
Carly Hanna
BSc (Human Nutrition and Psychology)
Coeliac disease affects 1.4% of the world population, however, it’s suggested that this might be higher since many individuals with gastrointestinal symptoms go undiagnosed.
To understand what testing is available, and what kind of diet and supplements can assist individuals with coeliac disease to avoid serious health issues, we’ll first need to look into conditions that have similar symptoms.
Difference between gluten intolerance, wheat allergy and coeliac disease
While these three conditions are commonly mistaken for one another, there are distinct tests that can distinguish between them.
RELATED — Coeliac Disease: Symptoms and Effects on our health and body
Symptoms of coeliac disease often mimic other gut diseases, such as irritable bowel syndrome (IBS) and Crohn’s disease.
Wheat Allergy | Gluten Intolerance (non-coeliac gluten sensitivity) | Coeliac Disease |
|
|
|
If you suspect that you may be intolerant or allergic to gluten, or have coeliac disease, the first step is seeing your GP. They can help assess your symptoms.
How to get tested for gluten intolerance, wheat allergy and coeliac disease
Coeliac disease can be hard to diagnose, which is why you should know more about the tests we shared below.
Wheat allergy testing
The main way to test for a wheat allergy is to get a skin prick test from your health professional. A skin prick procedure involves small pricks in the skin where a wheat-containing serum is then placed.
If the area becomes itchy, red and/or swollen, this indicates that there may be a wheat allergy – an immunological response to ingesting wheat proteins.[1]

However, if there is no history of clinical symptoms, a positive skin prick test is not enough to diagnose a wheat allergy.
Gluten intolerance (non-coeliac gluten sensitivity) testing
A gluten intolerance is when our body doesn’t have an immunological reaction to ingesting wheat, but we can still have gastrointestinal symptoms.
After a negative skin-prick procedure, the most common way to see if we are gluten intolerant is through trial and error. This may include eliminating all gluten-containing foods and monitoring our symptoms.
Once this has been done, we can slowly add back gluten-containing foods and if our symptoms return, this usually indicates gluten intolerance.
Coeliac disease testing
Serology test looks for antibodies, such as IgA and IgE, to see if there is an immune response to eating gluten.[2]
If there are high levels of antibodies, this indicates an immune response to gluten.[3]
For further confirmation of coeliac disease, an endoscopy and biopsy can be performed.
An endoscopy involves a camera, attached to an endoscope, being placed down the esophagus, all the way to the small intestine as it aims to look for signs of flattening villi.
A biopsy involves removing a sample of the tissue from the digestive system, and it may also be performed at the same time.
Treatment for coeliac disease
Treatment for coeliac disease often includes:
- gluten-free diet
- dairy-free diet
- use of supplements[4]
Other forms of treatment can include
- Intermittent fasting[5]
- Eating less frequent (this allows more times between meals to ensure gastric emptying)
RELATED — Intermittent Fasting: Diet with actual health benefits
Life-long gluten-free diet
Foods that are naturally gluten-free are wholefoods such as
- unprocessed meat
- dairy
- eggs
- rice
- fruits and vegetables
- beans and legumes
- nuts and seeds
- butters and oils
Strict gluten-free diet can bring personal and social challenges. However, with the growing number of gluten-free alternatives to breads, pastas and cereals, there are increasing options for those following a gluten-free diet.
A common nutrition myth enforced by the diet culture is that carbohydrates are “bad”.
For individuals with coeliac disease, cutting out carbohydrates isn’t necessarily needed. However, due to increased likelihood of nutrient deficiencies, it is recommended that supplements are used to obtain more vitamins and minerals.
Lactose-free or dairy-free diet
As most people with coeliac have second-hand lactose intolerance, following a lactose-free or dairy-free diet can help build up the enzyme lactase in the body.
Gluten-free and dairy-free diet helps treat coeliac disease
Not consuming dairy can often reduce the amount and/or severity of symptoms that people experience with coeliac disease.
Supplements that help with coeliac disease
Due to the increased risk of nutrient deficiencies with coeliac disease, supplements are often a good idea to increase our intake of vitamins and minerals.
Recommended nutrients and dosages include[6]
- vitamin B12 – 500 mcg/day
- zinc – 30mg/day
- RELATED — Zinc (for immunity, skin health and libido)
- magnesium – 250 mg/day
- RELATED — Magnesium (for a great night of sleep)
- selenium – 150 mcg/day
- iron – 200 mg/day
- folic acid – 800 mcg/day
- calcium – 1000 mg/day
- RELATED — Calcium (for healthy bones, teeth and heart)
- vitamin D – 400 U/day
- RELATED — Vitamin D: The sunshine hormone for stronger bones
- glutamine – 30 g/day (fuels cells in the small intestines and large bowel and helps with protein losses)[7]
We also suggest looking into probiotics and digestive enzymes, that will assist with digestion and create a healthy microbiome in your gut.
