
Beatrice Blanch
(BSc Physiology, PGCertMedTech)
Getting a good night of sleep is sometimes challenging on its own.
Over the last few years, our quality of sleep and sleep hours has decreased and the number of people struggling with low energy and daytime sleepiness has grown proportionally.
Today, we will look into what sleep apnea is , how to know if you have it, and how to resolve it before it causes health issues such as
- Stroke
- Heart failure
- Cardiomyopathy
- Hypertension
- Diabetes
and other conditions.
What is sleep apnea?
Sleep apnea is a disorder characterised by repeated cessations or reductions of airflow while we sleep. These are called apnea and hypopnea events.
The American Academy of Sleep Medicine (AASM) defines apnea as a 90% reduction of airflow compared to baseline for 10 seconds.
Types of sleep apnea
There are three types of sleep apnea:
- Obstructive apnea
- Central apnea
- Mixed apnea
Obstructive sleep apnea (OSA) is the most common type of apnea and is characterised by repeated partial or complete collapse of the upper airway during sleep.
Central sleep apnea occurs when there is a lack of respiratory effort during sleep, which then results in insufficient / decreased airflow.
This is different to obstructive sleep apnea where the input to thoracic muscles are uninterrupted – it’s just the narrowing of the upper airway which causes lack of airflow.[1]
Obstructive sleep apnea is the most common type of apnea
Mixed sleep apnea describes the apnea in patients who predominantly have obstructive sleep apnea, but after being treated with CPAP this becomes central apnea. These patents have a mixture of both obstructive and central sleep apnea.
A hypopnea is defined as a 30% reduction of airflow compared to baseline for 10 seconds with an associated 3% drop of the oxygen saturation in the blood.
A hypopnea is not a type of apnea
Important to mention is that sleep apnea is not made up of “apneas” alone. Sleep apnea is the combination of apneas and hypopneas (AHI) that determines the severity of the sleep apnea.
Sleep apnea statistics
Obstructive sleep apnea is a disorder that is becoming increasingly prevalent, and is estimated to affect 26% of adults in the United States.[2]
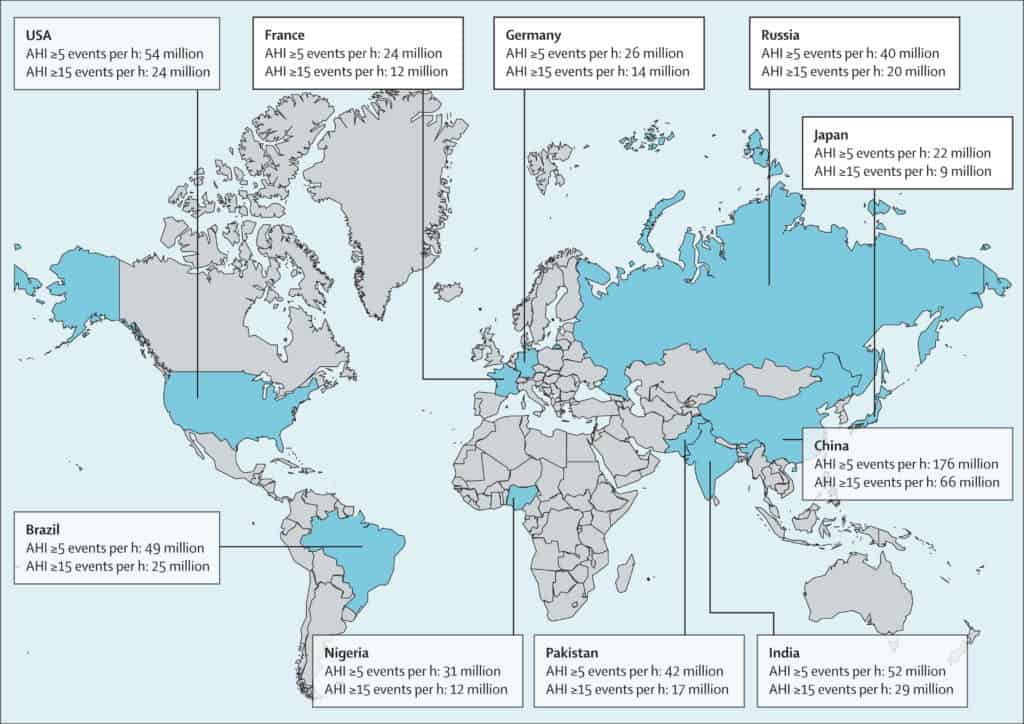
Source: Eastwood, P., R. Estimation of the global prevalence and burden of obstructive sleep apnea: a literature-based analysis. The Lancet - Respiratory Medicine (VOLUME 7, ISSUE 8, P687-698, AUGUST 01, 2019)
Specifically for New Zealand, Mihaere study, published in 2009, estimates that the prevalence of OSA is 22.0% for Māori men, 11.4% for non-Māori men, 6.3% for Māori women, and 3.0% for non-Māori women.[3]
How weight and age affect sleep
The prevalence of obstructive sleep apnea increases with age.
