Joyce Roberts
BHSc Nsg, Post Grad Cert Adv Nsg, Post Grad Dip Adv Nsg, Accredited Diabetes Nurse Specialist
Note — The article was checked and updated November 2024.
Apart from microvascular diseases, which we discussed in our previous article, poorly managed blood sugar levels can also lead to macrovascular diseases.
These health complications can manifest as
- Heart attack
- Stroke
- Artritis
- Liver disease
- Skin infections (that can lead to amputation).
Also, the lifelong impact of living with diabetes can cause depression, which can then lead towards low general health and wellbeing.
Education and sharing important information on diabetes is therefore needed to ensure that people with diabetes keep on top of their health, both physical and mental, which is why we outlined in this article some of the most important areas to be aware and mindful of, and we encourage you to share this information.
Macrovascular diseases
Macrovascular complications include
- Coronary artery disease
- Cardiomyopathy
- Arrhythmias
- Cardiovascular disease
- Peripheral arterial disease
Macrovascular complications are not necessarily specific to diabetes but tend to occur at an earlier age and are more common in people with diabetes.
They are a major cause of morbidity and mortality, especially among individuals with type 2 diabetes due to ongoing poor control of diabetes.
RELATED — Diabetes untreated (Part 1): Microvascular diseases
Poor lifestyle habits are a risk factor for developing heart disease
Apart from poor lifestyle habits, other well-known risk factors for developing heart disease are hypertension, dyslipidemia and obesity. Other significant risk factors include:
- Poorly controlled diabetes (blood sugar levels)
- Metabolic syndrome
- Diabetic nephropathy
- Possible cardiomyopathy
- Hemostatic factors
- Other biochemical risk factors such as homocysteine or c-reactive protein
The central pathological mechanism in macrovascular disease is the process of atherosclerosis. The fatty, fibrous plaques that have developed progressively narrow the coronary artery lumens.
This then reduces the flow and volume of blood, which can lead to heart tissue death.[1]
Stroke and diabetes
A stroke occurs due to a sudden interruption of the blood supply to the brain.
People with type 2 diabetes have a significant increase in risk of having a stroke
There are three types of stroke which are:
- Ischaemic
- Embolic
- Hemorrhagic
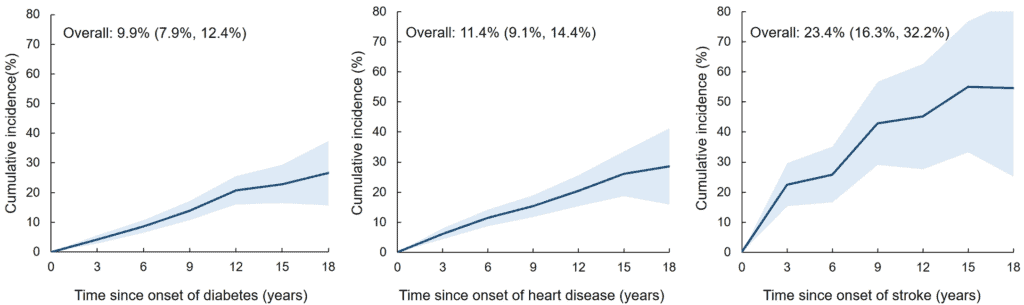
Source: Jones, M. Progression of diabetes, heart disease, and stroke multimorbidity in middle-aged women: A 20-year cohort study. (2018)
Ischaemic stroke is the most common of the strokes and occurs when a clot blocks an artery in the brain. The clot has formed in a small blood vessel in the brain due to the narrowing caused by the presence of diabetes, hypertension or high cholesterol.
Embolic stroke occurs due to a blood clot or piece of plaque (cholesterol or calcium deposits) on the wall of an artery breaking loose and traveling to the brain, blocking the flow of blood.
Hemorrhagic stroke occurs due to an artery in the brain rupturing and leaking blood into the brain. The stroke occurs due to parts of the brain being deprived of blood.[2]
Diabetes and thyroid disease
These two diseases appear to be closely linked as thyroid hormones have marked effects on glucose homeostasis.
Both hypothyroidism and hyperthyroidism are found at an increased frequency in those with either type 1 or 2 diabetes.
Research also shows that a person with diabetes and thyroid dysfunction is at an increased risk of developing cardiovascular disease.
Link between diabetes and depression
Depression is a mental disorder affecting millions of people worldwide. It is characterized by a persistent sadness and a lack of pleasure in life.
