
Melanie Young
B.A, B.App.Sc (Clin.Sc.), B Osteo.Sc., Reg. Osteopath, MONZ
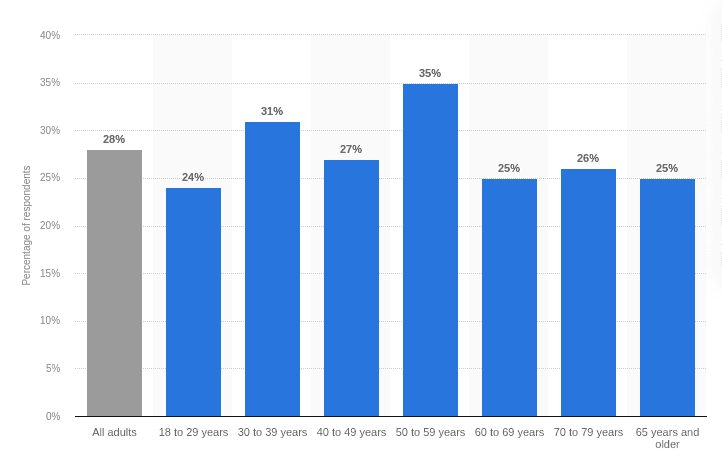
As some of us already know, pain associated with sciatica is extremely unpleasant and difficult to deal with. While many think that sciatica is associated with the older population, individuals who often exercise and are very active can also find themselves suffering with the same condition.
That is why once you experience sciatica for the first time, you will want to know as much as possible to prevent its recurrence, which is one of the goals of this two-part article.
Important note – seek medical attention immediately if you have problems controlling your bladder or bowels, or if you have numbness in your genital or anal area.
What is sciatica?
Sciatica describes pain that can occur anywhere along the path of the sciatic nerve, which runs from the lower back through the hips, buttocks, and down each leg to the foot.
It typically occurs when the nerve is compressed. This is often due to a
- herniated disc
- bone spur
- spinal stenosis
- muscular fascial tension
This compression can cause pain, numbness, tingling, or weakness in one leg. Sciatica is a symptom of an underlying issue rather than a condition itself.
Effective treatment often includes addressing the underlying cause through hands-on therapy, exercises, or other interventions aimed at relieving pressure on the nerve and improving overall spinal health.[1]
What are the signs and symptoms of sciatica?
As the longest and thickest nerve in your body, irritation or compression of the sciatic nerve can provide a range of signs and symptoms.
The most common symptoms include pain in the following areas:
- buttock
- posterior thigh
- outside of the leg below the knee
which may be stabbing or shooting right down to the foot.
The leg pain is usually worse than the back pain and there may also be a feeling of numbness and/or pins and needles in the skin. The leg pain may be made worse with coughing or sneezing.
Recognising these symptoms is vital for identifying the underlying cause and implementing appropriate treatment strategies.
Difficulty moving the leg
Sciatica may cause difficulty in lifting or moving the leg due to nerve compression in the lower back on one side, disrupting communication between the brain and muscles. There may be challenges with walking or climbing stairs.
This impaired mobility stems from weakened nerve signalling, contributing to muscle stiffness and discomfort.[2]
Sciatica may cause difficulty in walking
Muscular weakness in the leg
The hamstring muscles at the back of the thigh may become weakened and tight, the foot and calf muscles may also become weak, resulting in wasting (which means the muscle gets smaller and weaker) and difficulty walking.
The leg may feel ‘heavy’. The weakness may be due to pain or fear of pain in movement rather than objective weakness on testing.[3]
Pain in the glutes
Gluteal or buttock pain is a common symptom of sciatic nerve irritation, frequently associated with nerve inflammation and irritation. It is often caused by local muscle tightness or sitting on a wallet in your back pocket.
The sciatic nerve runs through or under the piriformis muscle in the glutes so excessive tension in this muscle or other deep gluteal muscles such as the gemelli, can compress the nerve and cause pain.[4]
Tingling, numbness and/or burning in the calf or foot
Sensations of tingling, numbness or burning in the foot indicate sciatic nerve involvement. Dermatomes represent the spinal nerve roots on the skin surface and the ones which are likely to be affected are the sole of the foot, the lateral foot and lateral calf.[5]
Pain in the back and/or leg when coughing or sneezing
A sudden pain in the leg or back when you cough or sneeze is a sign that you may have nerve compression caused by a disc bulge in the lower lumbar spine.
As you cough or sneeze, this increases the pressure in the cerebrospinal fluid and a weakened disc may push more disc material onto the nerve.
It is important to see a health professional who can assess you for disc injury so you can start doing the right things.[6]
What causes sciatica?
Sciatica is caused by compression or irritation of the sciatic nerve, often due to a herniated disc, spinal stenosis, or deep gluteal syndrome.