With ageing, there is a loss of tissue elasticity, and this can contribute to an increase in the collapsibility of the upper airway, which can cause obstruction.[4]
The changes and decrease in sex hormones in older women due to menopause is also thought to be responsible for the increase in prevalence of OSA.[5]
RELATED — Menopause Revealed: Signs, Stages, Types and Treatment
Other than age, people who have excessive weight are at the highest risk of developing OSA. The excess weight around the neck and upper body has a high chance of causing the upper airway to narrow during sleep, and therefore prevent the flow of air into the airways.
60% - 90% of people with obstructive sleep apnea are overweight
Further more, the studies show that 50%-80% of clinically obese patients have OSA.[6]
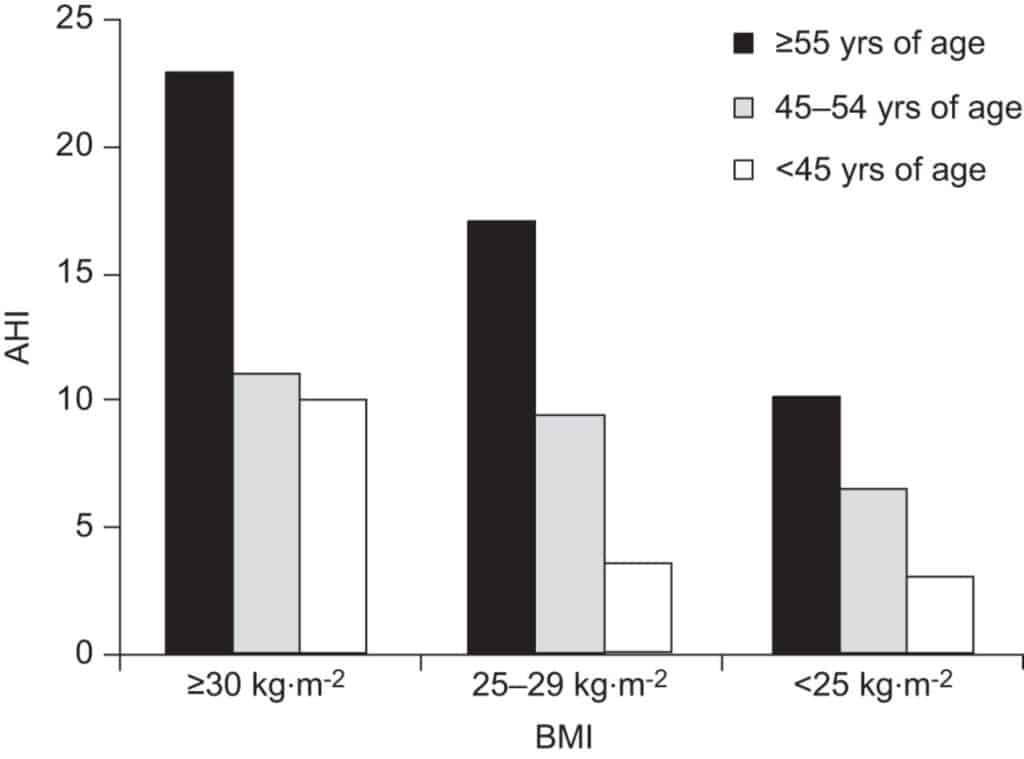
Source: Franklin, K., A. Sleep apnea is a common occurrence in females. European Respiratory Journal. 2013.
Weight loss and reduction in sleep apnea
Weigh loss or bariatric surgery is always advised to obese patients who are diagnosed with OSA, as losing excess weight can drastically improve and even eliminate the disorder.
