
Beatrice Blanch
(BSc Physiology, PGCertMedTech)
Two decades ago sleep was overrated. Research and long-term studies were still ongoing and most of us thought that 6 hours of sleep should be enough.
Today, the science of sleep is clear — chronic lack of sleep or sleep deprivation can lead to multiple health issues and diseases, and long-term can lead to premature death.
In this article, we will look at the importance of sleep and why sleep is necessary for our overall health.
What is sleep — necessity or inconvenience?

Before the 1950s, most people thought that sleep was a passive activity, and that the body and the brain were inactive during sleep.
However, we now know that the brain is actually very active during sleep.
This means that it is engaged in many activities that are necessary to our waking life and health.[1]
Sleep makes up about one-quarter to one-third of a human’s life, so it only makes sense that important processes must happen during sleep as well.
Human beings are the only species that deliberately deprive themselves of sleep for no apparent gain.
— Matthew Walker, Why We Sleep
Walker also said that “Many people walk through their lives in an underslept state, not realising it”.[2]
Unfortunately, many people suffer from a lack of sufficient sleep, either from sleep deprivation or various sleep disorders, which is associated with many health problems, as well as a lower quality of life.
Why do we sleep?
Many of us have experienced the side effects of lack of sleep, such as
- poor memory and focus
- weakened immunity
- mood changes
Good sleep keeps us healthy and functioning well. It allows our body and brain to repair, restore, and be re-energised.
In the following sections, we will look into more detail as to why we sleep.
Sleep and endocrine health
Sleep deprivation is related to an increase in cortisol and results in glucocorticoid overload, which can lead to large negative effects on the body.
This can result in inflammation, weakened immune system, higher risk of diabetes and weight gain.
In short bursts, cortisol can help suppress inflammation. However, consistently high levels of cortisol can lead to inflammation and a weakened immune system.
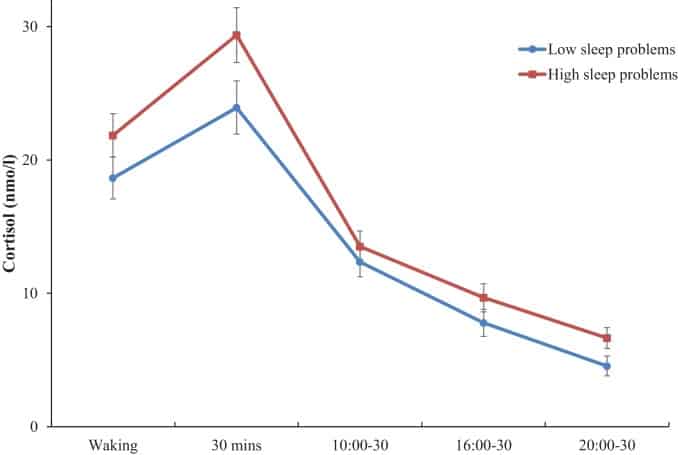
Cortisol helps to regulate blood sugar by releasing stored glucose, however having consistently high levels of cortisol can lead to high blood sugar (hyperglycaemia) and could cause type 2 diabetes.
RELATED — Diabetes: Early Signs, Causes, Types and Treatment
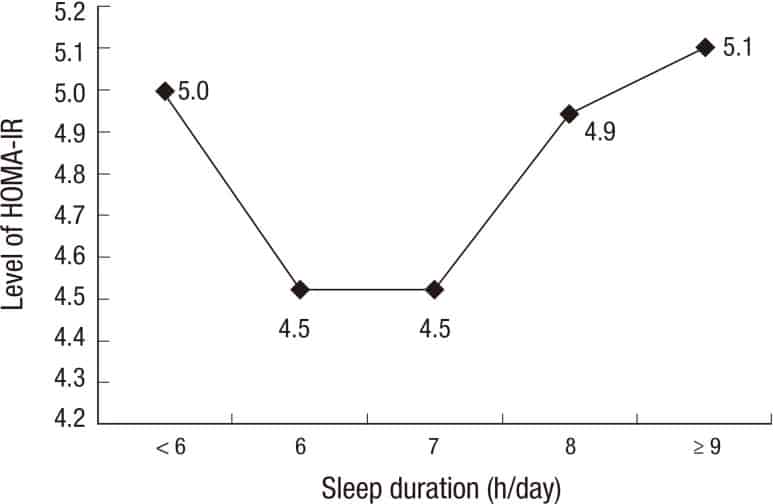
It is therefore no surprise that there is an association between short sleep duration and higher risk of developing obesity and type 2 diabetes.[3]
Sleep affects insulin
Insulin is a hormone that plays an important role in transferring glucose from the blood to our tissues where it can be used as energy.