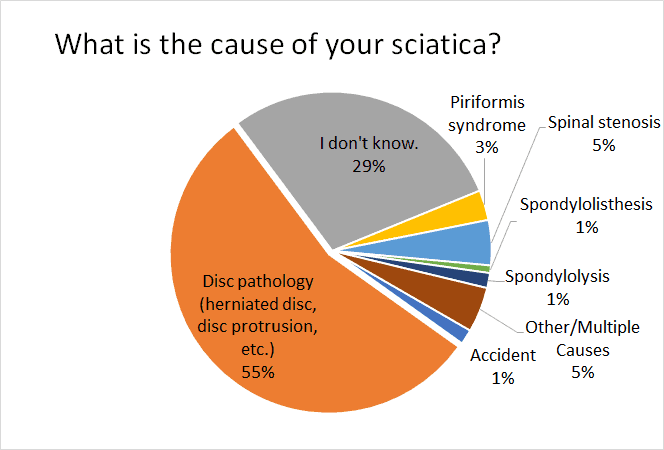
Source: Physiotherapy in Dwarka (https://physiotherapyindwarka.in/physiotherapy-for-sciatica/)
This pressure can result from
- accidental injury
- too much sitting
- lack of exercise
- repetitive strain lifting
or conditions such as vertebral fracture or spondylolisthesis, leading to inflammation and pain radiating along the nerve’s pathway.
Sciatica is caused by compression or irritation of the sciatic nerve
Herniated or prolapsed disc
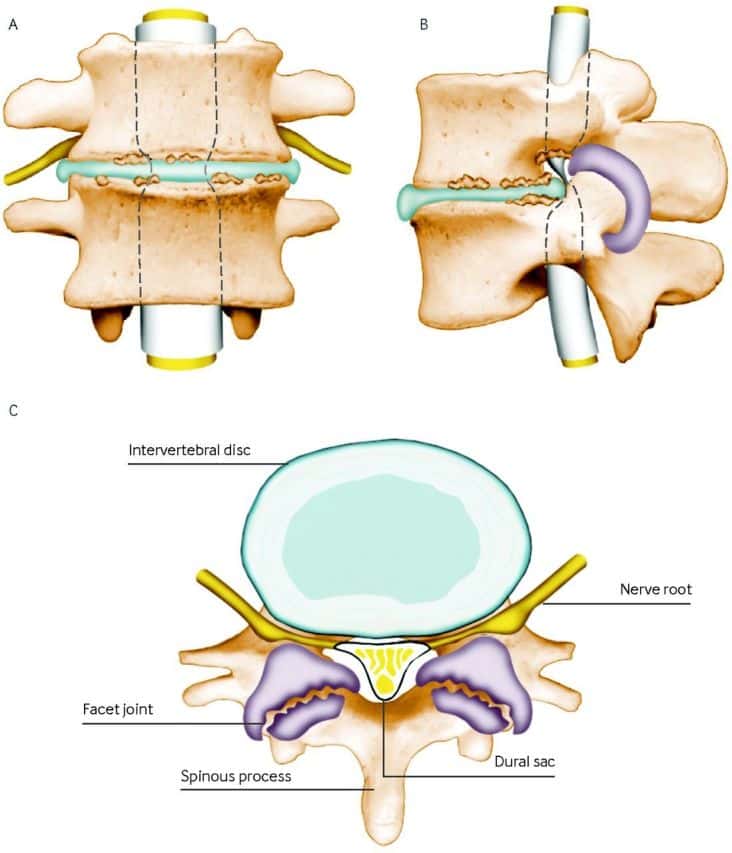
In the lower back, the L4/L5 disc or the L5/S1 vertebral disc are most vulnerable to damage.
The protective layers of the disc can become damaged and the nucleus pulposus material, which has the consistency of toothpaste, can push backward and laterally, causing pressure on the nerves that go down one leg and resulting in the nerve irritation we call sciatica.
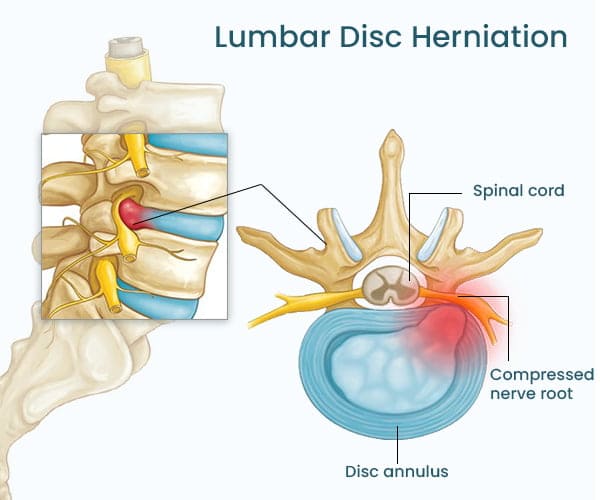
Osteopath/physio/chiro/orthopaedic specialists are trained in orthopaedic testing to assess these nerves. An MRI combined with clinical symptoms can often confirm if a herniated or prolapsed disc is causing the sciatic nerve pain.
