
Carly Hanna
BSc (Human Nutrition and Psychology)
Note — The article was checked and updated April 2024.
Food is one of life’s great pleasures and the act of eating brings people together and creates memories that last for a lifetime.
Individuals with Coeliac disease see such gatherings as stressful and as a real risk of becoming unwell due to food cross-contamination with gluten.
If not managed properly, Coeliac disease can have a profound impact on mental health as well as the physical health of the affected individual, which is why support and understanding more about this disease is important.
What is coeliac disease?
Coeliac disease is an autoimmune disorder where the immune system damages cells in the lining of the small intestine. It can develop during any stage of life and is mostly caused by genetic factors.[1,2]
While the disease is not reversible, eating a gluten-free diet is the best treatment to avoid a range of uncomfortable symptoms such as bloating and cramping, nausea, diarrhoea, and constipation.
How does coeliac disease affect digestion?
Given that coeliac disease damages the surface of the small intestine, this makes it very difficult for the gut to absorb any nutrients.
The finger-like projections known as villi help absorb nutrients from the food we eat. However, in coeliac disease, the villi are flattened due to inflammation. This makes proteins such as gluten hard to digest.
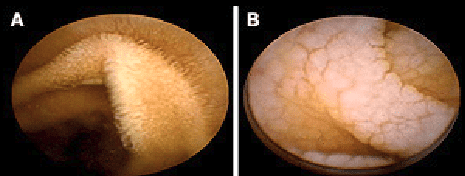
In coeliac disease individuals, the intestinal villi become damaged after continued inflammation and exposure to irritants such as gluten.[3,4]
Coeliac disease sufferers often have nutritional deficiencies
Gluten in food
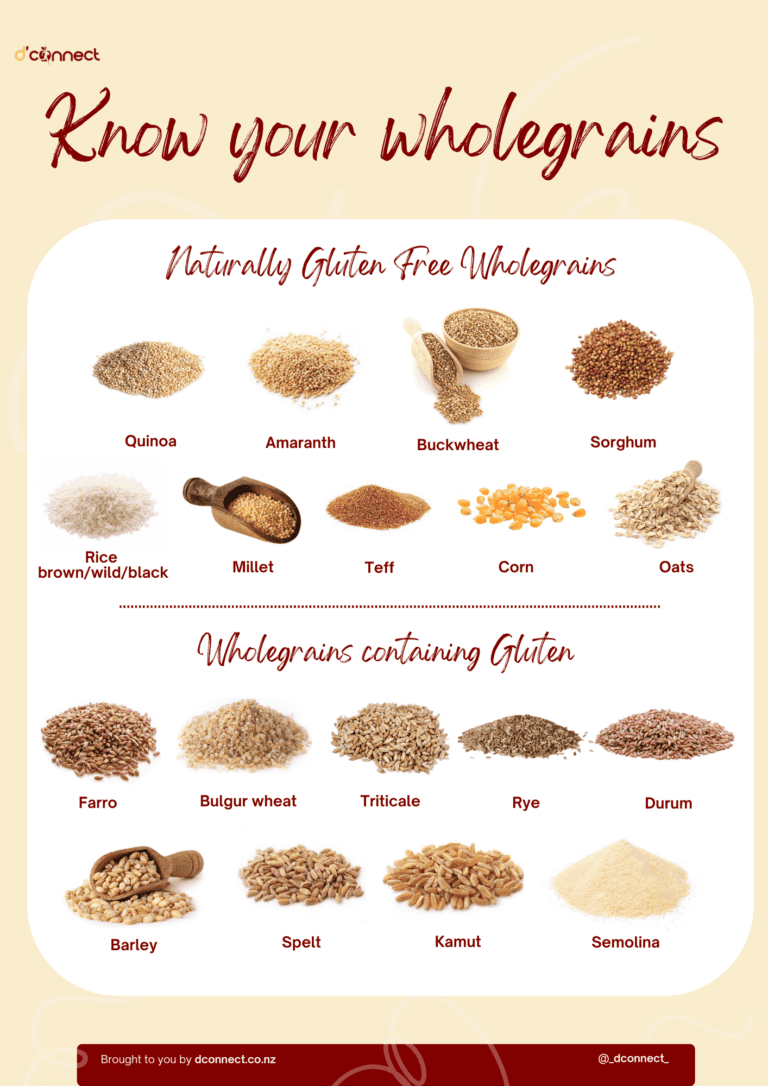
Gluten is a protein found in many grains such as barley, rye, oats and wheat – otherwise known as the acronym BROW.