Resistance to insulin occurs when the body either has trouble producing insulin, or when insulin is unable to transfer glucose into the tissues, resulting in high blood sugar levels and diabetes.
A study looked at the effect of a single night of sleep deprivation on insulin resistance. The subject group had one night of normal sleep, followed by a night of only 4 hours of sleep.
They found that partial sleep deprivation for just one night induces insulin resistance in multiple metabolic pathways in healthy subjects.[4]
Hormones ghrelin and leptin, that promote and suppress our appetite, are also sensitive to quantity and quality of sleep.
Levels of ghrelin increase before a meal time, and decrease after. Ghrelin levels increase after acute sleep deprivation, therefore increasing appetite and promoting food intake.
Chronic sleep deprivation or sleeplessness can cause a decrease in leptin levels, therefore it is more difficult for us to feel full.[5]
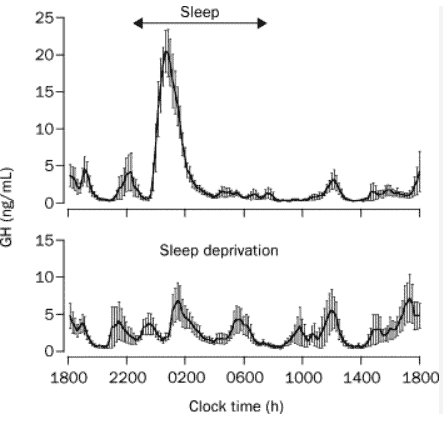
Source: Brandenberger, G. Effect of sleep deprivation on overall 24 h growth-hormone secretion. The Lancet. (2000)
Growth hormone is secreted by our pituitary gland, with increased secretion during sleep, particularly just after sleep onset.
The role of growth hormone includes
- regulating metabolism
- helping with the growth of bones, muscles, and other tissues
Growth hormone is released intermittently during sleep, with particular increases during stage N3 of sleep.
People with frequently disturbed sleep show lower night time levels of growth hormone plasma levels than healthy people.[6]
Sleep and cardiovascular health
Sleep is now recognised as an essential factor for the health of our heart.
It was only recently in 2022 that the American Heart Association (AHA) added sleep to its Healthy Heart Checklist, called ‘Life’s Essential 8,’ previously called ‘Life’s Simple 7’.
Healthy Heart Checklist lists behaviours or criteria to point us in the direction of optimal heart health, stating that “Sleep duration is associated with cardiovascular health”.
The other 7 important factors are
- diet
- physical activity
- nicotine exposure
- body mass index
- blood lipids
- blood glucose
- blood pressure
Measured by average hours of sleep per night, the ideal level is
Sufficient sleep can prevent high blood pressure
During normal sleep, blood pressure decreases relative to when we are awake. This is called nocturnal dipping.
If we are getting low quality sleep, for example suffering with obstructive sleep apnea or having frequent arousals during the night, blood pressure will stay higher for a longer period of time.
RELATED — Sleep apnea: How to cure it and get your sleep back
Because of this, the lack of nocturnal dipping is a strong predictor of hypertension, and cardiovascular risk. Poorly controlled hypertension remains a strong cause of cardiovascular-related morbidity and mortality worldwide.[9]
Lack of sleep can affect cholesterol levels
Cholesterol is made by our cells and is also a part of our diet. It serves as a precursor for the synthesis of important substances in the body including steroid hormones, bile acids, and vitamin D.