Gluten-free meal plan
| Breakfast | Lunch | Dinner | Snacks |
| Gluten-free toast with eggs and spinach (or scramble tofu for vegan option) | Buddha bowl (quinoa, roast vegetables, fresh salad, protein e.g. chicken, salmon, tofu or chickpeas, avocado) | Gluten-free pesto pasta (can add chicken or plant-based chicken) | Raw cheesecake (great for dessert) Vegetable sticks and hummus |
| Gluten-free cereal with yoghurt (dairy or coconut) with nuts and seeds | Gluten-free sandwiches | Tacos (corn shells, mince or soy mince, carrot, tomato, lettuce, salsa, guacamole, cashew cream) | Rice crackers and cheese Fruit and nuts Chia seed pudding |
| Smoothie | Potato and bacon salad | Teriyaki tofu/chicken and rice with broccoli and sesame seeds | Gluten-free baked goods such as these: Gluten-free orange and lemon cupcakes |
What foods should be avoided and what are the gluten-free alternatives?
Gluten is found in foods such as breads, pastas and cereals. A good way to remember which foods to avoid is BROW – Barley, Rye, Oats and Wheat.[8]
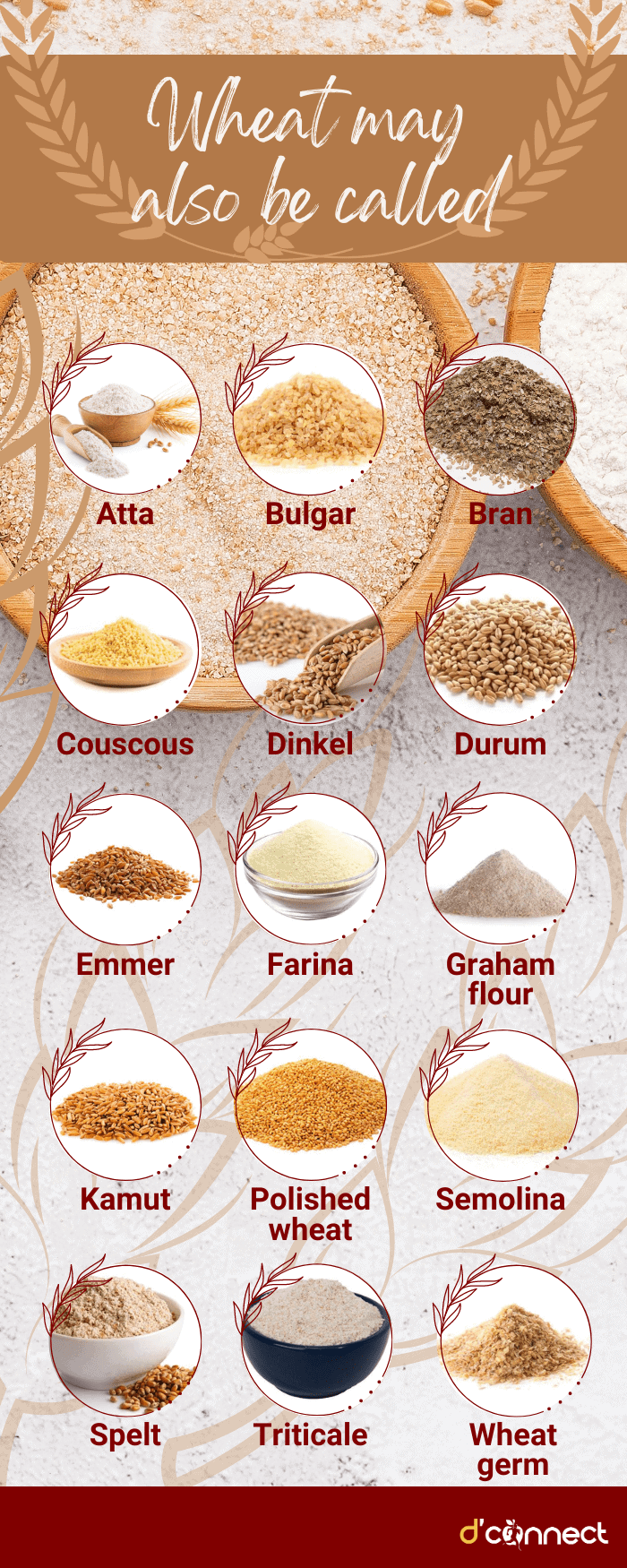
Important note – when looking for alternative to BROW items, keep in mind that wheat may also be called
- atta
- bulgur
- bran
- couscous
- dinkel
- durum
- emmer
- farina
- graham flour
- kamut
- polished wheat
- semolina
- spelt
- triticale
- wheat germ[9]
Gluten can also be found in food starch, preservatives and stabilizers, as well as some household products such as medicine, vitamins/minerals and lip balms.[8]
If you do have coeliac disease and not just gluten intolerance, you need to watch out for cross-contamination, especially in corn and rice products.
