
Lisa Polaczuk
BHSc Acupuncture and Traditional Chinese Medicine, Dip. in Tuina (Chinese Medical Massage), Postgrad Cert in Counseling Principles and Ethics and Critical Psychology, BA Psychology
Acupuncture evolved from the ancient Chinese Medical Practice approximately 3000 years ago. It is used to treat a wide range of issues including
- Digestive health
- Respiratory health
- Pain
- Injuries
- Stress
In this article, we take a look at the nature of acupuncture, its history, and the potential benefits of the treatment.
What is Acupuncture?
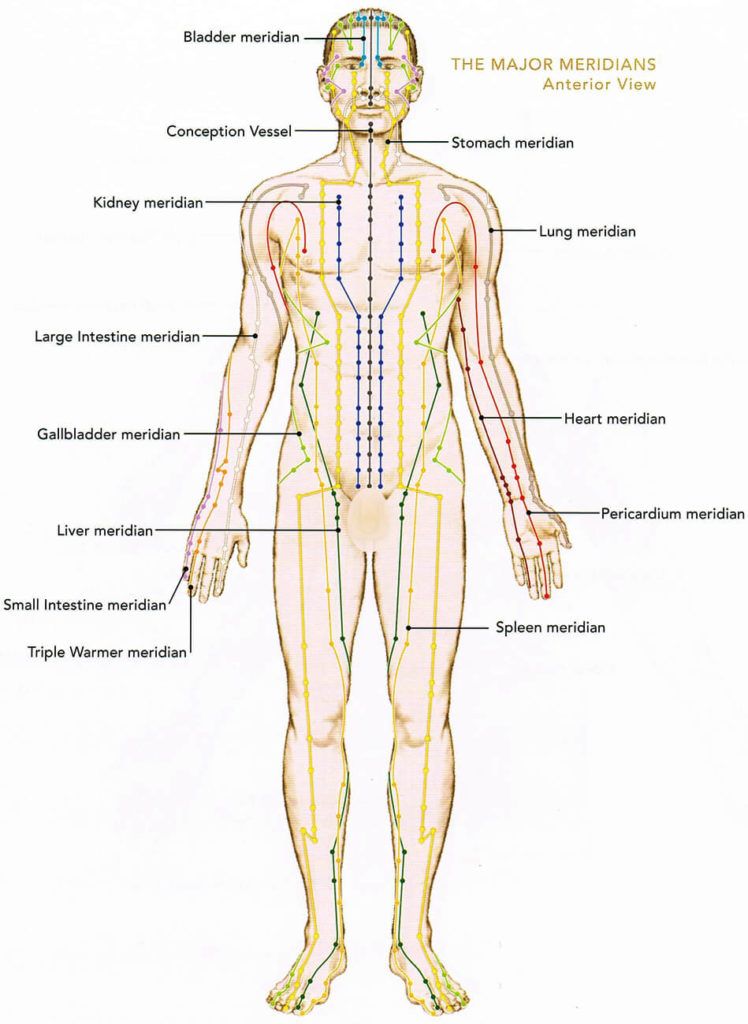
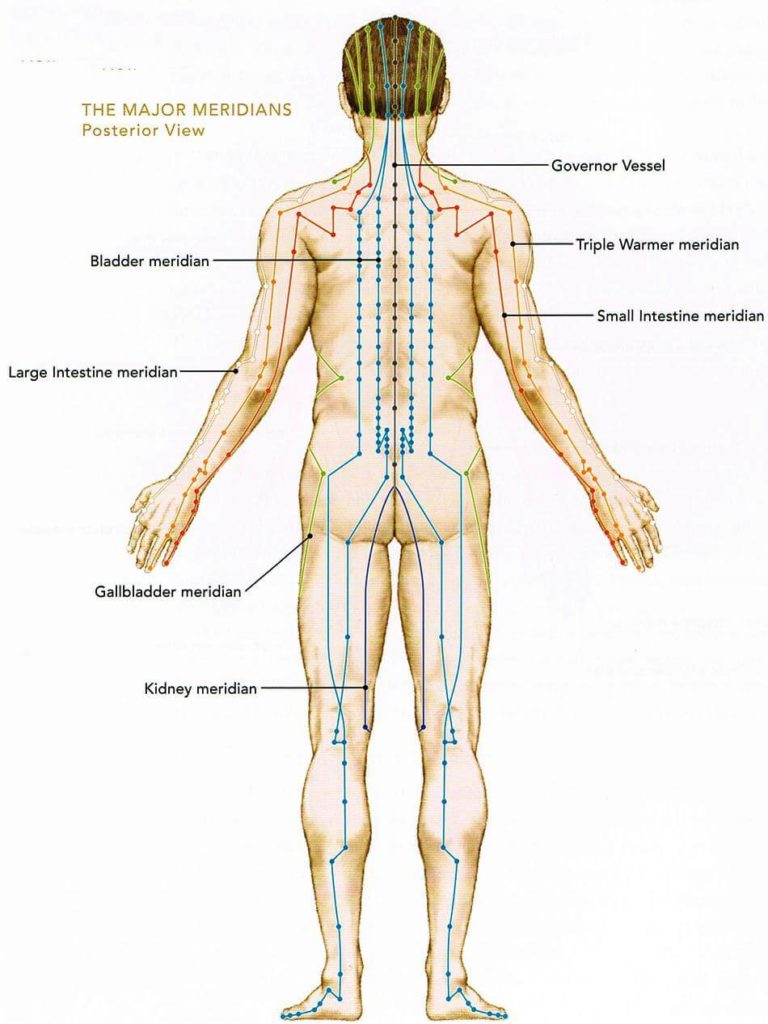
Acupuncture is a method involving the insertion of fine sterilised single-use needles into various acupuncture points located along pathways often called “channels” or “meridians”.
There are 12 main channels, and all have associated organs, bodily structures and functions through which “Qi” energy flows.
In Traditional Chinese Medicine, Qi is vital energy or the life force that exists within us and all around us. When the flow of Qi throughout the body is interrupted through stress, injury and/or life’s circumstances, it creates internal disharmony and ill health may arise.
Acupuncture restores the body’s internal energy flow
The selection of acupuncture points (acupoints) used in treatment is based on thorough questioning in all the different areas of a person’s life and their signs and symptoms.
Various sizes and numbers of needles are inserted at various depths into the body. Needles can be manipulated and retained from 20 to 60 minutes to help restore the balance of Qi for good health and wellbeing.[1]
What is the difference between Acupuncture and other therapies?
The difference between acupuncture and therapies such as Osteopathy, Chiropractic, Massage Therapy, Mirimiri, and Homeopathy is that needles are the tool used to treat patients. Acupuncture literally means to puncture with a needle.
Physiotherapists also use needles as a treatment option, but the approach varies significantly. Physiotherapists perform “dry needling” which involves inserting fine needles into tight bands of muscle tissue using strong manipulative needling techniques to release “trigger points” and/or inserting into superficial areas where a nerve enters the muscle, stimulating an electrical twitch or “motor point” to treat a variety of musculoskeletal pain syndromes.[2]
Acupuncture also uses motor points given acupoints are located in areas with higher concentrations of superficial nerves and nerve bundles.
This does differ, as acupoints are also located in areas with higher concentrations of vascular structures and blood vessels and are higher in electrical conductivity with lower resistance as well as the storing and releasing of electrical current via internal circuits, which may explain Meridian function connected to Acupoints.[3,4,5]
Some physiotherapists or Western/Medical Acupuncturists are trained from a Western perspective but can be educated in some Traditional Chinese Medicine knowledge.
They may include acupuncture points that are based on an evidence-based prescription that a certain point will elicit a certain response or help with a particular injury.