RELATED — Vitamin D: The sunshine hormone for stronger bones
The New Zealand guidelines for healthy cholesterol are listed in the table below.[10]
|
LDL: Less than 2.0 mmol/L |
|
LDL is also called bad cholesterol since if there is too much of it in our blood it can build up on the inside of our blood vessels. This makes our blood vessels more narrow and puts us at risk of heart disease or stroke. |
|
HDL: Greater than 1.0 mmol/L |
|
HDL is also called good cholesterol since it helps to clear out extra cholesterol, and prepares it to be removed from our body. Higher levels of HDL can lower our risk of heart disease or stroke. |
|
Triglycerides: Less than 1.7 mmol/L |
|
Energy from food that does not get used right away gets stored as triglycerides. Triglycerides can also build up inside blood vessels and increase cardiovascular risk. |
|
Total cholesterol: Less than 4.0 mmol/L |
| This is a rough measure of all the cholesterol and triglycerides in our blood. |
|
Total cholesterol/HDL ratio: Less than 4.0 |
|
This is the ratio of our total cholesterol to our HDL cholesterol. This ratio is used to estimate our risk of heart attack and stroke. |
A study was done which included 2,705 adults which found that people who had less sleep than average were more likely to have high levels of triglycerides and low HDL cholesterol.
Levels of HDL cholesterol were the highest when people slept 8 hours per night.[11]
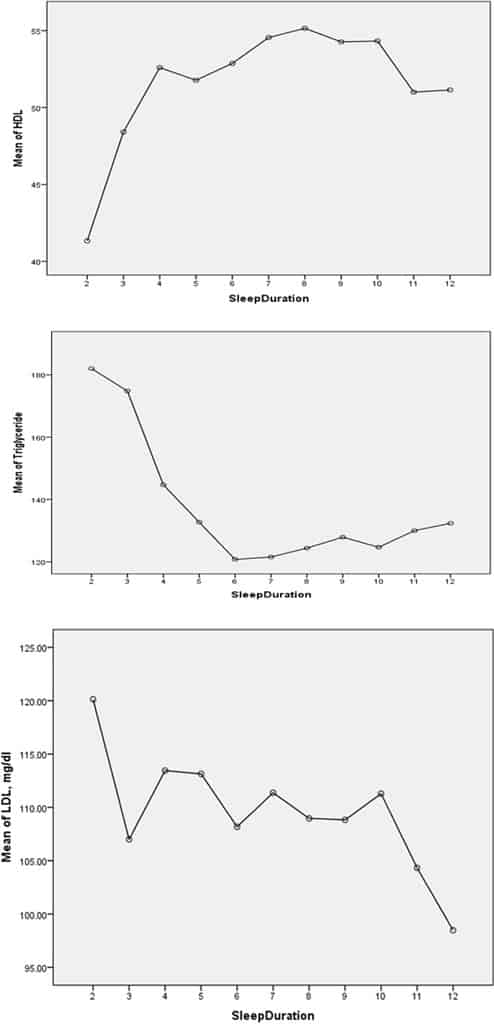
People with poor sleep quality or frequently interrupted sleep, such as in sleep apnea, often have
- high total cholesterol
- high LDL cholesterol
- high triglycerides in their blood
- low HDL cholesterol.[11]
Sleep and restoration, growth and repair
Sleep allows our bodies to repair and be rejuvenated, and restore what was lost while we were awake.
Sleep is able to facilitate major restorative functions in the body, for example muscle growth, tissue repair, and protein synthesis.
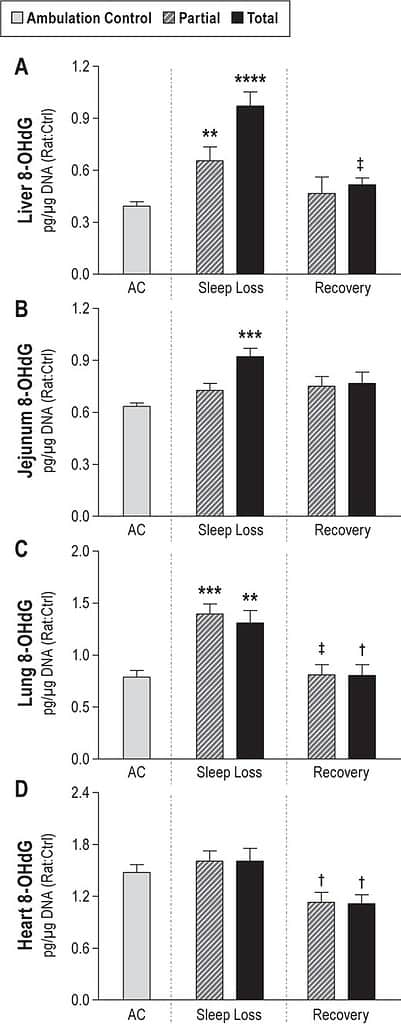
A study conducted in rats questioned the role of sleep in cell injury and repair. Rats underwent partial and total sleep deprivation over 10 days, then were allowed to sleep undisturbed for 2 days.