Research suggests depression is common in people with diabetes because the numerous tasks associated with managing the illness can be a burden.[3]
Diabetes-related distress is becoming more commonly recognised because of
- Significant negative emotional reactions to the diagnosis of diabetes
- Distress due to high risk of complications
- Self-management demands
- Unresponsive providers and/or unsupportive interpersonal relationships.
Symptoms associated with depression may be elevated in the person with diabetes but not severe enough to be classed as a depression.
Ongoing studies are suggesting that it is time to recognise that emotional distress associated with diabetes should be considered a common component and has the potential to indicate an increased risk for poor treatment outcomes.
Arthritis and increase in inflammation
Research shows that the link between arthritis and diabetes stems from inflammation.[4]
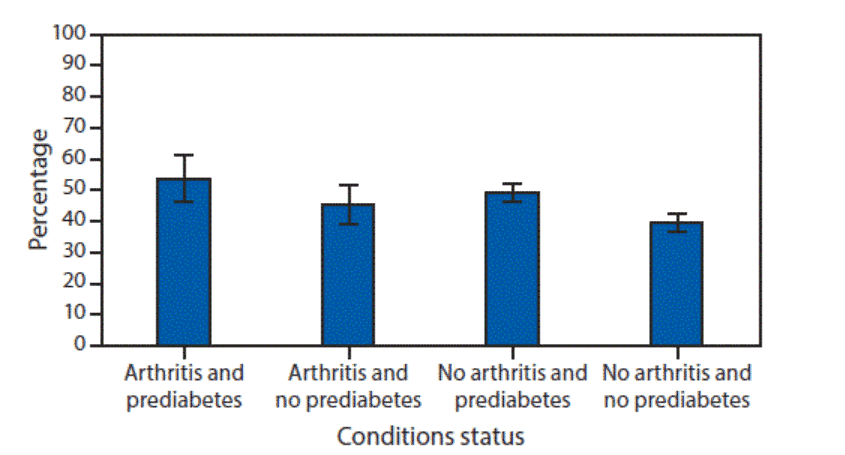
Source: Murphy, L., B. Prevalence of Arthritis Among Adults with Prediabetes and Arthritis-Specific Barriers to Important Interventions for Prediabetes — United States, 2009–2016. (2018)
Genetics and other risk factors like obesity and sedentary lifestyle are also involved.
The person with type 1 or type 2 diabetes appears to have higher concentrations of the cytokines, inflammatory substances such as tumor necrosis factor alpha (TNF-alpha) and interleukin 6 (IL-6) causing the inflammation.
Risk of osteoporosis due to diabetes
Osteoporosis is a metabolic bone disorder in which the rate of bone resorption accelerates and the rate of bone formation decelerates, resulting in soft bones that fracture easily.
Osteoporosis is divided into primary osteoporosis and secondary osteoporosis. While primary osteoporosis occurs as a natural process of aging, secondary osteoporosis develops due to an underlying disease such as diabetes.[5]
Alzheimer’s disease and increase in dementia
Alzheimer’s is one type of dementia marked by mental deterioration.
Alzheimer’s disease and diabetes have been found to share various pathophysiological mechanisms, including alterations in insulin signaling, defects in glucose transporters and mitochondrial dysfunctions in the brain.[6]
Alzheimer’s is a progressive degeneration of the cerebral cortex
Research shows that diabetes affects the processing of amyloid-β and tau, and might increase the rate of formation of senile plaques and neurofibrillary tangles, the main neuropathological hallmarks of Alzheimer’s disease.
Diabetes and impact on liver disease
NAFLD is characterized by excessive fat build-up in the liver without another clear cause such as alcohol use.[7] Nonalcoholic fatty liver disease (NAFLD) is on the rise due to
- Rising levels of obesity
- Type 2 diabetes
- Metabolic syndrome
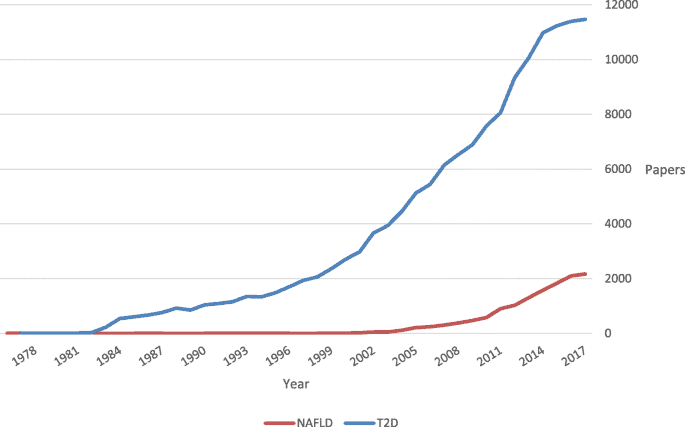
Source: Tomah, S. Nonalcoholic fatty liver disease and type 2 diabetes: where do Diabetologists stand? (2020)
NAFLD is a spectrum disease that includes
- Fatty liver
- NASH (nonalcoholic steatohepatitis)
- Fibrosis
- Cirrhosis
NAFLD places the person with type 2 diabetes at an increased risk of developing or dying from cardiovascular disease.