In food products, wheat may also be called
- atta
- bulgur
- bran
- couscous
- dinkel
- durum
- emmer
- farina
- graham flour
- kamat
- polish wheat
- semolina
- spelt
- triticale
- wheat germ[5]
These grains are found in an abundance of food products, including breads, pastas, cereals and even in non-food products such as medicines and supplements.[6]
Avoiding these foods and products is not always enough because there is also the issue of cross-contamination, which we will discuss further in this article.[1]
With that said, let’s circle back and see when coeliac disease was first discovered.
History of coeliac disease
In the early 1800s, Matthew Baillie first described a disease that affected the gastrointestinal system presenting symptoms such as diarrhoea and malnutrition.[7,8]
However, it wasn’t until 1888 that Dr Samuel Gee first recognised and termed “coeliac”, which originated from the Greek term “suffering in the bowels”, and suggested that this could be improved through diet. Though at this point, it wasn’t certain which foods were causing gastrointestinal issues.
For the next few decades, several studies looked at diets high in starches, such as bananas and rice, to try and pinpoint what caused coeliac disease and which diets helped treat it.
While gluten had been used for centuries, it wasn’t until the early 1940s that Dr Willem Dicke theorised that it was in fact the wheat protein gluten that was causing the disorder.
In the 1950s, the significance of gluten and its role in coeliac disease was discovered, which is when the gluten-free diet was established.
In the 1970s, the gene HLA-DQ2 was associated with coeliac disease. In the 1980s, it was suspected that coeliac disease was an autoimmune disease, before finally being confirmed in the early 1990s.
Since then, there has been an increase in awareness around a gluten-free diet as well as an increase in the range of gluten-free products readily available.
However, has the prevalence of coeliac disease increased over the years or would we today just have more awareness around food allergies and diet culture that hypes up a gluten-free diet?
Prevalence of coeliac disease
Up to 100,000 people in NZ have coeliac disease, with nearly a third of those being children.[2] These statistics are also seen worldwide as it affects 1 in 100 people (about 1-2% of the population).[1]
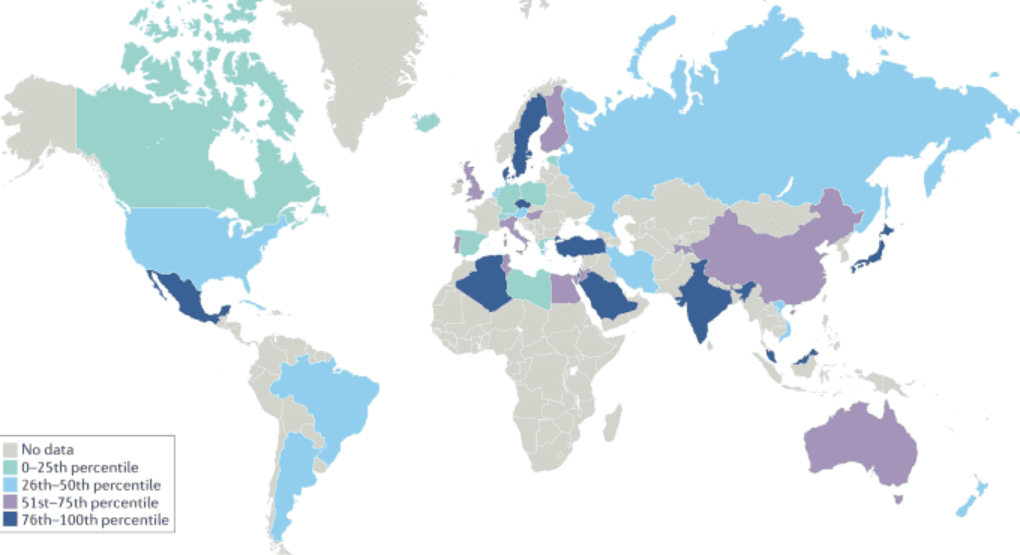
Because coeliac disease is an autoimmune disorder, it has a strong genetic tendency, which means that it is heritable and can run in families.[9]
Coeliac disease can develop at any stage of life
Reasons that may explain an increase in gluten intolerance include are
- Change in the production of crops and use of pesticides,
- Change from “soft” wheat (low gluten-containing wheat) to “hard” wheat (high gluten-containing wheat)
- The use of antibiotics, which causes resistance to protein digestion
- Westernised, low-nutrient diet which suppresses the immune system
- Changes in genetic and environmental factors[6,10]
There is no clear evidence to date that environmental factors, such as stress or antibiotics, can trigger the development of coeliac disease. However, it is still likely that coeliac is a result of a combination of both environmental and genetic factors.[1]
What are the symptoms of coeliac disease?