In totally sleep-deprived rats, the study found that oxidative DNA damage was 139% of control values, with organ-specific effects in the liver, lung, and small intestine.
In partially sleep deprived rats, there was also organ-specific DNA damage, with a 5.3-fold increase in dying cells in the intestinal epithelium compared to controls.
After two days of recovery sleep, damage was repaired to normal or almost normal values.[12]
Another indication of sleep for repair is the brain’s removal of adenosine. While we are awake, neurons in the brain produce adenosine as a result of cellular activities.[13]
Sleep and brain plasticity, memory and learning
Neuroplasticity is the ability of the brain to rewire itself and grow to create new connections between neurons.
Neuroplasticity allows the brain to learn new skills, change, and adapt to its environment.[14]
Synapses are connections between neurons that, along with neurotransmitters, allow electrical signals to travel from one neuron to another.
During the day, synapses are “excited” and their activity is increased in response to the stimuli that the brain receives from the environment. While asleep, the activity of these synapses goes back to normal.
Without this restorative period, the prolonged period of excitation inhibits neuroplasticity, which means that it is more difficult to learn new things while awake.[15]
A study was published in 2017 that looked at the effect of disturbed sleep on neuroplasticity. Men and women were asked to perform motor movement tasks during the day following a night of restful sleep, and a night of disturbed sleep.
The night of disturbed sleep was done by the researchers manipulating their sleep and decreasing the brain slow wave activity. Participants were unaware of which night was normal and disturbed.[16]
They found that after a night of good sleep, the participants were able to learn efficiently. However, after a night of manipulated sleep, learning efficiency did not improve and instead learning performance was as low as the evening on the previous day.[16]
Going without sleep for long periods of time can cause a range of psychopathological symptoms.
Lack of sleep can cause hallucinations
The researchers found that psychotic symptoms rapidly develop after one night without sleep, and develop further with increasing time awake.
These symptoms include
- visual/somatosensory misperceptions (illusions, visual distortions)
- hallucinations and delusions
- acute psychosis
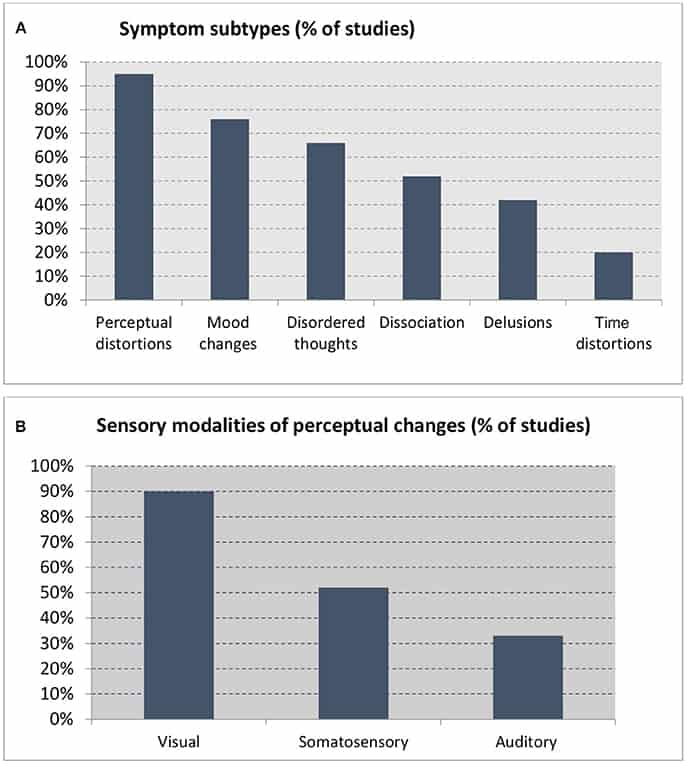
These experiences disappeared after a period of normal sleep in most cases.
Sleep and energy conservation
The energy conservation theory suggests that one of the main functions of sleep is to reduce demand for energy.
This is based on evolutionary theory as night would be the least efficient time to hunt or search for food, and the best time to be inactive due to less chance of dying from injury and the darkness acting as some protection from predation, therefore creating an evolutionary and reproductive benefit.[13]
However this has been contested due to REM sleep being a state of increased brain energy metabolism, therefore contradicting the theory.[17]
RELATED — Different types of sleep: Which one do we need the most?
In addition, after sleeping for 8 hours the calculated energy savings are only 5-9% per 24 hours.
This modest energy saving is not enough to explain the need for sleep in terms of energy conservation, especially in the context of evolutionary theory as sleeping also includes predation risks due to decreased behavioural responsiveness.[18]
Although energy conservation may be a contributing factor as to why we sleep, it can be argued that energy conservation should not be considered as one of sleep’s primary functions.[17]
Related Questions
1. How can I increase my sleeping hormones?
Melatonin is referred to as the sleep hormone.
It is produced by the body just after it gets dark and reaches its peak in the early hours of the morning, reducing during daylight hours.
Increasing darkness around bedtime, for example dimming lights and staying off of screens, may help to increase melatonin.
You may also ask your doctor for supplementary melatonin in the form of a tablet. See the Health Navigator NZ for rules and regulations about getting melatonin prescribed.
2. What is the difference between sleep onset and sleep latency?
Sleep onset is the exact time that we fall asleep or enter our first stage of sleep, usually stage N1.
Sleep latency is the time between “lights out” and sleep onset. In other words, the duration of time it takes for you to fall asleep.
3. How do I fix sleep latency?
If you find that it is taking you a very long time to fall asleep, try to become more aware of healthy sleep hygiene habits.
This includes
- being consistent with your bedtime and wake time everyday, including weekends
- making sure your bedroom is dark, relaxing, and quiet, and at a comfortable temperature
- removing electronic devices such as phones, laptops, TVs from the bedroom, or at least avoiding using them before you go to bed
- avoiding large meals, caffeine, alcohol exercise before bedtime.
If you are looking to unwind before sleep, we suggest checking our section on Relaxation.
Beatrice is currently completing her Postgraduate Diploma in Medical Technology, with an endorsement in Sleep Medicine, and has been fortunate to be working in healthcare in conjunction with her postgraduate studies.
Since starting, Beatrice has seen first-hand the effects of lifestyle on sleep hygiene, and the relationship between poor sleep and preventable chronic diseases. Beatrice aims to use scientific evidence-based research to help educate people on the importance of healthy sleep hygiene so that they may improve the quality of their life.
References
(1) John Hopkins Medicine. The Science of Sleep: Understanding What Happens When You Sleep. Retrieved from https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-science-of-sleep-understanding-what-happens-when-you-sleep
(2) Berkeley Psychology. Sleep Scientist Warns Against Walking Through Life ‘In An Underslept State’.
(3) Hirotsu, C., Tufik, S., & Andersen, M. L. (2015). Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep science 8(3), 143–152. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4688585/#:~:text=Sleep%20deprivation%20seems%20to%20be,deleterious%20effects%20on%20the%20body
(4) Donga, E., van Dijk, M., van Dijk, J. G., Biermasz, N. R., Lammers, G. J., van Kralingen, K. W., Corssmit, E. P., & Romijn, J. A. (2010). A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. The Journal of clinical endocrinology and metabolism, 95(6), 2963–2968. Retrieved from https://pubmed.ncbi.nlm.nih.gov/20371664/
(5) Thomas, L. (2019). Ghrelin and Sleep. News-Medical. Retrieved from https://www.news-medical.net/health/Ghrelin-and-Sleep.aspx#:~:text=Ghrelin%20levels%20rise%20primarily%20in,concentrations%20remain%20essentially%20the%20same
(6) Kim, T. W., Jeong, J. H., & Hong, S. C. (2015). The impact of sleep and circadian disturbance on hormones and metabolism. International journal of endocrinology 591729. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4377487/
(7) Makarem, N., Castro‐Diehl, C., St‐Onge, M-P., Redline, S., Shea, S., Lloyd‐Jones, D., Ning, H., & Aggarwal, B. (2022). Redefining Cardiovascular Health to Include Sleep: Prospective Associations With Cardiovascular Disease in the MESA Sleep Study. Journal of the American Heart Association. Retrieved from https://www.ahajournals.org/doi/10.1161/JAHA.122.025252
(8) Allen, N. B., Anderson, C. A. M., Black, T., Brewer L. C., Foraker, R. E., Grandner, M. A., Lavretsky, H., Perak, A. M., Sharma, G., Rosamond, W. (2022). American Heart Association adds sleep to cardiovascular health checklist. Retrieved from https://newsroom.heart.org/news/american-heart-association-adds-sleep-to-cardiovascular-health-checklist?utm_campaign=sciencenews21-22&utm_source=science-news&utm_medium=phd-link&utm_content=phd-06-29-22
(9) Calhoun, D. A., & Harding, S. M. (2010). Sleep and hypertension. Chest, 138(2), 434–443. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2913764/
(10) Health navigator NZ. What do my cholesterol results mean? Retrieved from https://www.healthnavigator.org.nz/health-a-z/c/cholesterol-test-results/
(11) Smiley, A., King, D., Harezlak, J., Dinh, P., & Bidulescu, A. (2019). The association between sleep duration and lipid profiles: the NHANES 2013-2014. Journal of diabetes and metabolic disorders, 18(2), 315–322. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6914752/
(12) Everson, C. A., Henchen, C. J., Szabo, A., & Hogg, N. (2014). Cell Injury and Repair Resulting from Sleep Loss and Sleep Recovery in Laboratory Rats. Sleep, 37(12), 1929–1940. Retrieved from https://www.google.com/url?q=https://academic.oup.com/sleep/article/37/12/1929/2416803&sa=D&source=docs&ust=1676082491507160&usg=AOvVaw134P0ZVNNVH_TSeRzNMnkf
(13) Healthy Sleep Harvard. Why Do We Sleep, Anyway? Retrieved from https://healthysleep.med.harvard.edu/healthy/matters/benefits-of-sleep/why-do-we-sleep
(14) Zhang, M. Q., Li, R., Wang, Y. Q., & Huang, Z. L. (2017). Neural Plasticity Is Involved in Physiological Sleep, Depressive Sleep Disturbances, and Antidepressant Treatments. Neural plasticity, 5870735. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5664320/
(15) Gorgoni, M., D’Atri, A., Lauri, G., Rossini, P. M., Ferlazzo, F., & De Gennaro, L. (2013). Is sleep essential for neural plasticity in humans, and how does it affect motor and cognitive recovery? Neural plasticity, 103949. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3693176/
(16) Fattinger, S., de Beukelaar, T., Ruddy, K. Volk, C., Heyse, N. C., Herbst, J. A., Hahnloser, R. H. R., Wenderoth, N., & Huber, R. (2017). Deep sleep maintains learning efficiency of the human brain. Nature Communications 8, 15405. Retrieved from https://www.nature.com/articles/ncomms15405#citeas
(17) Schmidt, M. H. (2014) The energy allocation function of sleep: A unifying theory of sleep, torpor, and continuous wakefulness. Neuroscience & Biobehavioral Reviews 47, 122-153. Retrieved from https://www.sciencedirect.com/science/article/pii/S0149763414001997
(18) Latifi. B., Adamantidis. A., Bassetti. C., Schmidt, M. H. (2018). Sleep-Wake Cycling and Energy Conservation: Role of Hypocretin and the Lateral Hypothalamus in Dynamic State-Dependent Resource Optimization. Frontiers in Neurology 9. Retrieved from https://www.frontiersin.org/articles/10.3389/fneur.2018.00790/full