Diabetes and risk of infections
Diabetes increases our susceptibility to infections, due to its association with reduced response of T-cells, neutrophil function and disorders of humoral immunity.[8]
Ear infections
Common ear infections in diabetics include
- Acute otitis externa (Swimmer’s ear)
- Malignant otitis externa
- Otomycosis.[8]
Acute otitis externa is a form of cellulitis involving the skin and subdermis of the external auditory canal.
Malignant otitis externa is an invasive and aggressive infection of the external auditory canal which can also extend to the skull base.
The two most common bacteria involved in otitis externa infections are pseudomonas aeruginosa and staphylococcus aureus.
Otomycosis is a fungal ear infection of the outer canal, where fungal species involved are candida and aspergillus.
Important to mention – is that there is a growing body of research that confirms the increased prevalence of hearing loss in people with type 1 and type 2 diabetes.
Our inner ear relies on healthy blood vessels to support hearing, and ongoing hyperglycemia can damage the small blood vessels and nerves in the inner ear, leading to hearing loss.
Foot infections
Corns and calluses
Corns and calluses are common problems caused by repeated pressure of the same area of the foot. This then causes a thickening of the skin, while the tissue underneath can be bruised and infected, which can potentially create an ulcer.
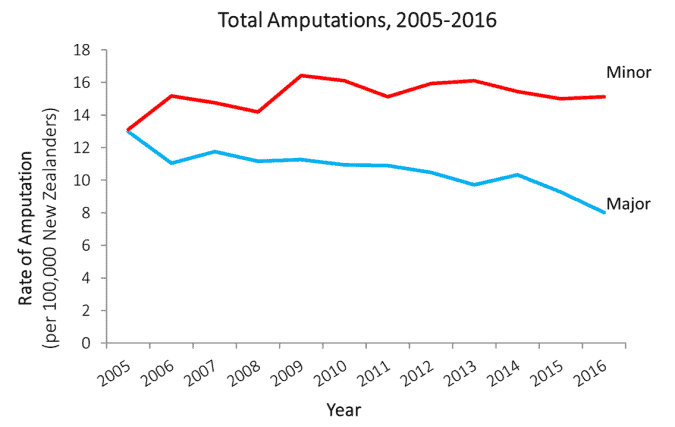
Source: Gurney, K., J. Lower-limb amputation in New Zealand: temporal changes and the role of diabetes mellitus. (2018)
Poor eating habits and poor foot care increase the risk of developing significant problems that can lead to amputations.
People with diabetes are at a high risk of amputations
Fungal food infections
The two most common forms of fungal infections are:
- Tinea pedis (athlete’s foot)
- Onychomycosis (nail infection).
Both need to be treated immediately to prevent secondary bacterial infection and cellulitis.
Patients with diabetes are particularly susceptible to foot infections primarily because of neuropathy, vascular insufficiency and diminished neutrophil function.[9]
Cellulitis
An acute bacterial infection of the subcutaneous tissue, cellulitis specifically affects the dermis and subcutaneous tissue and can spread rapidly.
Cellulitis presents as a red, painful swollen area that also is warm to the touch.
The way cellulitis occurs is when the bacteria enters through a break in the skin or is an extension of a current wound, ulcer or trauma. The two most common bacteria involved are
- Streptococcus pyogenes
- Staphylococcus aureus
The commonly affected area is the lower legs, but it can occur elsewhere such as face, arms or other areas.[9]
If left untreated, the infection can spread to the lymph nodes and bloodstream and quickly become life-threatening.
Diabetes and skin appearance
People suffering from diabetes are prone to developing a range of skin conditions, which we have covered below.
Diabetic dermopathy
This is one of the most commonly seen skin problems in the person with diabetes, and it appears as
- light brown or reddish
- oval or round
- slightly indented patches of skin.
Studies are showing that diabetic dermopathy occurs more frequently in diabetic patients with retinopathy, neuropathy and nephropathy. It also appears to be closely linked to poorly controlled blood sugar levels.