Lumbar disc surgery does not always provide relief so it needs to be the last resort after all conservative options have been exhausted.[7,8]
Piriformis syndrome
Gluteal or buttock pain is a common symptom of sciatic nerve irritation, frequently associated with nerve inflammation and irritation.
It is often caused by local muscle tightness or sitting on a wallet in your back pocket. The sciatic nerve runs through or under the piriformis muscle in the glutes so excessive tension in this muscle or other deep gluteal muscles such as the gemelli, can compress the nerve and cause pain.[4]
Pregnancy
Sciatica in pregnancy is thought to occur in around 17-22% of pregnancies and usually not until the third trimester. It is more common in pregnant women with a large uterus and less body height to carry the growing foetus.
Sciatica occurs in around 17-22% pregnancies
Sciatica in pregnancy is contributed to by the normal increases in weight, the stretching of the abdominal muscles, common forward tilt of the pelvis and loosening of ligaments due to hormonal changes during pregnancy.[9]
Spinal stenosis
Spinal stenosis can cause symptoms similar to the leg pain of sciatica but it may occur on both sides at the same time. This is caused by compression of the nerves in the spinal canal.
Symptoms can include back pain, burning pain in the buttocks and down the legs, loss of feeling in the feet, and a numbness, cramping, or weakness in the legs.
Other symptoms include problems with balance and weakness of the muscles of the lower extremities.
Symptoms are posture dependent, appearing with standing and lumbar extension, exacerbated by walking, and relieved by sitting or forward flexion. Diagnosis is confirmed with MRI scanning.[10]
Spondylolisthesis
Spondylolisthesis occurs when a vertebra slips, usually forward, on the vertebra below, causing narrowing of the spaces for the spinal cord and spinal nerves as they exit the spine.
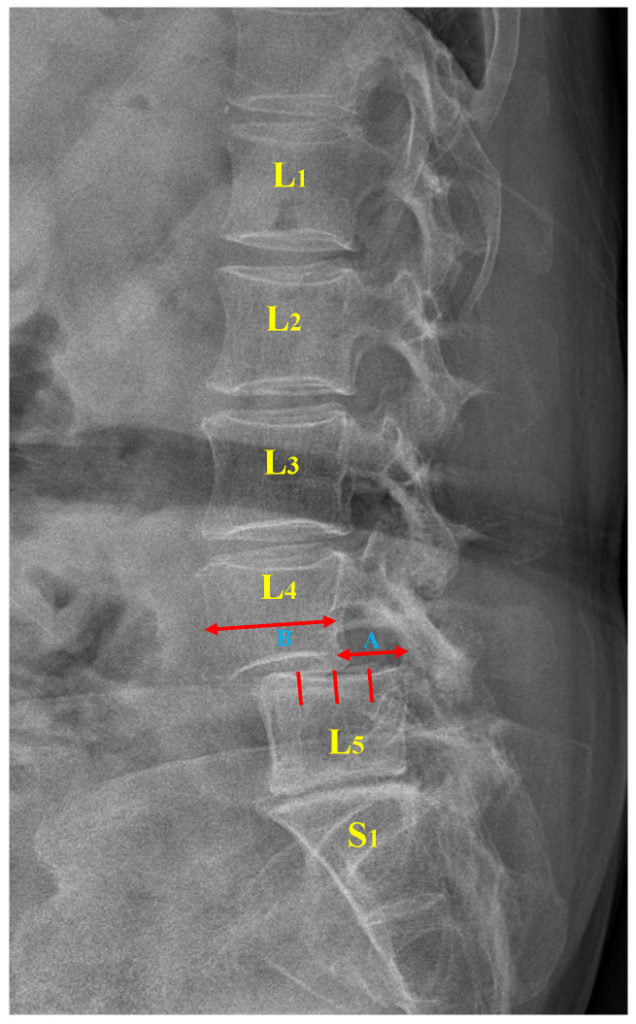
This condition can cause sciatica depending on the severity. An osteopath can assess your back to see if you have a ‘step defect’ and refer you for an X-ray of your spine to confirm the diagnosis.[11]
Trauma or injury to the lower back
Trauma to the back, such as a fall, heavy lifting, or sudden impact, can irritate or compress the sciatic nerve.
This may occur due to inflammation, a herniated disc, vertebral fracture or misalignment of the spine, which puts pressure on the nerve roots that form the sciatic nerve.
This irritation can lead to pain, tingling, or numbness radiating down the leg, known as sciatica.