Acupuncturists trained in TCM can treat a far wider range of issues including
- Digestive issues (Irritable Bowel Syndrome (IBS), Crohns symptoms, and chronic indigestion and reflux)
- Respiratory issues (including Emphysema and Chronic Bronchitis)
- Pain and pain conditions
- Injuries, sprains and strains
- Migraines and headaches
- Stress and mental health
- Women’s health issues (Fertility, Pregnancy and Postpartum care as well as Endometriosis, Amenorrhea and Polycystic Ovarian Syndrome (PCOS) [6,7]
RELATED — 5 Natural Remedies for Menopause
History and origin of Acupuncture
Acupuncture evolved from the ancient Chinese Medical Practice of TCM which originated approximately 3000 years ago.[8]
TCM and Acupuncture were practices originally based on traditional myths, legends and ancestry during the Shang Dynasty (approximately 1600-1046 BC).[9]
Illnesses were attributed to unhappy deceased ancestors who were believed to have the power to endanger or destroy human life. Sharpened stones and long bones were identified as being used to “expel” evil ancestors through insertion into the body.
During the Zhou Dynasties (approximately 1100-220 BC) society had an organised medical system where Imperial officials received medical training. Theories about Qi and the interactions and opposites of yin and yang were explored in their relation to health and longevity rather than the influence of ancestors.
The innovative times of the Han Dynasty (206 BC -220 AD) saw intellectual elites further inform TCM through ideas of correspondences between the
- Body (microcosm)
- Cosmos (macrocosm)
- Influence of Wuxing (5 elemental theory)
- Daoism
- Confucianism
and the observation of nature and how it relates to the internal flow of qi and illness in the body.
Acupuncture treatment is an ancient practice used for 3000 years
Chinese medicine continued to expand through the Dynasties but by the 17th Century, the ruling Emperor enforced that acupuncture be banned from medical practice and excluded from the Imperial Medical Institute, based on efforts to modernise medicine.
After the establishment of the Republic of China (1912-1949), Western medical knowledge based in science was permanently introduced to China. In 1949, the Communist Government revived traditional forms of medicine including acupuncture, and the practice started to spread globally alongside the development of acupuncture needles.
Acupuncture was introduced to New Zealand (NZ) in the 1970s by NZ Doctors who had travelled to China to investigate acupuncture. They brought the practice home to use alongside their own conventional therapies.[10]
Notable individuals
One of the most notable influences in Traditional Chinese Medicine and Acupuncture is the translation and analyses of Classical Medical texts. Of note is the Yellow Emperor’s Classic of Internal Medicine (Nei Jing) dated around 100 BCE.[11]
This monumental classic was said to be written by the legendary Huang Di, the Yellow Emperor. The text referred to the Channels in which the Qi flows and locations of Acupuncture points but doesn’t hold record of any description of Acupuncture points themselves.
This classic offers in-depth explanations on ethics, psychology and cosmology in relation to human pathology, health and vitality as well as diagnosis and treatment.
Pioneering medical doctors such as Hua Tao and Zhang Zhongjing offered further insight to acupuncture through the authorship of several texts during the late Han Dynasty (25-220 AD) summarising diagnostic patterns and medicinal practice up until that time.[12]
Dr Huang Fu unified and systematised location and names of acupuncture points plus corrected differences found in older texts compiling the book, “Systematic Classic of Acupuncture and Moxibustion” (256-260). During the Ming Dynasty (1368-1644], renowned Acupuncturist and Physician Yang Jizhou, wrote The Great Compendium of Acupuncture and Moxibustion.
The text showed detailed knowledge of 365 Acupuncture points and descriptions of where to needle on the channels and how to use Acupuncture to treat illness.
Dr Lian Zhu was a notable founder of contemporary acupuncture in modern China-post 1949. A military physician and high ranking officer in the government health care system, she learnt acupuncture in 1945 and became one of China’s most influential trainers, founding the first public acupuncture university.[13]
She was the first scholar to write a book crucial to the establishment of acupuncture as a biomedical practice promoting research methods and acupuncture acceptance by the general public, medical doctors, government officials and international medical societies.
Research on Acupuncture
Due to the scepticism of Western science to understand the mechanisms underlying how acupuncture works and its effectiveness, acupuncture research of the past three decades has transformed this philosophical practice into one of the most evidence-based methods studied and well-documented popularised biomedical treatments globally.
A recent review of acupuncture research trends analysed a total of 13,320 publications over the last 20 years and found acupuncture research had a two-fold growth rate than biomedical research overall and that of the 60 countries conducting the research
- China (47%)
- United States (17.5%)
- United Kingdom (8.2%)
were the biggest contributors.[14]
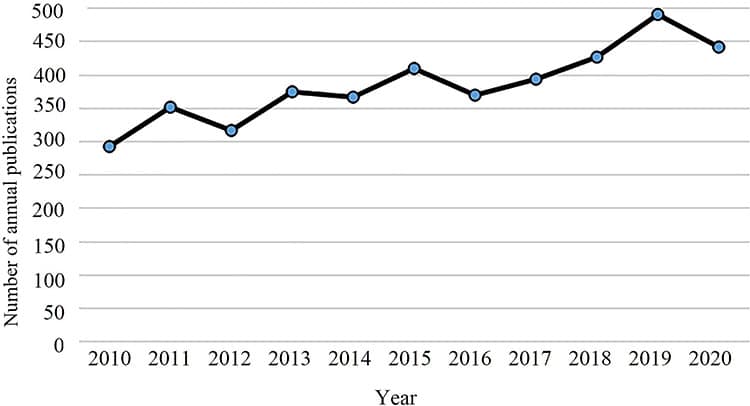
Growth in the proportion of Randomised Control Trials (RCT) and quality of acupuncture published research has grown exponentially.
Another recent review searched relevant medical databases over a 27-year period for clinical guideline recommendations and found 2189 positive recommendations for acupuncture related to 204 pain (107) and non-pain (97) conditions mainly published in North America, Europe and Australasia.[15]
Attributing the underlying mechanism of acupuncture to the placebo effect or sham acupuncture is no longer plausible.
Earlier studies often produced misleading and inaccurate results finding acupuncture to be the same or only slightly better than Sham Acupuncture like, for example:
- A 1976 study, acupuncture was found to be non-significantly superior to sham acupuncture in patients assigned treatment during 16 pain crises for sickle cell anaemia.[16]
- A 1985 study where there was no statistical significance between treating acupuncture versus sham acupuncture in patients with headaches monitored over a 6-week treatment period.[17]
Recent findings that sham acupuncture is an invalid ‘inert’ control, has led to the reexamination of clinical trials and quality of research methods producing more accurate measures of acupuncture effectiveness for certain conditions.[18,19] Here, we can mention two examples:
- The 2013 network analyses of 114 trials comparing acupuncture with other physical treatments for knee osteoarthritis (OA) found in the high-quality studies that acupuncture was statistically significant to sham acupuncture as well as usual care, exercise and weight loss for the treatment of OA pain.[20]
- The 2012 meta-analyses of acupuncture for the treatment of 4 chronic pain conditions – back/neck, OA, headache and shoulder pain found acupuncture to be superior to sham and no acupuncture.[21]
Health benefits of Acupuncture
The most robust acupuncture research comes from Analgesic Acupuncture (AA) and its pain-relieving benefits.
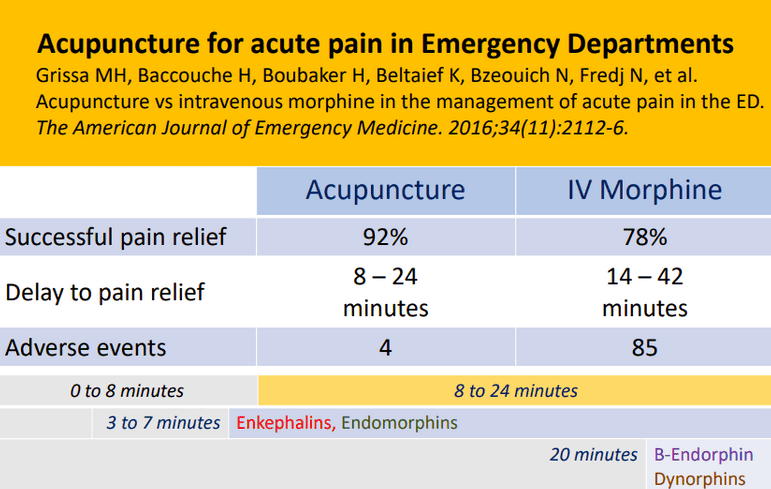
A study in the US found that treating a group of Emergency Department (ED) patients with acute onset moderate to severe pain with acupuncture (150 patients) provides successful, faster and safer pain relief when compared to Intravenous Morphine (IVM) (150 patients).[22]
Another study carried out in the ED of 4 tertiary hospitals in Melbourne Australia for 1964 patients looked at Analgesic Acupuncture for acute lower back pain, ankle sprain and migraine.
They assessed several groups:
- acupuncture alone (177 patients)
- acupuncture and pharmacotherapy (178 patients)
- pharmacotherapy alone (173 patients)
They found no differences in pain scores between the groups in the first hour of treatment and that 48 hours later, 80% of each of the three groups stated they would probably or definitely repeat their treatment.
This study shows acupuncture to be equivalent to pharmacotherapy making acupuncture at least as good as pharmacotherapy for analgesic pain relief, as well as a safe and acceptable form of analgesia for patients.[23]
Analgesic Acupuncture is also effective for chronic pain such as:
- Musculoskeletal pain
- Back and neck pain
- Osteoarthritis
- Chronic headache
- Shoulder pain
where acupuncture was found to be superior for all pain conditions compared to both sham acupuncture and no acupuncture and that the effects of acupuncture persisted over a 12 month period.[21,24,25]
Research suggests acupuncture offers excellent pain relief
Various studies have shown acupuncture triggers opioid/non opioid mediators and has modulating effects on the nervous system which would help to explain the benefits of treating anxiety and depression with acupuncture.[26,27,28,29]
RELATED — Introduction to: Depression
Research also suggests acupuncture may be beneficial for health issues such as
- acute gout and gouty arthritis (by lowering uric acid and alleviating pain)[30]
- hypertension (as it helps to lower both diastolic and systolic blood pressure in those taking antihypertensive medications[[31]
- supplementary therapy in the management of type 2 Diabetes Mellitus (as it improves blood lipids, blood pressure control and weight loss)[32]
RELATED — Diabetes: Early Signs, Causes, Types and Treatment
Acupuncture for women’s health issues is also beneficial including
- reducing menstrual pain and intensity[33]
- reducing chronic pelvic pain and dyspareunia related to Endometriosis[34]
- improving menstrual frequency, hormone regulatory, and fertility by affecting ovulation in women with Polycystic Ovary Syndrome (PCOS)[35,36]
The Acupuncture Evidence Project searched 1,000 systematic reviews along with three network meta-analyses to identify the effect of acupuncture on 117 conditions and in 2017 published strong evidence for the positive effect of Acupuncture for 8 conditions:
- Headaches (tension-type and chronic)
- Migraine prevention
- Chronic lower back pain
- Knee osteoarthritis
- Allergic rhinitis
- Postoperative pain
- Nausea and vomiting, and
- Chemotherapy-induced nausea and vomiting.
A potential positive effect on 38 conditions including:
- Sciatica
- Back or pelvic pain during pregnancy
- Post-traumatic stress disorder
- Menopausal hot flushes
- Perimenopausal and postmenopausal insomnia
RELATED — Why we sleep: The role of sleep in our healthy life
In the next article we will be going into more detail about these conditions.
Side effects and possible risks of Acupuncture
The Acupuncture Evidence Project states that “Acupuncture is considered safe in the hands of a well-trained practitioner”.[37]
In New Zealand, acupuncture has moved into a regulated practice where NZ Acupuncture boards as well as the Chinese Medical Council grant annual practising certificates to Acupuncturists to ensure competent practitioners practise to a high standard and meet the requirements under the Health Practitioners Competence Assurance Act 2003.[38,39]
Side effects and possible risks may still occur and may include
- Temporary markings, bleeding, bruising, swelling and/or hematoma due to the puncture of small, tiny blood vessels
- Dizziness and/or fainting due to preexisting conditions, tiredness, lack of food, drinking alcohol or taking recreational drugs prior to treatment and/or needle apprehension and anxiety
- Skin redness, itching, allergies and infection
- Sensations of a dull aching, numbness, heaviness attributed to the therapeutic effect of acupuncture
- Sharpness or stinging, attributed to insertion into a superficial nerve, hair follicle, or sweat gland
- Bent, stuck or broken needles
Internal organ or nerve injury including pneumothorax.[40,41]
Risks can be avoided when the practitioner has a thorough knowledge of anatomy, considers patient frame, position when needling, needle length and depth.
Related Questions
1. Needles being inserted into the skin sounds painful – how much does it actually hurt?
The fine, tiny needles make for a smooth insertion.
If there is any pain, it is only sharp briefly before disappearing immediately after.
2. Do I need to check with a doctor before seeing an Acupuncturist?
It is encouraged to let your doctor know you may be receiving treatment.
Having your healthcare team work together is the best practice for you.
3. Can I use acupuncture alongside other treatments or pain relief methods?
Yes, using acupuncture alongside other treatments/pain relief methods is supported as acupuncture is a complementary medicine.
Keep an eye on your pain relief methods you may need to reduce them while receiving acupuncture.
Have you tried acupuncture? What effects did you find it had? Share your experiences in the comments below.
Lisa is an Acupuncturist and Traditional Chinese Medicine Practitioner, using the wisdom of TCM and the effectiveness of the needle and other tools to treat pain, injury, and a wide range of health issues including women’s health, stress and mental health.
If you would like to learn more about Lisa, see Expert: Lisa Polaczuk
References
(1) Lu Y, Wang J. (2009). An Inquiry into the Action of Acupuncture on the Human Body by Means of Pharmacology. Journal of Traditional Chinese Medicine. Retrieved from https://www.sciencedirect.com/science/article/pii/S0254627209600522?ref=pdf_download&fr=RR-2&rr=8d967b062c29508b
(2) Dunning J, Butts R, Mourad F et al. (2014) Dry Needling: A Literature Review with Implications for Clinical Practice Guidelines. Physical Therapy Reviews. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4117383/
(3) Gunn C, Ditchburn F, King M et al. (1976). Acupuncture Loci: A Proposal for their Classification According to their Relationship to Known Neural Structures. American Journal of Clinical Medicine.
(4) Liu C, Xiaohua W, Hua Xu et al. (2014). X-Ray Phase Contrast CT Imaging of the Acupoints based on Synchrotron Radiation. Journal of Electron Spectroscopy and Related Phenomena.
(5) Matos L, Lopes L, Freire V et al. (2021). Can the Electrical Potential of Acupoints be used to Assess the Functional State of Meridians and the Effects of Therapeutics? A Exploratory Data Analysis. Journal of Bodywork & Movement Therapies.
(6) National Center for Complementary and Integrative Health (2022). Acupuncture Effectiveness and Safety. Retrieved from https://www.nccih.nih.gov/health/acupuncture-effectiveness-and-safety
(7) McDonald J, Jazz S. (2017). The Acupuncture Evidence Project: A Comparative Literature Review. Australian Acupuncture and Chinese Medicine Association. Retrieved from https://www.asacu.org/wp-content/uploads/2017/09/Acupuncture-Evidence-Project-The.pdf
(8) Zhuang Y, Zing J, Zeng B et al. (2013). History of Acupuncture Research. Int Rev Neurobiology.
(9) Ramey D, Buell P. (2010). A True History of Acupuncture. Focus on Alternative and Complementary Therapies. Retrieved from https://onlinelibrary.wiley.com/doi/full/10.1211/fact.2004.00244
(10) Pollock K. (2018). Alternative Health Therapies. Te Ara- The Encyclopedia of New Zealand. Retrieved from https://teara.govt.nz/en/alternative-health-therapies/page-5
(11) Collingwood A. (2002)TCM Chronology. Integrated Chinese Medicine Holdings Ltd.
(12) Zeng H, Qiao Y, Chen X et al. (2021). History and Development of TCM Case Report in a Real World Setting. Evidence Based Complementary and Alternative Medicine. Retrieved from https://onlinelibrary.wiley.com/doi/10.1155/2021/7402979
(13) Fan A, Alemi S. (2023). Dr. Lian Zhu: A Founder of Contemporary Acupuncture Medicine. Medical Acupuncture. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10440647/
(14) Ma Y, Dong M, Zhou K et al. (2016). Publication Trends in Acupuncture Research: A 20-Year Bibliometric Analysis Based on PubMed. e Collection.
(15) Birch S, Lee M, Alraek T et al. (2018). Overview of Treatment Guidelines and Clinical Practical Guidelines that Recommend the Use of Acupuncture: A Bibliometric Analysis. Journal Complementary Medicine.
(16) Co L, Schmitz T, Havdala H et al. (1979). Acupuncture: An Evaluation in the Painful Crisis of Sickle Cell Anaemia. Pain.
(17) Dowson D, Lewith G, Machin D. (1985).The Effects of Acupuncture Versus Placebo in the Treatment of Headache.
(18) Birch S.(2006). A Review and Analysis of Placebo Treatments, Placebo Effects, and Placebo Controls in Trials of Medical Procedures When Sham is Not Inert. Journal of Complementary and Alternative Medicine. Retrieved from https://www.researchgate.net/publication/7134057_A_Review_and_Analysis_of_Placebo_Treatments_Placebo_Effects_and_Placebo_Controls_in_Trials_of_Medical_Procedures_When_Sham_Is_Not_Inert
(19) Kaptchuk T, Ke-Ji C, Jun S. (2010). Recent Trials of Acupuncture in the West: Responses from Practitioners. Chinese Journal of Integrated Medicine. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC2919856/
(20) Corbett M, Rice S, Madurasinghe V et al.(2013). Acupuncture and other Physical Treatments for the Relief of Pain due to Osteoarthritis of the Knee: network meta-analyse. Osteoarthritis Cartilage.
(21) Vickers A, Cronin A, Maschino A. (2012). Acupuncture for Chronic Pain: Individual Patient Data Meta-analysis. Arch Internal Medicine. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3658605/
(22) Grissa MH, Boubaker H, Beltaief K et al. (2016). Acupuncture vs intravenous morphine in the management of acute pain in the ED. The American Journal of Emergency Medicine.
(23) Cohen M, Smit D, Andrianopoulos N et al. (2017). Acupuncture for analgesia in the emergency department: a multicenter, randomised, equivalence and non-inferiority trial. Medical Journal Australia. Retrieved from https://www.mja.com.au/journal/2017/206/11/acupuncture-analgesia-emergency-department-multicentre-randomised-equivalence#11
(24) Vickers A, Vertosick E, Lewith G et al. (2017). Acupuncture for Chronic Pain: Update of an Individual Patient Data Meta-analysis. Journal Pain. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5927830/
(25) MacPherson H, Vertosick E, Lewith G et al. (2017). The Persistence of the Effects of Acupuncture After a Course of Treatment: A Meta-analysis of Patients with Chronic Pain. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5393924/
(26) Wen G, He X, Lu Y et al (2010). Effect of acupuncture on neurotransmitters/modulators. Acupuncture Therapy for Neurological Disease.