Diabetic bullae
This skin condition is a rare and distinct marker for diabetes, which is also known as bullosis diabeticorum. It appears as blister-like lesions that occur spontaneously on the feet and heads of diabetics.
Diabetic stiff skin
Mostly associated with long-term type 1 diabetes, diabetic stiff skin is thought to have developed due to the reaction of glucose with proteins in the skin and increased glycation end products.
This causes restricted mobility in the joints of the hands and stiff, waxy, thickened yellow skin.
Acanthosis nigricans
Acanthosis nigricans is a dark, coarse, thickened skin area predominantly seen in flexures and in the neck folds of people with diabetes.

It is mainly associated with insulin resistance and metabolic syndrome.
Insulin site hypertrophy
This is a common complication in insulin-treated patients. It appears as a soft lump, often with irregular contours, in the areas where insulin is being injected repetitively and, possibly, with poor technique.
This potentially leads to unpredictable absorption of injected insulin, leading to poor diabetes management.
Related Questions
1. What are the most common complications of diabetes?
Common complications of diabetes occur due to poor management of blood sugars levels. These are eye problems, foot ulcers, kidney disease and heart attacks or strokes.
2. What top three things should a person with diabetes avoid?
Diabetes management is about how lifestyle, daily routine and technology can affect blood glucose levels. The three highly recommended tips are to avoid highly sweetened foods, such as fruit juice, smoking and gaining weight.
3. Which fruit is best for people with diabetes?
Fruits that are low in the glycemic index and high in fibre such as berries, apricots, plums, peaches, apples and kiwifruit.
If you would like to learn more about diabetes, we suggest reading Diabetes – Early Signs, Causes, Types and Treatment. Also, if you have any questions, please let us know in the comments below.
Joyce has been nursing since the 1980s, and for the past 20 years she has been focusing on patients with diabetes.
Given that diabetes can be a debilitating disease if not managed properly, Joyce’s focus is to ensure that individuals with diabetes have all the correct information. She works diligently and her focus is to prepare, inform and make sure that the individuals are well equipped with knowledge and support to live with the disease 24 hours a day.
References
(1) McCance, K. L., & Huether, L. E. (2010). Pathophysiology: The biologic basis for disease in adults and children. Mosby.
(2) Diabetes UK. (n.d.). Diabetes and stroke. Diabetes UK. Retrieved from https://www.diabetes.org.uk/guide-to-diabetes/complications/stroke
(3) Gonzalez, J. S., Fisher, L., & Polonsky, W. H. (2011). Depression in Diabetes: Have we been missing something important? Diabetes Care, 34(1), 236–239. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3005471/
(4) Rath, L. (n.d.). Rheumatoid arthritis and type 2 diabetes. Arthritis Foundation. Retrieved from https://www.arthritis.org/health-wellness/about-arthritis/related-conditions/other-diseases/rheumatoid-arthritis-and-type-2-diabetes
(5) Brown, S. (2004, January). Osteoporosis: An under-appreciated complication of diabetes. Clinical Diabetes, 22(1), 10–20. (2004) Retrieved from https://diabetesjournals.org/clinical/article/22/1/10/1411/Osteoporosis-An-Under-appreciated-Complication-of
(6) Rojas, M., Chávez-Castillo, M., Bautista, J., Ortega, Á., Nava, M., Salazar, J., Díaz-Camargo, E., Medina, O., Rojas-Quintero, J., & Bermúdez, V. (2021). Alzheimer’s disease and type 2 diabetes mellitus: Pathophysiologic and pharmacotherapeutics links. World Journal of Diabetes, 12(6), 745–766. Retrieved from https://doi.org/10.4239/wjd.v12.i6.745
(7) Hazlehurst, J. M., Woods, C., Marjot, T., Cobbold, J. F., & Tomlinson, J. W. (2016). Non-alcoholic fatty liver disease and diabetes. Metabolism: Clinical and Experimental, 65(8), 1096–1108. Retrieved from https://doi.org/10.1016/j.metabol.2016.01.001
(8) Casqueiro, J. , Casqueiro, J., & Alves, C. (2012). Infections in patients with diabetes mellitus: A review of pathogenesis. Indian Journal of Endocrinology and Metabolism, 16(Suppl1), S27–S36. Retrieved from https://doi.org/10.4103/2230-8210.94253
(9) Bader, M. S. (2008). Diabetic foot infection. American Family Physician. 78(1), 71–79. Retrieved from https://www.aafp.org/pubs/afp/issues/2008/0701/p71.html