Prompt evaluation and gentle hands-on treatment can help manage symptoms and prevent further complications.
Related Questions
1. Why does sciatica get worse at night?
This can happen due to several reasons.
Sleeping Position
Certain positions may put additional pressure on the sciatic nerve, exacerbating pain. For example, sleeping on your stomach or on a soft or uneven mattress can strain the lower back.
Reduced Movement
During the day, movement helps keep the muscles and joints more flexible. At night, lying still for long periods can cause the muscles around the nerve to tighten, leading to increased pain.
Inflammation
Inflammation in the spaces of the lower spine can increase overnight, as the body is in a more static state, potentially leading to an increase in nerve sensitivity.
Psychological Factors
At night, with fewer distractions, you may become more aware of the pain, which can make it feel more intense.
2. What are the best exercises to prevent sciatica?
If you are looking to prevent the recurrence of sciatica, then you should incorporate the following stretches and exercises into your daily or weekly routine:
- Cat-Cow Stretch
- Bird-Dog
- Hip Flexor Stretch
- Glute Bridges
- Hamstring Stretch
These stretches and exercises can help manage sciatic nerve pain by improving flexibility, reducing muscle tension and strengthening supporting muscles.
Melanie studied to become an osteopath at RMIT University in Melbourne, graduating with Distinction in 1997. She has over 45 years experience in dance, Tai Chi and Pilates. She draws on these foundations, combining them with gentle treatment approaches, including Functional, Cranial & Biodynamic Osteopathy, to effectively treat a wide range of ages and conditions.
If you would like to learn more about Melanie, see Expert: Melanie Young.
References
(1) Davis D, Maini K, Taqi M, et al. Sciatica. [Updated 2024 Jan 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/
(2) Stynes S, Konstantinou K, Ogollah R, Hay EM, Dunn KM (2018) Clinical diagnostic model for sciatica developed in primary care patients with low back-related leg pain. PLoS ONE 13(4): e0191852. https://doi.org/10.1371/journal.pone.0191852
(3) Dove L, Baskozos G, Kelly T, Buchanan E, Schmid AB. Prevalence of weakness and factors mediating discrepancy between reported and observed leg weakness in people with sciatica. Eur Spine J. 2024 Nov;33(11):4229-4234. doi: 10.1007/s00586-024-08330-6. Epub 2024 Jun 24. PMID: 38910169; PMCID: PMC7616658.
(4) Hopayian K, Heathcote J. Deep gluteal syndrome: an overlooked cause of sciatica. Br J Gen Pract. 2019 Sep 26;69(687):485-486. doi: 10.3399/bjgp19X705653. PMID: 31558515; PMCID: PMC6774708. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6774708/
(5) Fairag M, Kurdi R, Alkathiry A, Alghamdi N, Alshehri R, Alturkistany FO, Almutairi A, Mansory M, Alhamed M, Alzahrani A, Alhazmi A. Risk Factors, Prevention, and Primary and Secondary Management of Sciatica: An Updated Overview. Cureus. 2022 Nov 12;14(11):e31405. doi: 10.7759/cureus.31405. PMID: 36514653; PMCID: PMC9743914. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9743914/
(6) Verwoerd AJH, Mens J, El Barzouhi A, Peul WC, Koes BW, Verhagen AP. A diagnostic study in patients with sciatica establishing the importance of localization of worsening of pain during coughing, sneezing and straining to assess nerve root compression on MRI. Eur Spine J. 2016 May;25(5):1389-1392. doi: 10.1007/s00586-016-4393-8. Epub 2016 Feb 2. PMID: 26842881.
(7) Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ. 2007 Jun 23;334(7607):1313-7. doi: 10.1136/bmj.39223.428495.BE. PMID: 17585160; PMCID: PMC1895638. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC1895638/
(8) Mulleman D, Mammou S, Griffoul I, Watier H, Goupille P. Pathophysiology of disk-related sciatica. I.–Evidence supporting a chemical component. Joint Bone Spine. 2006 Mar;73(2):151-8. doi: 10.1016/j.jbspin.2005.03.003. Epub 2005 Jun 22. PMID: 16046173.
(9) Katonis P, Kampouroglou A, Aggelopoulos A, Kakavelakis K, Lykoudis S, Makrigiannakis A, Alpantaki K. Pregnancy-related low back pain. Hippokratia. 2011 Jul;15(3):205-10. PMID: 22435016; PMCID: PMC3306025. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC1895638/
(10) Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. 2016 Jan 4;352:h6234. doi: 10.1136/bmj.h6234. PMID: 26727925; PMCID: PMC6887476. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6887476/
(11) Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye AD. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(3):36917. doi: 10.52965/001c.36917. PMID: 35910544; PMCID: PMC9329062. Available from:






