
Tiana Hape-Cramond
(Associate Registered Nutritionist)
Jump to:
In the previous article What is the function of amino acids in our body we looked at the benefits of amino acids. Today, we’ll see how high consumption of amino acids can negatively affect:
- asthma
- cardiovascular health
- diabetes
- digestion
- kidneys
If you’re planning a diet higher in protein, either plant or animal protein, we suggest reading the article and see which amino acids can have a less than desirable effect on your health.
Asthma and excess intake of amino acids
Asthma is a chronic respiratory disease characterised by airway inflammation, narrowing of the airways, and difficulty breathing.
There is evidence to suggest that excess consumption of amino acids, particularly histidine, may play a role in the development or exacerbation of asthma.
This may be due to the production of histamine, a molecule involved in allergic reactions and inflammation.
Histidine is converted to histamine
Excess histidine intake can increase histamine production, leading to airway inflammation and bronchoconstriction, which are hallmarks of asthma.[1]
Another mechanism involves the formation of advanced glycation end products (AGEs), which are formed when proteins and sugars react in the body.
This reaction commonly occurs when proteins and sugars are roasted or broiled at high temperatures.[2]
Excess amino acids, particularly lysine and arginine, which are commonly found in:
- fish
- chicken
- gelatine
- wheat germ
- oats
can contribute to the formation of AGEs, which have been shown to be high levels in the airways of people with asthma.[3]
AGEs can also trigger inflammation and oxidative stress, which can contribute to the development or exacerbation of asthma.[4]
Cardiovascular health and amino acid intake
Excess of amino acids in the body can contribute to heart problems by:
- elevating levels of homocysteine
- promoting the production of reactive oxygen species
- disrupting lipid metabolism
The excess intake of protein (over 2g of protein per kg of body mass), which is made up of amino acids, can lead to an increase in the workload on the heart.
This is because the body needs to process the excess amino acids and eliminate the waste products, such as urea and ammonia, through the kidneys.
This results in an increase in blood flow to the kidneys, putting additional strain on the heart.[5]
Some amino acids, such as methionine, can contribute to the formation of homocysteine, which is a compound that can damage blood vessels and increase the risk of heart disease.
Elevated levels of homocysteine have been linked to an increased risk of heart attack and stroke.[6]
Amino acids can also affect lipid metabolism, which can contribute to the development of heart disease. For example, high levels of the amino acids:
- leucine
- arginine
- valine
- proline
- phenylalanine
- isoleucine
- lysine
have been linked to an increase in triglyceride levels, which are a risk factor for heart disease.[7]
The amino acid homocysteine has been shown to have an effect on lipid metabolism as an increase of homocysteine decreases HDL levels by inhibiting the synthesis.[8]
Type 2 diabetes and branched-chain amino acids connection
Insulin resistance is a hallmark of type 2 diabetes, and some studies have suggested that certain amino acids may contribute to insulin resistance.
Branched-chain amino acids (BCAAs) such as leucine, isoleucine, and valine have been linked to insulin resistance in both animal and human studies.[9,10]
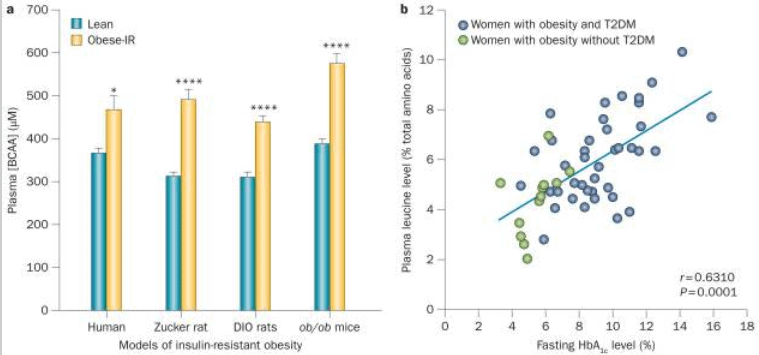
It’s still unclear how BCAAs might contribute to insulin resistance, but one theory is that they interfere with insulin signaling in cells.[11]
Amino acids may also be involved in the development of diabetic complications, such as:
- diabetic nephropathy (kidney disease)
- retinopathy (eye disease)
RELATED — Diabetes Untreated (Part 1): Microvascular diseases and health risks
For example, high levels of certain amino acids, such as homocysteine, have been linked to an increased risk of diabetic nephropathy.
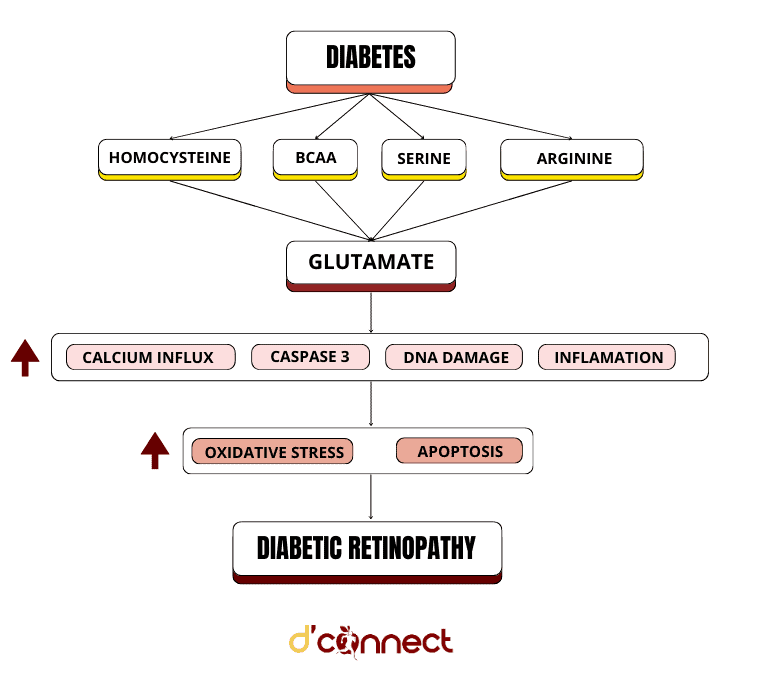
Similarly, elevated levels of homocysteine, serine, BCAA, arginine, and glutamate in the blood have been associated with an increased risk of retinopathy in people with diabetes.[12]
Gastrointestinal distress (bloating and diarrhea) due to high intake of amino acids
Excess of amino acids can lead to gastrointestinal distress because amino acids can be difficult for the body to digest and absorb.
When the body takes in more protein than it needs, the excess amino acids are broken down and processed by the liver.
Meals containing more than 40g of protein are not seen to be more beneficial than meals containing 30g of protein.[13]
Aim for max of 40g of protein per meal
If the liver is overwhelmed by the excess amino acids, it may not be able to process them efficiently, which can lead to a buildup of ammonia and other toxins in the bloodstream.
These toxins can then irritate the lining of the gastrointestinal tract, leading to symptoms such as:
- bloating
- gas
- diarrhea
- nausea
Amino acids alanine and arginine intake above 50g cause nausea and abdominal cramping.[14]
It is highly unlikely to reach these dosages as there is roughly 0.5 to 1g of beta-alanine in a 113g cut of steak and in a supplement there is 1.6g of beta-alanine in a serving.
For arginine, there is 16.2g in a turkey breast, whereas L-arginine supplements contain 1.0g of arginine.[15]
In addition, excess amino acids can also disrupt the balance of beneficial bacteria in the gut, which can further contribute to gastrointestinal distress.
A study found that excess amino acids, specifically methionine, could promote the growth of certain bacteria that are associated with inflammatory bowel disease (IBD).
Methionine enhanced the growth of the bacterium Bilophila wadsworthia, which has been linked to IBD in humans.[16]
It’s important to note that excessive amino acid intake is not the only cause of gastrointestinal distress and that other factors, such as food intolerances, infections, and stress, can also play a role.
Increased risk of gout with diet high in amino acids
Amino acids can play a role in the development of gout by contributing to the formation of uric acid.
Purines are nitrogen-containing compounds that are broken down in the body to form uric acid.
Purines are found in many foods, including those that are high in protein, such as meat, fish, and poultry.
When purines are broken down, they release amino acids, which can contribute to the formation of uric acid. Therefore, a diet high in purine-rich foods can increase the risk of gout.[17]
The amino acids glycine, glutamate, and serine when used in large amounts contribute to the the formation of uric acid in gout.[18]
Hypotension and link with amino acids intake
Some amino acids such as arginine and citrulline can be converted to nitric oxide (NO) in the body, which helps to relax blood vessels and lower blood pressure.[19,20]
Excessive nitric oxide production can cause hypotension
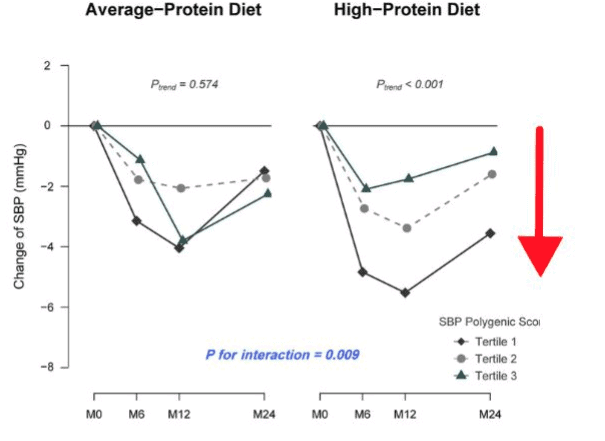
Source: Sun, D. Genetic Susceptibility, Dietary Protein Intake, and Changes of Blood Pressure. (2019)
The renin-angiotensin-aldosterone system (RAAS) plays an important role in regulating blood pressure, and amino acids can affect its activity.[21]
Amino acids, such as tyrosine, have been shown to have an inhibitory effect on the RAAS.[22]
Amino acid phenylalanine is converted to tyrosine in the body, which can then be used to synthesise the neurotransmitter dopamine.
Dopamine has been shown to have a vasodilatory effect, meaning that it can widen blood vessels and potentially lower blood pressure.[23]
The urinary system and impact on kidneys
Excessive intake of amino acids can also lead to impaired kidney function over time, as the kidneys are continually working to process and eliminate the excess amino acids and waste products.
This can lead to kidney damage and even kidney failure in severe cases.[24]
The amino acid cystine can contribute to the formation of kidney stones when present in excess amounts. This is also present in cystinuria where cystine can leak into the urine and create kidney stones.[25,26]
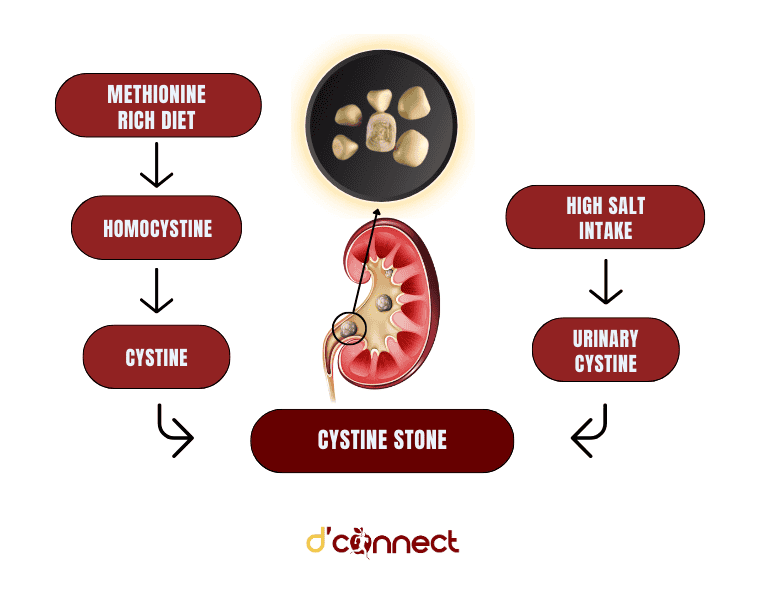
It is important to consume amino acids in moderation as part of a balanced diet to prevent kidney overload and maintain optimal kidney health.
Related Questions
1. Which amino acid has the most negative effect on health if taken in excess amounts?
The amino acids that are most toxic in humans and animals are methionine, cysteine and histidine.
These amino acids not only have acute effects, but also taken in large amounts overtime can increase the risk of tissue damage, high cholesterol and potentially chronic diseases.[14]
2. Which amino acid is best for heart health?
There are many amino acids that are essential for maintaining a healthy heart. It is difficult to say which one is best for heart health.
However, taurine is important for heart health as it has cardioprotective effects.[27]
L-arginine, L-carnitine, glycine and proline are also important for heart health.
3. Which amino acids can help with gout?
The amino acid glycine enhances urinary excretion of uric acid which can help those with gout.
It’s important to know that amino acids in the correct amounts, and from a diverse diet, are very important for our healthspan and longevity.
This is why we suggest reading What are Amino Acids and what is their role in keeping us healthy?
Tiana is an Associate Registered Nutritionist who has a passion for public health and education. Working towards a Master’s in Nutrition Practice with a Bachelor’s in Human Nutrition, Tiana has a personal interest in healthy heart nutrition and promoting positive lifestyle behaviours.
Tiana is a part of the Content Team that brings you the latest research at D’Connect.
References
(1) Yoshikawa T, Naraoka S, Goto-Inoue N, Hayasaka T, Setou M. Elevated histidine decarboxylase expression in asthmatic airways and its modulation by food-derived proanthocyanidins. Free Radic Biol Med. 2019;135:77-87. doi: 10.1016/j.freeradbiomed.2019.02.006
(2) Uribarri J, Woodruff S, Goodman S, et al. Advanced glycation end products in foods and a practical guide to their reduction in the diet. J Am Diet Assoc. 2010;110(6):911-916.e12. doi: 10.1016/j.jada.2010.03.018
(3) Poulsen MW, Hedegaard RV, Andersen JM, de Courten B, Bügel S, Nielsen J, Skibsted LH, Dragsted LO. Advanced glycation endproducts in food and their effects on health. Food Chem Toxicol. 2013 Oct;60:10-37. doi: 10.1016/j.fct.2013.06.052. Epub 2013 Jul 16. PMID: 23867544.
(4) Perkins TN, Donnell ML, Oury TD. The axis of the receptor for advanced glycation endproducts in asthma and allergic airway disease. Allergy. 2021 May;76(5):1350-66.
(5) Link Between Chronic Kidney Disease, Diabetes, and Heart Disease. (n.d.). Centers for Disease Control and Prevention.
(6) Lentz SR. Homocysteine and vascular dysfunction. Life sciences. 1997 Aug 22;61(13):1205-15.
(7) Mook-Kanamori DO, Römisch-Margl W, Kastenmüller G, Prehn C, Petersen AK, Illig T, et al. Increased amino acids levels and the risk of developing of hypertriglyceridemia in a 7-year follow-up. Journal of Endocrinological Investigation [Internet]. 2014 Jan 9 [cited 2023 Mar 22];37(4):369–74. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3972444/
(8) Barter PJ, Rye KA. Homocysteine and Cardiovascular Disease. Circulation Research [Internet]. 2006 Sep 15 [cited 2023 Mar 22];99(6):565–6. Available from https://www.ahajournals.org/doi/10.1161/01.RES.0000243583.39694.1f
(9) Shih CC, Shih YL, Chen JY. The association between homocysteine levels and cardiovascular disease risk among middle-aged and elderly adults in Taiwan. BMC cardiovascular disorders. 2021 Dec;21:1-8.
(10) Lynch CJ, Adams SH. Branched-chain amino acids in metabolic signalling and insulin resistance. Nature Reviews Endocrinology [Internet]. 2014 Oct 7 [cited 2023 Mar 25];10(12):723–36. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4424797/
(11) Yoon MS. The Emerging Role of Branched-Chain Amino Acids in Insulin Resistance and Metabolism. Nutrients [Internet]. 2016 Jul 1 [cited 2023 Mar 22];8(7):405. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4963881/
(12) Aldosari DI, Malik A, Alhomida AS, Ola MS. Implications of Diabetes-Induced Altered Metabolites on Retinal Neurodegeneration. Frontiers in Neuroscience [Internet]. 2022 Jul 13 [cited 2023 Mar 22];16. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9328693/#:~:text=Flow%20diagram%20depicting%20the%20effect,vascular%20damage%20in%20diabetic%20retinopathy
(13) Kristi Wempen, R.D.N. (2022) Are you getting too much protein?, Mayo Clinic Health System. Mayo Clinic Health System. Available from https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/are-you-getting-too-much-protein#:~:text=General%20recommendations%20are%20to%20consume,your%20money%20on%20excessive%20amounts
(14) Garlick PJ. The Nature of Human Hazards Associated with Excessive Intake of Amino Acids. The Journal of Nutrition [Internet]. 2004 Jun [cited 2023 Mar 22];134(6):1633S1639S. Available from https://academic.oup.com/jn/article/134/6/1633S/4688868
(15) 5 foods high in arginine (no date) WebMD. WebMD. Available from https://www.webmd.com/diet/top-foods-high-in-arginine#:~:text=White%20meat%20has%20the%20highest,of%20chicken%20has%202.790%20grams
(16) Roy DG, Chen J, Mamane V, Ma EH, Muhire BM, Sheldon RD, Shorstova T, Koning R, Johnson RM, Esaulova E, Williams KS. Methionine metabolism shapes T helper cell responses through regulation of epigenetic reprogramming. Cell metabolism. 2020 Feb 4;31(2):250-66.
(17) Hong F, Zheng A, Xu P, Wang J, Xue T, Dai S, et al. High-Protein Diet Induces Hyperuricemia in a New Animal Model for Studying Human Gout. International Journal of Molecular Sciences [Internet]. 2020 Mar 20 [cited 2023 Mar 25];21(6):2147. Available from https://www.mdpi.com/1422-0067/21/6/2147
(18) Yü TF, Adler M, Bobrow E, Gutman AB. Plasma and urinary amino acids in primary gout, with special reference to glutamine. Journal of Clinical Investigation [Internet]. 1969 May 1 [cited 2023 Mar 26];48(5):885–94. Available from https://www.jci.org/articles/view/106047
(19) Siervo M, Lara J, Ogbonmwan I, Mathers JC. Inorganic nitrate and beetroot juice supplementation reduces blood pressure in adults: a systematic review and meta-analysis. The Journal of nutrition. 2013 Jun 1;143(6):818-26.
(20) Mehta S, Stewart DJ, Levy RD. The hypotensive effect of L-arginine is associated with increased expired nitric oxide in humans. Chest. 1996 Jun;109(6):1550-5. doi: 10.1378/chest.109.6.1550. PMID: 8769510.
(21) Fountain JH, Kaur J, Lappin SL. Physiology, Renin Angiotensin System [Internet]. Nih.gov. StatPearls Publishing; 2023 [cited 2023 Mar 26]. Available from https://www.ncbi.nlm.nih.gov/books/NBK470410/
(22) Tain YL, Hsu CN, Chan JYH. Prenatal high-protein diet leads to hypertension and renal impairment through altered renal nitric oxide synthase expression and plasma nitric oxide bioavailability in rat offspring. Am J Physiol Regul Integr Comp Physiol. 2014;306(4):R282-R292. doi: 10.1152/ajpregu.00299.2013
(23) Tzeng, T. F., Liou, S. S., & Liu, I. M. (2017). The neuroprotective effects of dopamine against hypoxia-induced toxicity on brainstem motor neurons in chicken embryos. International journal of molecular sciences, 18(6), 1245. doi: 10.3390/ijms18061245
(24) Dr Robert Wolfe. Amino Acids and Kidney Disease [Internet]. The Amino Company. The Amino Company; 2018 [cited 2023 Mar 28]. Available from https://aminoco.com/blogs/amino-acids/amino-acids-kidney-disease
(25) Cystine Stones [Internet]. National Kidney Foundation; 2016 [cited 2023 Mar 26]. Available from https://www.kidney.org/atoz/content/what-are-cystine-stones#:~:text=Cystine%20stones%20are%20caused%20by,anywhere%20in%20the%20urinary%20tract.
(26) Kidney stones: Overview [Internet]. Nih.gov. Institute for Quality and Efficiency in Health Care (IQWiG); 2019 [cited 2023 Mar 26]. Available from https://www.ncbi.nlm.nih.gov/books/NBK348937/
(27) Drake KJ, Sidorov VY, McGuinness OP, Wasserman DH, Wikswo JP. Amino acids as metabolic substrates during cardiac ischemia. Exp Biol Med (Maywood). 2012 Dec;237(12):1369-78. doi: 10.1258/ebm.2012.012025. PMID: 23354395; PMCID: PMC3816490. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3816490/#:~:text=Taurine%20is%20a%20very%20important,arrhythmias%20and%20improving%20contractile%20function