Some products that don’t have gluten in the ingredients list can still be manufactured in a factory with other products that contain gluten.
Reading food labels is vital for individuals with coeliac disease
Due to New Zealand food standards, gluten and wheat are identified on all food labels in New Zealand and Australia, so always check the label.[8]
Related Questions
1. Should I be gluten-free if I don’t have coeliac?
Unless you get coeliac-like symptoms from eating gluten, there is no reason not to include gluten-containing foods in your diet.
Breads, pastas and cereals can provide essential nutrients and energy. However, those that test positive for coeliac disease, but are asymptomatic are still at risk for long-term health complications.
2. What are my chances of having gluten intolerance or a wheat allergy?
The global prevalence of having a gluten intolerance and/or wheat allergy is between 0.5-1%.[10]
3. What symptoms are most distinguishable between coeliac disease, gluten intolerance and wheat allergy?
Wheat allergy and gluten intolerance can produce IBS-like symptoms including nausea and bloating.
Coeliac disease affects other areas of the body more severely and can include symptoms such as fatigue and weight loss.
4. Is a gluten-free diet healthy?
A gluten-free diet is essential for the health of people with coeliac disease.
5. Which foods are made from gluten?
Gluten is found in breads, pastas and cereals, a common acronym to remember gluten-containing foods is BROW – barley, rye, oats and wheat.
6. Can you develop coeliac disease from eating too much gluten?
No. There is no evidence to date that shows that a diet high in gluten can lead to developing coeliac disease.
If you are looking for gluten-free meal and snack ideas, we suggest seeing our Recipes.
Having passion for mental health and nutrition, Carly’s goal is to become a registered psychologist with a focus on self-care – food, exercise, and sleep. She has a special interest in various mental health disorders, plant-based diets, and the relationship between food and mood.
Through evidence-based research, holistic approach to health and personal experience, Carly hopes to empower others’ well-being.
Carly is a part of the Content Team that brings you the latest research at D’Connect.
References
(1) Patel N, Samant H. Wheat allergy. InStatPearls [Internet] 2021 Jul 18. StatPearls Publishing. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK536992/
(2) Parzanese I, Qehajaj D, Patrinicola F, Aralica M, Chiriva-Internati M, Stifter S, Elli L, Grizzi F. Celiac disease: From pathophysiology to treatment. World journal of gastrointestinal pathophysiology. 2017 May 15;8(2):27. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5437500/
(3) Catassi C, Verdu EF, Bai JC, Lionetti E. Coeliac disease. The Lancet. 2022 Jun 9. Retrieved from: https://www.sciencedirect.com/science/article/pii/S0140673622007942?casa_token=w8XbH3tRHvoAAAAA:lS1bX0FQ9YlWXmrilrPj_oFEqm_gojhIHWaaq74n7FKH-LctjOOcKAbqbeSHitwu7LT8iF_k5w
(4) Melinda Dennis. Do I have to avoid dairy products? National Celiac Association Forum. 2020. Accessed online, retrieved from: https://nationalceliac.org/celiac-disease-questions/if-you-have-celiac-disease-do-you-also-have-to-avoid-dairy-products/
(5) Gluten-Free Society. 9 health benefits of fasting for celiacs. 2023. Accessed online, retrieved from: https://www.glutenfreesociety.org/9-health-benefits-of-fasting/
(6) Rondanelli M, Faliva MA, Gasparri C, Peroni G, Naso M, Picciotto G, Riva A, Nichetti M, Infantino V, Alalwan TA, Perna S. Micronutrients dietary supplementation advices for celiac patients on long-term gluten-free diet with good compliance: a review. Medicina. 2019 Jul 3;55(7):337. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6681258/
(7) Mary Flesher. What is Glutamine? GI Society, Canadian Society of Intestinal Research. Jun 2004. Accessed online, retrieved from: https://badgut.org/information-centre/health-nutrition/glutamine/#:~:text=Celiac%20disease%3A%20Ongoing%20studies%20on,people%20with%20short%20bowel%20disease.
(8) Health Navigator New Zealand. Coeliac Disease (2022 Jun 21). Accessed 2022 Oct 2. Retrieved from: https://www.healthnavigator.org.nz/health-a-z/c/coeliac-disease/
(9) Health Navigator New Zealand. Gluten-free diet (2022 Jul 11). Accessed 2022 Oct 2. Retrieved from: https://www.healthnavigator.org.nz/healthy-living/g/gluten-free-diet/
(10) Sam Mehmet. Study reveals why wheat and gluten intolerance is becoming more common. New Food Magazine. 2020 Aug 12. Accessed online, retrieved from: https://www.newfoodmagazine.com/news/115778/study-reveals-why-wheat-and-gluten-intolerance-is-becoming-more-common/#:~:text=It%20has%20long%20been%20known,adult%20population%20is%20affected%20worldwide






