
Rahle Dusheiko
Level 2 Iyengar Yoga Teacher, Life Coach (SWITCH Method)
As we age, our risk of falling and the potential for severe injuries increases significantly.
What if there were ways we could decrease this risk?
What if there were steps we could take to not only reduce the risk of falling, but improve our mobility and quality of life?
This article looks at statistics around falling and the impact this has on seniors, and provides simple balance exercises and strategies that are crucial for maintaining mobility and independence in older adults.
Seniors, falling and statistics
In 2018, New Zealand reported 1 in 3 people over 65 are injured from falls annually. This number increases to 2 in 3 people once they reach 80.[1] Across the Tasman, our neighbours, Australia, report 30% of people aged over 65 fall each year.[2]
Globally, falls are a significant health concern with approximately 28-35% of individuals aged 65 and over experiencing falls and 32-42% for those over 70 years of age.[3]
The United States also reports a significant high fall rate with 1 in 4 adults over 65.[4] Given these statistics, it’s clear that falls are a major health risk affecting the quality of life and lead to accidental deaths in the aged population.
As we get older our risk of falling dramatically increases
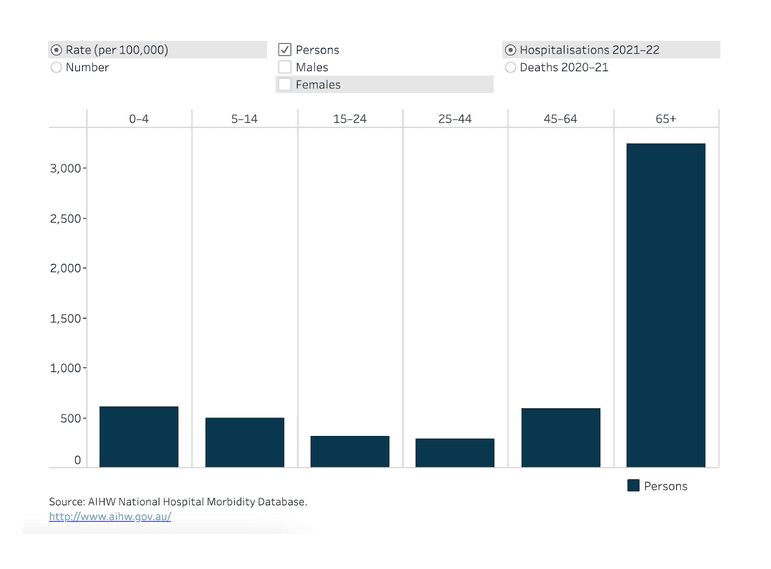
In this graph below, we can see clearly the elevated risk of hospitalisations from falls in seniors over 65 years of age (in Australia).[5]
The factors of the individual that contribute to the risk of falls among seniors, include:
- muscle weakness
- balance issues
- vision problems
- certain medications that affect balance and coordination
- inappropriate footwear
There are other factors that increase the risk of falls such as environmental conditions such as uneven surfaces, rugs and slippery floors. Other factors could be from excessive alcohol consumption, physical and cognitive decline and socioeconomic factors.
In New Zealand, 1 in 3 people over 65 fall annually.
In the LiLACS NZ study, it was found that 37% of the elderly surveyed had fallen over the past year, what’s more, 20% of those who fell needed hospital care due to their injuries.
Additionally, these falls were not a once-off incident; a significant number of individuals experienced multiple falls within the same year.[5]
Risks of falling in seniors
There are fatal and non-fatal risks associated with falling in seniors, most falls will require medical attention and possibly a hospital stay if it is more serious.
Here is a list of some of the most common risks associated with falls.
Fractures
The most common fractures from falls are the:
- hip
- thigh
- forearm
- pelvis
- thorax (rib area)
- knee[6]
Fracturing any of these can lead to severe health and lifestyle implications. The table below illustrates that the hip and thigh are the most fractured body region area across almost all age groups over 65.
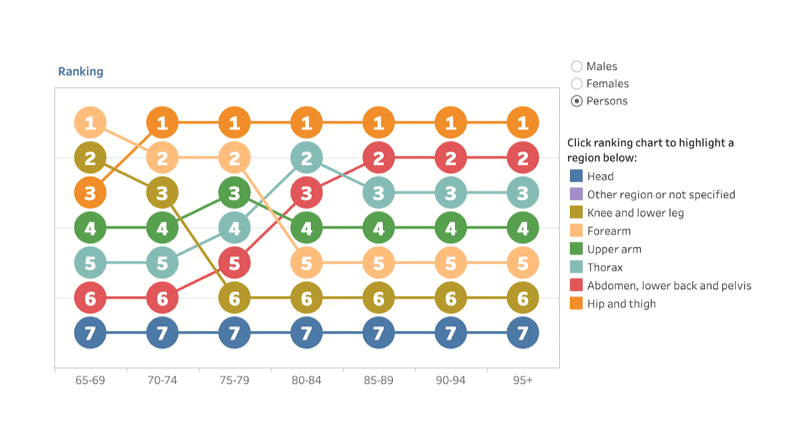
Source: Australian Institute of Health and Welfare.
Hip fractures are particularly serious and can lead to a loss of independence, decreased mobility, long term disability and increased mortality.[7]
Some studies have shown that up to 20% of seniors who fall and sustain a hip fracture, die within a year, while others face long-term care and possibly permanent disability.[8]
The implications and burden have far-reaching societal and financial impact, which stresses how important preventative measures and effective healthcare strategies are.
Whether someone lives at home, independently or in a facility, strategies are vital to prevent falls.
Head injuries
Head injuries from falls can be life threatening. Falls can lead to traumatic brain injuries and concussions, which pose severe risks for seniors, and can potentially lead to fatal outcomes or long-term, negative cognitive effects.
The Centers for Disease Control and Prevention (CDC) report that falls are the most common cause of traumatic brain injuries (TBI) among the elderly. The agency highlights the importance of addressing risk factors and preventive measures to reduce these injuries.[9]
We don’t need to be knocked out or even hit on the head directly to experience a brain injury. If we have had a low-level or same-level fall, it’s still possible to have a brain injury.
Older people that suffer a brain injury have an increased risk of cognitive decline, will take longer to recover and there could be worse consequences.
Two thirds of older adults completely recover from a mild brain injury
However, older adults who are frail, that have been diagnosed with dementia, cancer or who have a history of antithrombotic therapy are the most at risk for a poor recovery. If there has been a fall, you should always refer to your doctor for an assessment.
Reduced Mobility, Loss of Confidence and Isolation
After someone has experienced a fall, there is often a fear of falling and drop in confidence which also leads them to being less active.
Being less active, to avoid falling, can lead to a further health decline and creates a negative cycle because the person may avoid everyday activities.
This means the muscles become weaker, the person becomes more unstable which then increases their risk of falling.
A loss of confidence and decreased activity after a fall can also cause social isolation, which is another negative impact of falls in seniors. This fear can also increase anxiety and the isolation can lead to depression from loneliness.
RELATED — Depression Signs and Symptoms: Stop the downward spiral in time (Part 1)
After a fall, patients in hospital are often left in bed and not adequately rehabilitated, as staff might prefer to reduce liability risk.[10]
In these cases, the patient grows so weak that it can take months of rehab to get strength and mobility back.
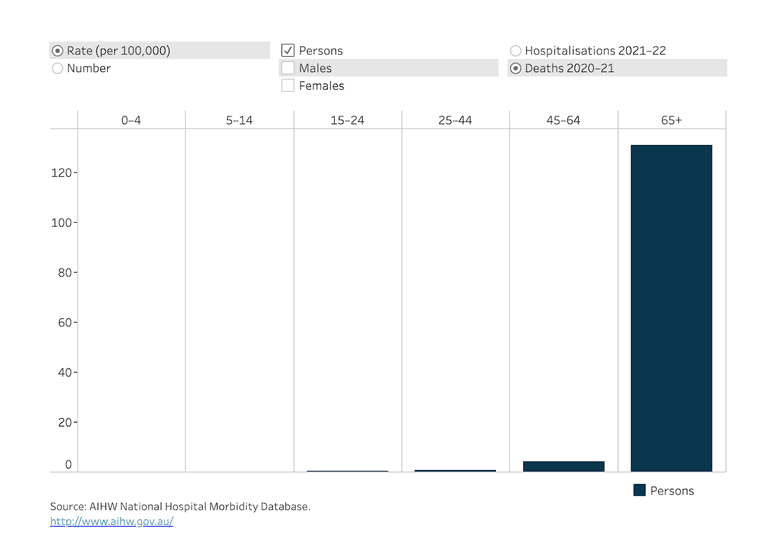
Falling and increased mortality
Falls account for a significant percentage of deaths in people over 65.[11]
There may not always be an immediate death after a fall. Like in the case of my grandmother, who fell and broke her neck, she was alert, responsive, able to talk and communicate for a few days in hospital. But she passed away several days later.
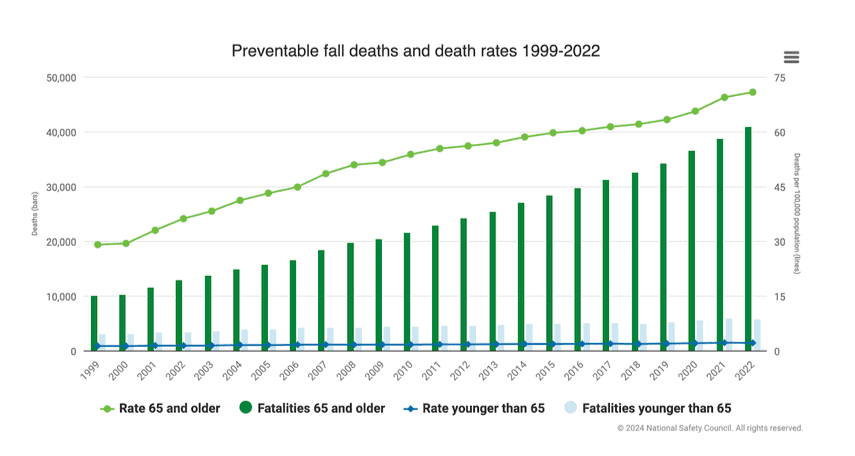
Source: NSC - Injury Facts.
So a fall can either cause immediate mortality, or delayed death, particularly if there has been a trauma to the brain or other vital parts of the body.
There could also be complications that arise from the fall such as infections, complications in surgery, blood clots or the fall could exacerbate an existing condition causing a decline in health and death.
It’s clear that preventative measures to reduce falls will reduce mortality from falls. Let’s take a look at these now.
Strategies to Prevent Falls
Around the world, we’ll find programmes that offer support and strategies to prevent or reduce falls in seniors.
These programmes and strategies that aim to prevent and reduce the risk of falling can mean the difference between a fatal and non-fatal fall. It’s literally the difference between life and death.
Some of these strategies deal with
- external environment
- reducing tripping hazards
- fall prevention strategies
And then there are lifestyle and health preventative measures. It is helpful to speak to your doctor and support network to find a strategy that works for your situation and condition.
Here are some strategies and interventions to reduce risk factors and lower the chances of falling.
Regular exercise – to keep your body strong, mobile and healthy.
Vision – make sure that glasses are suitable for long and short distances in order to walk outside. Also, get cataracts checked.
Medication – some medication can affect gait and stability. Check these with your doctor.
Suitable shoes – Wear suitable, secure non-slip shoes. Avoid loose shoes or walking around in socks.
Declutter – make sure there are clear, uncluttered pathways around your home, inside and outside.
Grab bars – install grab bars in bathrooms, stairs and other places in the home where falling might be a risk.
Smart storage – store items used often in places easy to access.
Wear a fall detection pendant – these devices can automatically raise an alarm to a customer care centre.
Vitamin D – has been shown to support bone health.
RELATED — Vitamin D: The sunshine hormone for stronger bones
Types of exercise
What type of exercise that is chosen should be suitable to the fitness level and health and mobility of the person. The activity can be anywhere from moderate to more vigorous intensity.
Some activities include:
- Walking
- Weight training
- Cycling
- Dancing
- Water-based exercises
- Tai chi
- Pilates
- Yoga
- Stair climbing
- House work
- Gardening
It’s important to know what type of exercise and what intensity is suitable for your body. It’s never too late to start being active!
Related Questions
1. What is the life expectancy after a fall in the elderly?
Life expectancy after a fall, especially with hip fractures, can decrease significantly. 20-30% of elderly patients die within a year due to related complications.
2. Do senior men or women fall more frequently?
Women more commonly fall due to osteoporosis, raising their risk of fractures.
Men, though falling less, suffer graver outcomes from falls due to lower participation in fall-prevention practices.
3. How can seniors improve their balance to prevent falls?
Seniors can enhance balance with regular exercises focusing on strength, mobility, and flexibility.
Activities like Tai Chi, yoga, walking, and balance-specific exercises improve stability and health. Getting eyes and glasses checked regularly, will also help proprioception and visibility for balance.
4. Are there any particular times of day when falls are more likely to occur in the elderly?
Falls are likelier at night or early morning due to low visibility and potential disorientation upon waking.
Improving lighting, decluttering paths, securing rugs, and keeping essentials close can reduce risks.
5. What are the psychological impacts of falling on seniors?
Falls have a negative psychological impact, causing fear, reduced activity, social withdrawal, and depression.
Addressing these through counselling and supportive re-engagement in activities is vital for wellbeing.
6. Can nutritional improvements help reduce the risk of falls in the elderly?
A balanced diet rich in calcium, vitamin D, and protein supports muscle strength and bone density, reducing fall injuries.
RELATED — Calcium (for healthy bones, teeth and heart)
Drinking lots of water is important. Limiting alcohol intake to prevent disorientation will also reduce the risk of falling.
Rahle Dusheiko is a Wellbeing Guide, certified Iyengar Yoga Teacher, and qualified Life Coach who blends yoga, life coaching, and holistic wellbeing to support balanced living.
With a yoga practice that began in 1999 and certification in 2014, Rahle’s approach extends beyond the mat, offering personalised pathways to health and vitality.
If you would like to learn more about Rahle , see Expert: Rahle Dusheiko.
References
(1) Tunstall Healthcare – 8 Kep Slip and Falls Statistics in Australia and New Zealand. September 2021. Retrieved from https://www.tunstallhealthcare.com.au/blog/8-key-slip-and-fall-statistics-in-australia-and-new-zealand?rq=falls
(2) Australia and New Zealand Falls Prevention Society | Info about falls. Retrieved from https://www.anzfallsprevention.org/info/#:~:text=Falls%20are%20a%20major%20health,least%20one%20fall%20per%20year
(3) Xing L, Bao Y, Wang B, Shi M, Wei Y, Huang X, Dai Y, Shi H, Gai X, Luo Q, Yin Y, Qin D. Falls caused by balance disorders in the elderly with multiple systems involved: Pathogenic mechanisms and treatment strategies. Front Neurol. 2023 Feb 23;14:1128092. doi: 10.3389/fneur.2023.1128092. PMID: 36908603; PMCID: PMC9996061. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9996061/#:~:text=Approximately%2028%20to%2035%25%20of,increases%20with%20age%20(11)
(4) National Council on Aging: Get the Facts on Falls Prevention. June 2024. Retrieved from www.ncoa.org/article/get-the-facts-on-falls-prevention
(5) Australian Institute of Health and Welfare: Injury in Australia: Falls. July 2023. Retrieved from https://www.aihw.gov.au/reports/injury/falls
(6) Cumming, R., Kelsey, J, Nevitt, M., Methodologic issues in the study of frequent and recurrent health problems in the elderly, Annals of Epidemiology, Volume 1, Issue 1. ScienceDirect: Methodologic issues in the study of frequent and recurrent health problems falls in the elderly. October 1990. Retrieved from https://www.sciencedirect.com/science/article/pii/104727979090018N
(7) WHO – Details on Falls. April 2021. Retrieved from https://www.who.int/news-room/fact-sheets/detail/falls
(8) WHO Global report on falls Prevention in older Age. 2007. Retrieved from https://iris.who.int/bitstream/handle/10665/43811/9789241563536_eng.pdf?sequence=1
(9) CDC: Facts About Falls – Older Adult Fall Prevention. May 2024. Retrieved from https://www.cdc.gov/falls/data-research/facts-stats/
(10) KFF Health News: ‘Fear Of Falling’ – How Hospitals Do Even More Harm By Keeping Patients In Bed. October 2019. Retrieved from https://kffhealthnews.org/news/fear-of-falling-how-hospitals-do-even-more-harm-by-keeping-patients-in-bed/
(11) CDC: Older Adult Falls Data. May 2024. Retrieved from https://www.cdc.gov/falls/data-research/