Coeliac disease can cause a wide range of symptoms including
- gastrointestinal
- dermatological
- neurological
and also other symptoms due to a lack of nutrients being absorbed in the body.
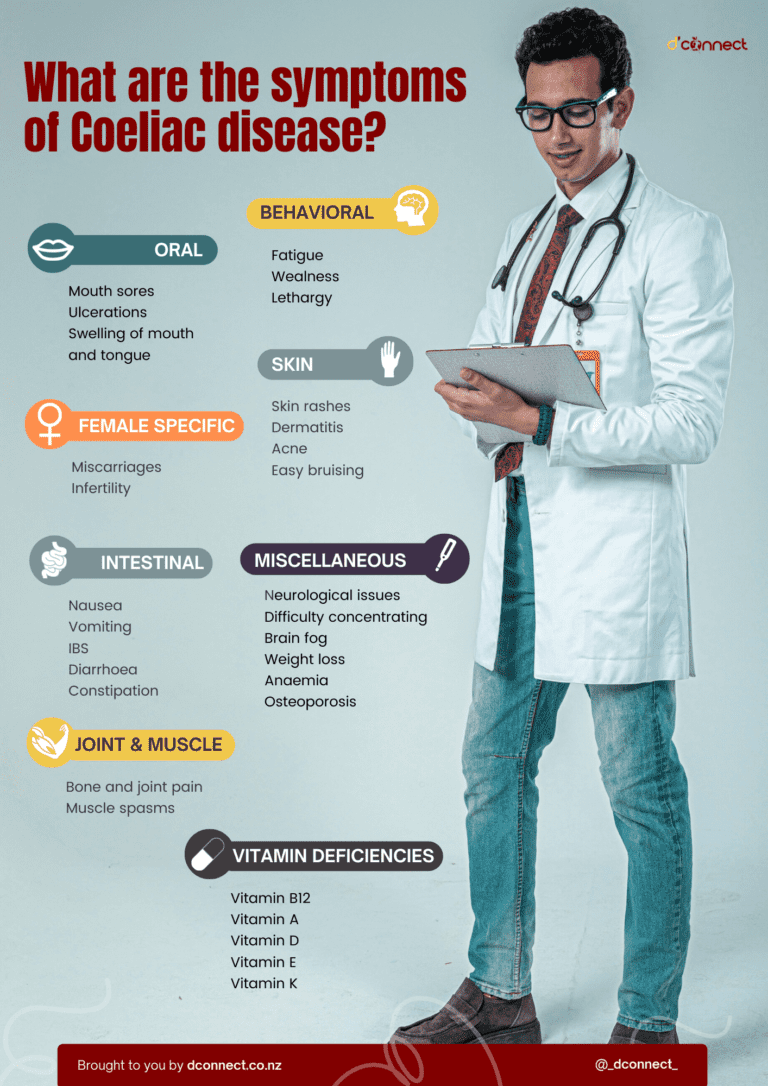
Irritable Bowel Syndrome (IBS) symptoms
Fatigue
Weight loss
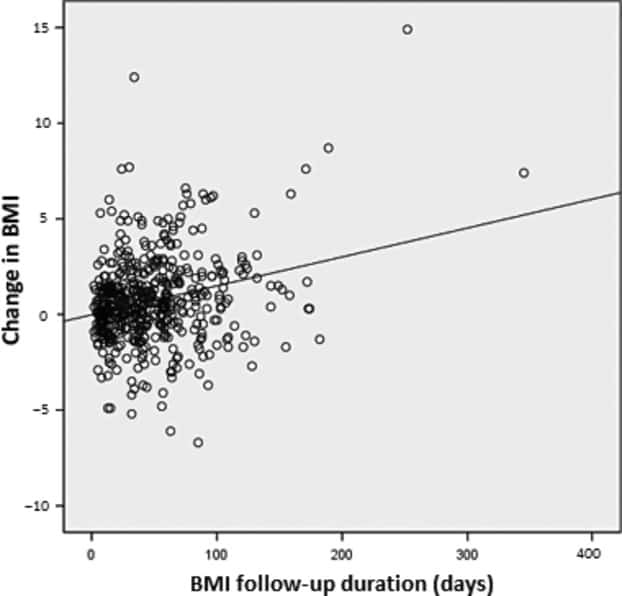
Because the digestive system isn’t absorbing food properly, it is likely that our body is deficient in the energy and nutrients it needs. Undiagnosed coeliac disease can lead to having a lower BMI than the general population.[12]
Abdominal bloating and cramping
Nausea and vomiting
Cramping, bloating and nausea are common symptoms of coeliac disease
Bruising of the skin
Muscle spasms
Muscle spasms can be a result of low blood calcium and magnesium levels, so the muscles contract involuntarily.[1,2]
RELATED — Magnesium (for a great night of sleep)
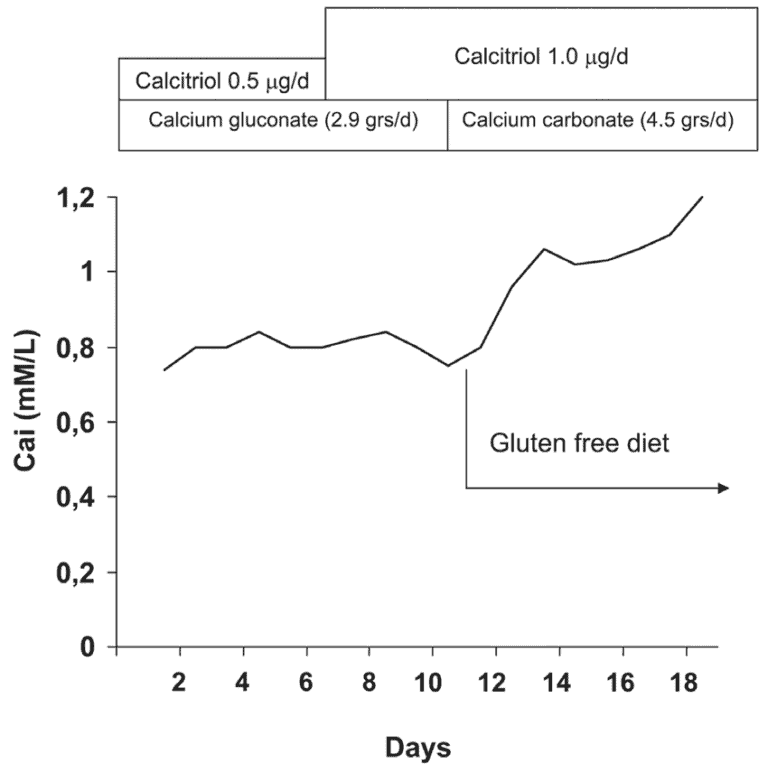
Source: Marcondes J. Resistance to Vitamin D Treatment as an Indication of Celiac Disease in a Patient with Primary Hypoparathyroidism. (2009)
Skin Conditions
Neurological issues
As food is also important for our brain, coeliac disease can also produce neurological symptoms and conditions, such as:
- Epilepsy (abnormal brain activity causing seizures)
- Ataxia (poor muscle control causing incoordination)
- Neuropathy (damage to the nervous system that can result in numbness and tingling)
- Myelopathy (damage to the spinal cord)[12]
This can be a result of not having the essential nutrients needed for the brain, neurotransmitters and nerves to work properly. Any of these conditions can produce symptoms such as
- Headaches
- Brain fog
- Difficulty concentrating
- Memory loss[13]
Bone and joint pain and increased risk of arthritis
Muscle weakness and bone and joint pain are less common symptoms of coeliac disease. Due to the inability to absorb essential nutrients for bone health, such as calcium and vitamin D, those with coeliac disease are four times more likely to develop early signs of arthritis.[1]
Related Questions
1. What is the difference between coeliac disease, gluten intolerance and wheat allergy?
Coeliac disease is an autoimmune disorder, whereas gluten intolerance and wheat allergy are not.
Those with coeliac disease are also likely to have more severe, persistent symptoms and an increased risk of other diseases compared to those with a gluten intolerance or wheat allergy.
2. At what age does coeliac disease usually occur or start?
Coeliac disease can develop at any age and is known to be diagnosed in childhood as well as adulthood. Early detection is key.
3. Is coeliac a serious disease?
Coeliac disease can have serious implications for one’s health as it can put those at risk of developing other diseases.
Those with coeliac disease have a slightly higher risk of mortality (shorter lifespan), however, following a gluten-free diet can help prevent this.[14]
4. Can coeliac disease affect pregnancy?
Coeliac disease can affect menstrual cycles, fertility, and also increase the risk of miscarriage.
5. What blood type is more common in having coeliac disease?
There is insufficient evidence around certain blood types being linked to autoimmune diseases, such as coeliac disease.[15]
6. Are men or women more prone to coeliac disease?
The prevalence and severity of coeliac disease are slightly higher in women than in men.[16]
If you are looking to minimise the consumption of gluten in your diet, we suggest checking our Recipe page where you will find easy-to-make and nutritious gluten-free meals.
Carly is currently an Intern Psychologist in the Whitiora Diabetes Service at Te Whatu Ora Counties Manukau. She has completed a Bachelor of Science, majoring in Human Nutrition and Psychology and is currently attaining her Masters in Health Psychology and Postgraduate Diploma in Health Psychology…
If you would like to learn more about Carly, see Expert: Carly Hanna.
References
(1) Health Navigator New Zealand. Coeliac Disease (21/06/22). Accessed 02/10/22. Retrieved from https://www.healthnavigator.org.nz/health-a-z/c/coeliac-disease/
(2) Coeliac New Zealand. How to Recognise Coeliac Disease (2022). Accessed 02/10/22. Retrieved from https://coeliac.org.nz/what-is-coeliac-disease/
(3) Clinical Education. Coeliac Disease 4 times more common than previously thought (2010). Accessed 02/10/22. Retrieved from https://www.clinicaleducation.org/news/coeliac-disease-4-times-more-common-than-previously-thought/
(4) Beyond Coeliac. Coeliac Disease: symptoms, testing, treatment and research (2022). Accessed 02/10/22. Retrieved from https://www.beyondceliac.org/celiac-disease/
(5) Health Navigator New Zealand. Gluten-free diet (11/07/22). Accessed 02/10/22. Retrieved from https://www.healthnavigator.org.nz/healthy-living/g/gluten-free-diet/
(6) Royal Lee Organics. Overview of what flour (2022). Accessed 02/10/22. Retrieved from https://www.organicsbylee.com/overview-of-wheat-flour/
(7) Beyond coeliac. History of coeliac disease (2022). Accessed 02/10/22. Retrieved from https://www.beyondceliac.org/celiac-disease/celiac-history/
(8) Parzanese I, Qehajaj D, Patrinicola F, Aralica M, Chiriva-Internati M, Stifter S, Elli L, Grizzi F. Celiac disease: From pathophysiology to treatment. World journal of gastrointestinal pathophysiology. 2017 May 15;8(2):27. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5437500/
(9) Makharia GK, Singh P, Catassi C, Sanders DS, Leffler D, Ali RA, Bai JC. The global burden of coeliac disease: opportunities and challenges. Nature Reviews Gastroenterology & Hepatology. 2022 May;19(5):313-27. https://doi.org/10.1038/s41575-021-00552-z
(10) Tucker, S. 5 Reasons Gluten Intolerance is on the Rise. Threebakers.com (10/09/15). Accessed 02/10/22. Retrieved from https://threebakers.com/5-reasons-gluten-intolerance-is-on-the-rise/
(11) News Medical. Iron deficiency in coeliac disease and obesity (28/09/22). Accessed 02/10/22.
(12) Kabbani TA, Goldberg A, Kelly CP, Pallav K, Tariq S, Peer A, Hansen J, Dennis M, Leffler DA. Body mass index and the risk of obesity in coeliac disease treated with the gluten‐free diet. Alimentary pharmacology & therapeutics. 2012 Mar;35(6):723-9. https://doi.org/10.1111/j.1365-2036.2012.05001.x
(13) Coeliac UK. Neurological symptoms. Accessed 23/10/22. Retrieved from https://www.coeliac.org.uk/information-and-support/coeliac-disease/conditions-linked-to-coeliac-disease/neurological-conditions/?&&type=rfst&set=true#cookie-widget
(14) Lebwohl B, Green PH, Söderling J, Roelstraete B, Ludvigsson JF. Association between celiac disease and mortality risk in a Swedish population. Jama. 2020 Apr 7;323(13):1277-85. DOI: 10.1001/jama.2020.1943
(15) Soliman, M. Are certain blood types more prone to autoimmune disease? Healthline (10/06/21). Accessed 23/10/22. Retrieved from: https://www.healthline.com/health/blood-type-and-autoimmune-diseases#alopecia-areata
(16) Ciacci C, Cirillo M, Sollazzo R, Savino G, Sabbatini F, Mazzacca G. Gender and clinical presentation in adult celiac disease. Scandinavian journal of gastroenterology. 1995 Jan 1;30(11):1077-81. DOI: 10.3109/00365529509101610






