiology.org/toc/ajpendo/292/1
(2) Faraut, B., Nakib, S., Drogou, C., Elbaz, M., Sauvet, F., Bandt, J-P. D., & Léger, D. (2015). Napping Reverses the Salivary Interleukin-6 and Urinary Norepinephrine Changes Induced by Sleep Restriction. The Journal of Clinical Endocrinology & Metabolism.
(3) Lou, S., Hu, S., Chen, Y., Zhao, K., Zhou, Y., Hou, J., Liang, L., & Sun, H. (2024). Benefits of napping habits in healthy adults: Maintaining alerting performance and cortisol levels change within 90min of habitual napping time. Sleep Medicine.
(4) Faraut, B., Boudjeltia, K. Z., Dyzma, M., Rousseau, A., David, E., Stenuit, P., Franck, T., Antwerpen, P. V., Vanhaeverbeek, M., & Kerkhofs, M. (2011). Benefits of napping and an extended duration of recovery sleep on alertness and immune cells after acute sleep restriction. Brain, Behaviour, and Immunity.
(5) Irwin, M., Thompson, J., Miller, C., Gillin, J. C., & Ziegler, M. (1999). Effects of sleep and sleep deprivation on catecholamine and interleukin-2 levels in humans: clinical implications. The Journal of Clinical Endocrinology and Metabolism.
(6) Spiegel, K., Leproult, R., & Van Cauter, E. (1999). Impact of sleep debt on metabolic and endocrine function. Lancet.
(7) Mesas, A. E., Sánchez-López, M., Pozuelo-Carrascosa, D. P., Sequí-Domínguez, I., Jiménez-López, E., & Martínez-Vizcaíno, V. (2022). The role of daytime napping on salivary cortisol in children aged 0-5 years: a systematic review and meta-analysis. European Journal of Pediatrics.
(8) Wofford, N., Ceballos, N., Elkins, G., & Westerburg, C. E. (2022). A brief nap during an acute stressor improves negative affect. Journal of Sleep Research. https://pmc.ncbi.nlm.nih.gov/articles/PMC9786543/
(9) Van Cauter, E., & Plat, L. (1996). Physiology of growth hormone secretion during sleep. The Journal of Pediatrics.
(10) Zaffanello, M., Pietrobelli, A., Cavarzere, P., Guzzo, A., & Antoniazzi, F. (2024). Complex relationship between growth hormone and sleep in children: insights, discrepancies, and implications. Frontiers in Endocrinology. https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1332114/full
(11) Brandenberger, G., Gronfier, C., Chapotot, F., Simon, C., & Piquard, F. (2000). Effect of sleep deprivation on overall 24 h growth-hormone secretion. Lancet.
(12) Karacan, I., Rosenbloom, A. L., Londono, J. H., Williams, R. L., & Salis, P. J. (1974). Growth hormone levels during morning and afternoon naps. Behavioural Neuropsychiatry.
(13) Singh, T., Ahmed, T. A., Mohamed, N., Elhaj, M. S., Mohammed, Z., Paulsingh, C. N., Mohamed, M. B., & Khan, S. (2022). Does Insufficient Sleep Increase the Risk of Developing Insulin Resistance: A Systematic Review. Cureus. https://pmc.ncbi.nlm.nih.gov/articles/PMC9036496/
(14) Baoying, H., Hongjie, C., Changsheng, Q., Peijian, W., Qingfei, L., Yinghua, L., Huibin, H., Jixing, L., Liantao, L., Ling, C., Kaka, T., Zichun, C., Lixiang, L., Jieli, L., Yufang, B., Guang, N., Penli, Z., Junping, W., & Gang, C. (2014) Association of napping and night-time sleep with impaired glucose regulation, insulin resistance and glycated haemoglobin in Chinese middle-aged adults with no diabetes: a cross-sectional study. BMJ Open. https://pmc.ncbi.nlm.nih.gov/articles/PMC4120253/
(15) Widjaja, N. A., Kurube, C. F., & Ardianah, E. (2023). Sleep duration and insulin resistance in obese adolescents with metabolic syndrome: is there a correlation? Acta Biomedica.
(16) Zuraikat, F. M., Laferrère, B., Cheng, B., Scaccia, S. E., Cui, Z., Aggarwal, B., Jelic, S., & St-Onge, M-P. (2024). Chronic Insufficient Sleep in Women Impairs Insulin Sensitivity Independent of Adiposity Changes: Results of a Randomized Trial. Diabetes Care.
(17) Yuan, J., Wang, J., Chen, Y., Zhang, M., Zhao, A., Du, J., Zhang, J., Liu, F., Wang, Y., Chen, P., & Zhu, B. (2024). The relationship between daytime napping and glycemic control in people with type 2 diabetes. Frontiers in Endocrinology. https://pmc.ncbi.nlm.nih.gov/articles/PMC10948433/
(18) Liu, H., Wu, Y., Zhu, H., Wang, P., Chen, T., Xia, A., Zhao, Z., He, D., Chen, X., Xu, J., & Ji, L. (2024). Association between napping and type 2 diabetes mellitus. Frontiers in Endocrinology. https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1294638/full
(19) Taheri, S., Lin, L., Austin, D., Young, T., & Mignot, E. (2004). Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLOS Medicine.
(20) Spiegel, K., Tasali, E., Penev, P., & Van Cauter, E. (2004). Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Annals of Internal Medicine.
(21) Kurnool, S., McCowen, K. C., Bernstein, N. A., & Malhotra, A. (2023). Sleep Apnea, Obesity, and Diabetes – an Intertwined Trio. Current Diabetes Reports. https://pmc.ncbi.nlm.nih.gov/articles/PMC10239381/
(22) Wittert, G. (2014). The relationship between sleep disorders and testosterone. Current Opinion in Endocrinology, Diabetes and Obesity.
(23) Liu, P. Y., & Reddy, R. T. (2022). Sleep, testosterone and cortisol balance, and ageing men. Reviews in Endocrine and Metabolic Disorders.
(24) Su, Liang., Zhang, S-Z., Zhu, J., Wu, J., & Jiao, Y-Z. (2021). Effect of partial and total sleep deprivation on serum testosterone in healthy males: a systematic review and meta-analysis. Sleep Medicine.
(25) Zhang, Y., Jiang, Z., Shang, G., Song, Z., Mao, K., Chen, S., & Liu, H. (2024). Effects of Testosterone in Mediating the Relationship Between Daytime Napping and Osteoporosis in European Populations: A Mendelian Randomization Study. Calcified Tissue International.
(26) Alzueta, E., & Baker, F. C. (2024). The Menstrual Cycle and Sleep. Sleep Medicine Clinics. https://pmc.ncbi.nlm.nih.gov/articles/PMC11562818/
(27) Andersen, M. L., Bittencourt, L. R. A., Antunes, I. B., & Tufik, S. (2006). Effects of progesterone on sleep: a possible pharmacological treatment for sleep-breathing disorders? Current Medicinal Chemistry.
(28) Plante, D. T., & Goldstein, M. R. (2013). Medroxyprogesterone acetate is associated with increased sleep spindles during non-rapid eye movement sleep in women referred for polysomnography. Psychoneuroendocrinology.