A study published in 2016 found a significant relationship between increased body weight and an increase in hypopneas (AHI). A man with OSA was monitored five times in three years as his weight changed within a 26 kg range.
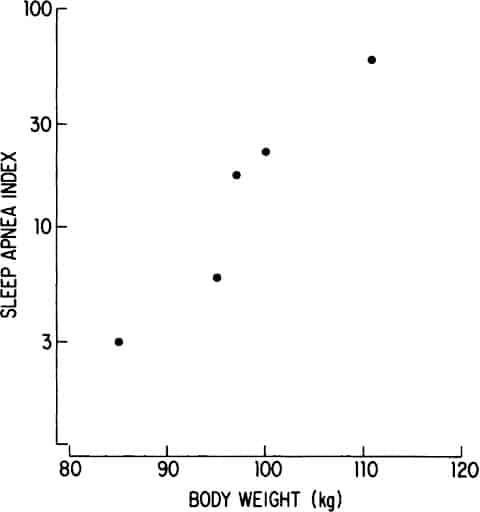
At his heaviest weight (111 kg), he had an AHI of 59.6 events per hour, and at his lightest weight (85 kg), this decreased to 3.1 events per hour.[7]
How sleep apnea is diagnosed
Many people who have a sleep study done are referred by their GP after complaining of excessive sleepiness during the daytime, or inability to focus during work.
In other cases, a person might have stayed in the hospital overnight for another treatment, and either the nurses or surgeons during the operation witnessed apneas occurring.
In both cases, the person is referred to a specialist sleep doctor who reviews their case and decides which type of sleep study/test is appropriate for them.
Sleep apnea tests and sleep studies
The severity of sleep apnea is calculated by the apnea hypopnea index (AHI) – this is the sum of the number of apnea and hypopnea events that occur per hour of sleep.[8]
Sleep apnea is diagnosed if AHI is greater than 5
Adult AHI | Pediatric AHI | |
Mild OSA | ≥ 5 to < 15 events per hour | ≥ 1 to ≤ 5 events per hour |
Moderate OSA | ≥ 5 to < 30 events per hour | > 5 to ≤ 10 events per hour |
Severe OSA | ≥ 30 events per hour | > 10 events per hour |
The diagnostic criteria for sleep apnea is an AHI greater than 5 events per hour. This diagnosis is most commonly done after an overnight sleep study.
There are different types of sleep studies (Level 1 to Level 4) with different physiological parameters being measured depending on the type of sleep study being done.
Level 1 sleep study
A level 1 sleep study, otherwise known as polysomnography (PSG), requires the patient to stay overnight at a sleep laboratory and be attended and supervised by sleep technicians.
This type of study involves recording many channels of data, such as
- Neurological waves
- Respiratory pattern and effort
- Muscular tone
- Cardiovascular trace
to create a picture of the person’s sleep pattern.
A level 1 sleep study is the standard for being able to diagnose many different types of breathing and sleep disorders. It is particularly useful because the technicians are able to monitor
- patient’s oxygen saturations
- number of apnea and hypopnea events
that occur during the night while they are happening so if the person has severe OSA they can be diagnosed the next day and discharged from the hospital with treatment.[9]
Level 2 sleep study
A level 2 sleep study measures the same parameters as level 1, with the same equipment, but the equipment is portable and the study is done unattended. This means it can be done at home.
Level 3 sleep study
Level 3 sleep studies use a portable device and measure fewer parameters, which are usually
- Oxygen levels
- Breathing effort
- Flow rate
- Heart rate
Level 3 sleep studies are the most common home sleep tests
Level 4 sleep study
Level 4 sleep studies also use portable equipment, but measure even less data compared to level 3 – usually only 1 or 2 channels of data.[9]
When the study is done at home (Level 2 to Level 4 studies), the patient returns the sleep study device the next day and the data is downloaded by the sleep technicians and analysed.
Analysis of the sleep study highlights apnea and hypopnea events that occurred during the night, as well as the oxygen desaturations and any other sleep abnormalities.
The AHI is then calculated and a doctor makes a decision on the appropriate treatment.
What are the treatments for sleep apnea?
There are many different treatments that can be used for resolving sleep apneas, but the most common treatment that is usually tried first is a continuous positive airway pressure (CPAP) machine.
Continuous positive airway pressure machine (CPAP)
CPAP treats the disorder by applying positive pressure to the upper airway via a mask worn while asleep. The positive pressure stents the airway open and physically prevents it from closing.
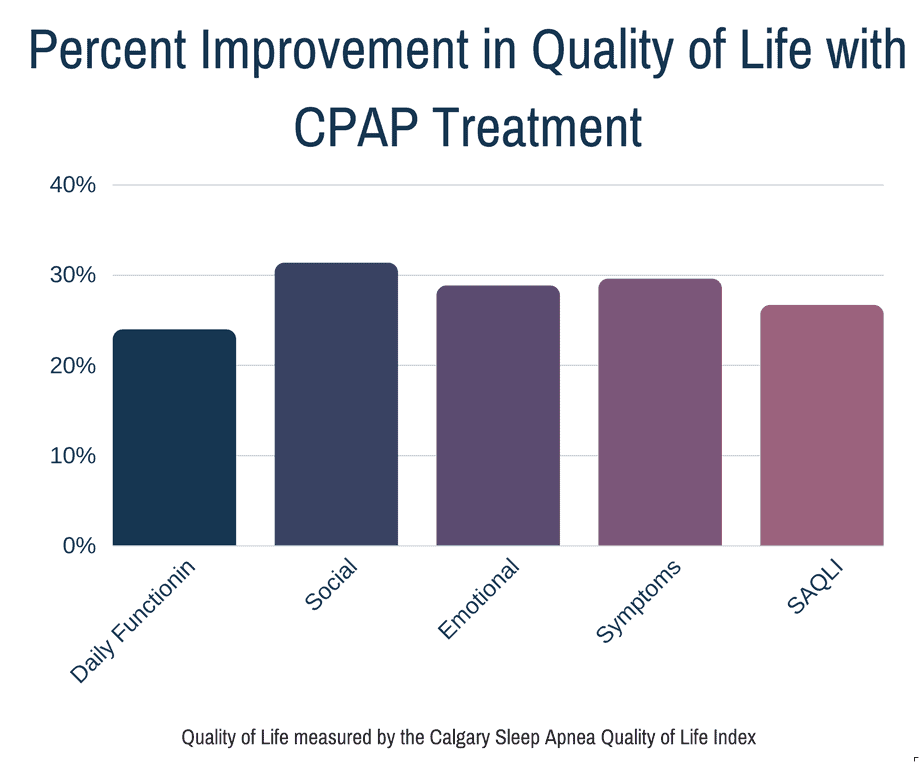
CPAP is the gold standard treatment for obstructive sleep apnea
CPAP has been shown to be the most effective treatment for OSA and has been proven to improve symptoms and associated comorbidities.[10]
Oral appliances for sleep apnea
Oral appliances are dental splints which prevent airway obstruction while sleeping by pushing and maintaining the mandible or tongue in an advanced position. This keeps the upper airway open.
This is the second most popular choice for treatment of sleep apnea, and can even be recommended to patients as the primary therapy or as complementary to CPAP.
Research shows that patients who use two devices on alternate days have been more compliant with the treatment since they have the option to take a break from the “discomfort” of one treatment type.[10]
Bilevel Positive Airway Pressure
Bi-level PAP or BiPAP is a positive pressure machine which delivers two different pressures – an inspiratory pressure and an expiratory pressure.
The inspiratory pressure (IPAP) provides a higher pressure and is delivered when the patient inspires, while the expiratory pressure (EPAP) provides a lower pressure, and is delivered when the patient expires.
The difference between the IPAP and EPAP is called the pressure support, or assist level, and is what makes BiPAP more comfortable.
Some patients who use CPAP find the continuous pressure uncomfortable when they exhale, so BiPAP is supposed to reduce some of the discomfort by reducing the pressure when the patients exhale.[11]
Adaptive servo ventilation
Adaptive servo ventilation (ASV) is another type of ventilatory machine which is more commonly used for patients with central sleep apnea, or complex apnea patients (for example, people with major heart problems).
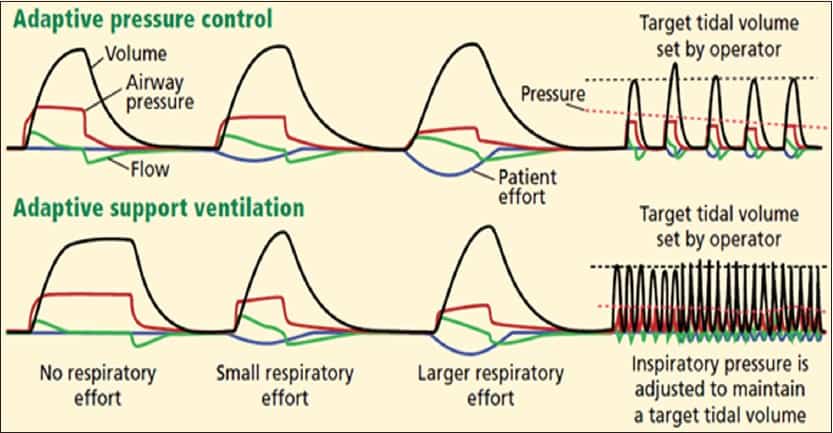
ASV changes the pressure being delivered based on the breathing pattern and blood oxygen levels of the patient. The goal is not only to have consistent breathing, but also maintain oxygen levels above 90%.[12, 13]
Sleep apnea and help through surgery
There are more invasive alternatives to treating sleep apnea and these include undergoing surgery on one of the structures of the upper airway.
Uvulopalatopharyngoplasty (UPPP)
UPPP was the first type of surgery that dealt with palatal abnormalities in patients with obstructive sleep apneas.
Excess tissue is removed during this surgery, and this can include the uvula, part of the soft palate and the pharyngeal pillars. This makes the airway wider and can allow air to move more easily with less obstruction.[10]

Laser-assisted uvulopalatoplasty (LAUP)
LAUP is an outpatient based procedure that is done under local anaesthesia. Here, the uvula and palate are cut and removed through carbon dioxide and laser incisions and vaporisation.
UPPP and LAUP are mostly done on people with mild to moderate obstructive sleep apnea, or when the predominant cause of OSA is known to be oropharyngeal narrowing.[14]
Upper airway stimulation
Upper airway stimulation is another invasive treatment for obstructive sleep apnea.
Upper airway stimulation works by providing phasic stimulation of the hypoglossal nerve via a pulse generator (IPG), which is implanted in the right infraclavicular area.
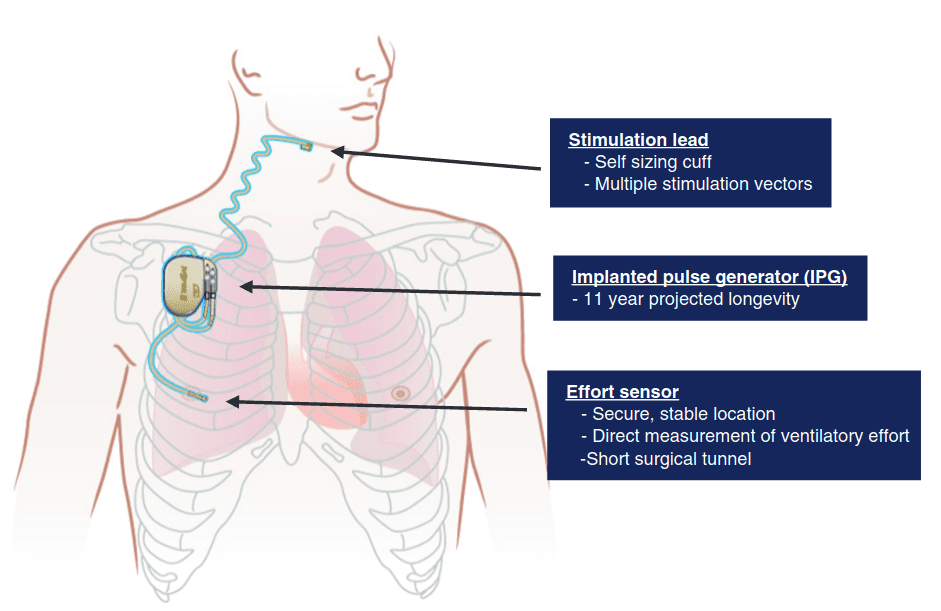
Stimulation of the hypoglossal nerve activates the genioglossus muscle and makes the tongue protrude forward, opening up the upper airway.
The upper airway stimulation device is only applied while the person is sleeping and can be implanted into the person as an outpatient.
The device is only activated 1 month after the operation to allow for proper healing. The voltage that is applied to the nerve is determined through a level 1 sleep study.[15]
Medication for sleep apnea
There are no drugs or medications (yet) that can replace the treatments mentioned, however there are medications that can help with the symptoms of sleep apnea.
Selective serotonin reuptake inhibitor
Selective serotonin reuptake inhibitor (SSRI) is an antidepressant that makes it harder for the brain to go into the stage of sleep called rapid eye movement (REM) sleep.
Obstructive apnea occurs most during REM sleep
Our muscles are most relaxed during REM sleep, including the muscles of our upper airway. SSRIs are thought to increase airway muscle tone, so less obstruction occurs.
RELATED — Different types of sleep: which one do we need the most?
Modafinil and armodafinil
Another common medication prescribed are stimulants such as modafinil and armodafinil. These stimulants help to keep the patient more alert and awake and reduce sleepiness during the daytime.
Daytime sleepiness is a common symptom of sleep apnea
Some people experience a worsening of their sleep apnea at night due to congested nasal passages, so nasal decongestants are also commonly used.[16]
Natural remedies for sleep apnea
Weight loss and sleep apnea
Weight loss is commonly advised to patients with obstructive sleep apnea, and research show that it decreases the severity of OSA in people who are obese.
Although weight reduction is not recommended as a stand alone therapy, it should be done in addition to another treatment.
Alcohol and sleep quality
Alcohol can act as a sedative and cause the upper airway muscles to relax. It can worsen sleep apnea in people who already have OSA, and induce apneas in people who have a snoring history.
It is recommended that people with OSA either abstain from or reduce their alcohol intake, and do not consume alcohol before going to bed.[17]
Smoking, airways and sleep
Smoking cigarettes is thought to increase mucosal edema in the upper airway, resulting in increased upper airway resistance, and possibly contributing to OSA.
Studies have looked at the relationship between smoking cessation and AHI, and findings have varied. However, smoking cessation is always recommended for general health purposes.[17]

Preferred sleep positions for reducing sleep apnea
Certain sleeping positions can help with sleep apnea. Many people who have OSA experience more obstructive events when they are lying in supine position (on their back).
Sleeping in a supine position can cause the tongue to be pushed backwards due to gravity, and can increase the chances of it closing off the upper airway.
Sleeping with the head elevated or sleeping on the side is a strategy to reduce snoring, and can be recommended by clinicians as well for OSA.[17]
Related Questions
1. How long does it take for CPAP to improve sleep apnea?
The benefits of the treatment (feeling more awake and having more energy) should be visible after two weeks.
However, this depends on your adherence to treatment – for example how many hours per night you use the device.[18]
2. Is sleep apnea hereditary?
It is estimated that having sleep apnea due to genetics is around 40%.
Our genes can impact body fat distribution, facial anatomy, breathing control and circadian rhythm, which can all contribute towards sleep apnea.[19]
3. What medications should you avoid if you have sleep apnea?
If you have sleep apnea, you should avoid any muscle relaxing medication such as antihistamines and benzodiazepines. Opioids and barbiturates also have an effect on breathing patterns during sleep and should be avoided.[20]
If you are interested in better sleep, in our next articles we will be talking about different stages of sleep and why they are important. Check in again soon.
Beatrice is currently completing her Postgraduate Diploma in Medical Technology, with an endorsement in Sleep Medicine, and has been fortunate to be working in healthcare in conjunction with her postgraduate studies.
Since starting, Beatrice has seen first-hand the effects of lifestyle on sleep hygiene, and the relationship between poor sleep and preventable chronic diseases. Beatrice aims to use scientific evidence-based research to help educate people on the importance of healthy sleep hygiene so that they may improve the quality of their life.
References
(1) Dempsey JA, Veasey SC, Morgan BJ & O’Donnell CP (2010). Pathophysiology of Sleep Apnea. American Physiological Society 90, 47-112. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3970937/
(2) Santilli M., Manciocchi E., D’Addazio G., Di Maria E., D’Attilio M., Femminella B., & Sinjari, B. (2021). Prevalence of Obstructive Sleep Apnea Syndrome: A Single-Center Retrospective Study. International Journal of Environmental Research and Public Health.
(3) Mihaere KM, Harris R, Gander PH, Reid PM, Purdie G, Robson B, Neill A (2009). Obstructive sleep apnea in New Zealand adults: prevalence and risk factors among Māori and non-Māori. Sleep 32(7), 949-956. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2706899/
(4) Phillips BA (2011). Obstructive Sleep Apnea in the Elderly. Principles and Practice of Sleep Medicine 5, 1536-1550.
(5) Jehan S., Auguste E., Zizi, F., Pandi-Perumal SR., Gupta R., Attarian H., Jean-Louis G., & McFarlane SI. (2016). Obstructive Sleep Apnea: Women’s Perspective. Journal of sleep medicine and disorders, 3(6), 1064. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5323064/
(6) Olson EJ, Courcoulas AP (2011). Obstructive Sleep Apnea, Obesity, and Bariatric Surgery. Principles and Practice of Sleep Medicine 5, 1339-1348.
(7) Browman CP, Sampson MG, Yolles SF, Gujavarty KS, Weiler SJ, Walsleben JA, Hahn PM, Mitler MM (2016). Obstructive Sleep Apnea and Body Weight. Chest (85)3, 435-436.
(8) Berry RB; Budhiraja R; Gottlieb DJ; Gozal D; Iber C; Kapur VK; Marcus CL; Mehra R; Parthasarathy S; Quan SF; Redline S; Strohl KP; Ward SLD; & Tangredi MM (2012). Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Journal of Clinical Sleep Medicine 8(5), 597-619. Retrieved from https://jcsm.aasm.org/doi/10.5664/jcsm.2172#d3e533
(9) El Shayeb M, Topfer L-A, Stafinski T, Pawluk L & Menon D (2014). Diagnostic accuracy of level 3 portable sleep tests versus level 1 polysomnography for sleep-disordered breathing: a systematic review and meta-analysis. Canadian Medical Association Journal 186, E25–E51.
(10) Lorenzi-Filho G, Almeida FR & Strollo PJ (2017). Treating OSA: Current and emerging therapies beyond CPAP. Respirology 22, 1500–1507.
(11) Antonescu-Turcu, A., & Parthasarathy, S. (2010). CPAP and bi-level PAP therapy: new and established roles. Respiratory care, 55(9), 1216–1229. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3119924/
(12) Cantero, C., Adler, D., Pasquina, P., Uldry, C., Egger, B., Prella, M., Younossian, A. B., Poncet, A., Soccal-Gasche, P., Pepin, J. L., & Janssens, J. P. (2020). Adaptive Servo-Ventilation: A Comprehensive Descriptive Study in the Geneva Lake Area. Frontiers in medicine, 7, 105. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7145945/
(13) Asp K. Difference between APAP, BiPAP, CPAP and ASV. Sleep resolutions. Retrieved from https://www.sleepresolutions.com/blog/difference-between-apap-bipap-cpap-and-asv
(14) Randerath WJ, Verbraecken J, Andreas S, Bettega G, Boudewyns A, Hamans E, Jalbert F, Paoli JR, Sanner B, Smith I, Stuck BA, Lacassagne L, Marklund M, Maurer JT, Pepin JL, Valipour A, Verse T & Fietze I (2011). Non-CPAP therapies in obstructive sleep apnoea. European Respiratory Journal 37, 1000–1028.
(15) Walker RP, Grigg-Damberger MM & Gopalsami C (1997). Uvulopalatopharyngoplasty Versus Laser-Assisted Uvulopalatoplasty for the Treatment of Obstructive Sleep Apnea. The Laryngoscope 107, 76–82.
(16) Booth S (2021). Can Medications Help With Sleep Apnea? WebMD. Retrieved from https://www.webmd.com/sleep-disorders/sleep-apnea/sleep-apnea-can-medications-help
(17) Atwood Jr. CW, Strollo Jr. PJ, Givelber R (2011). Medical Therapy for Obstructive Sleep Apnea. Principles and Practice of Sleep Medicine 5, 1219-1232.
(18) Resmed.com. What is CPAP therapy? Retrieved from https://www.resmed.com.au/cpap
(19) Summer J (2022). Is Sleep Apnea Genetic? Sleep Foundation. Retrieved from https://www.sleepfoundation.org/sleep-apnea
(20) Peters B (2022). Can Medication Cause Sleep Apnea? Very Well Health. Retrieved from https://www.verywellhealth.com/how-medications-may-affect-sleep-apnea-3014683