(27) Wen G, He X, Lu Y et al. (2010) Acupuncture-Induced Activation of Endogenous Opioid System. Acupuncture Therapy for Neurological Disease.
(28) Xang X, Yang N, Huang F et al. (2021). Effectiveness of Acupuncture on Anxiety Disorder: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Annals of General Psychiatry.
(29) MacPherson H, Vickers A, Bland M et al. Acupuncture, counselling or usual care for depression (ACUdep): a randomised controlled trial. 2017. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK409485/
(30) Lu W, Zhang J, Lv Z et al. (2016). Update on the Clinical Effect of Acupuncture Therapy with Gouty Arthritis: Systematic Review and Meta-analysis. Evidence-Based Complementary and Alternative Medicine. Retrieved from https://onlinelibrary.wiley.com/doi/full/10.1155/2016/9451670
(31) Li D, Zhou Y, Yang Y et al. (2014). Acupuncture for Essential Hypertension: A Meta-Analysis of Randomised Sham-Controlled Clinical Trials. Evidence-Based Complementary and Alternative Medicine. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3960742/
(32) Chen C, Liu J, Sun M. (2019). Acupuncture for type 2 Diabetes Mellitus: A Randomised Review and Meta-Analysis of Randomised Controlled Trials. Complementary Therapies in Clinical Practice.
(33) Armour M, Dahlen H, Zhu X el at. (2017). The Role of Treatment Timing and Mode of Stimulation in the Treatment of Primary Dysmenorrhea with Acupuncture: A Exploratory Randomised Controlled Trial. PLOS ONE. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5507497/
(34) de Sousa T, de Souza B, Zomkowisk K. (2016). The Effects of Acupuncture on Pain, Dyspareunia and Quality of Life in Brazilian Women with Endometriosis: A Randomised Clinical Trial. Complementary Therapies in Clinical Practice. Retrieved from
(35) Johansson J, Redman L, Veldhuis P et al. (2013). Acupuncture for Ovulation Induction in Polycystic Ovary Syndrome: A Randomised Controlled Trial. Am Journal Physiol Endocrinol Metabol. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4116535/
(36) Ye Y, ZHou C, Hu H et al. (2022). Underlying Mechanisms of Acupuncture Therapy on Polycystic Ovary Syndrome: Evidence from Animal and Clinical Studies. Front Endocrinol. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9637827/
(37) McClure L, Koppelman-Hopper M, Chimielicki B. The Acupuncture Evidence Project. An Overview of Scientific Evidence. Retrieved from https://www.evidencebasedacupuncture.org/acupuncture-scientific-evidence/
(38) Acupuncture New Zealand. (2021). The Acupuncture and Chinese Medicine Professionals.
(39) Chinese Medical Council of New Zealand. (2023). Safety in Chinese Medicine Clinical Practice, Guidance, Acupuncture and Associated Techniques. Retrieved from https://www.chinesemedicinecouncil.org.nz/common/Uploaded%20files/RegistrationsDocs/Standards%20Statement%20and%20Policies/Safety%20in%20Clinical%20Practice%20Guidance%2011Aug23.pdf
(40) Xu M, Yang C, Nian T et al. (2023). Adverse Effects Associated with Acupuncture Therapies: An Evidence Mapping from 535 Systematic Reviews. Chinese Medicine.
(41) Wu J, Hu Y, Zhu Y et al. (2015). Systematic Review of Adverse Effects: A Further step towards Modernization of Acupuncture in China. Evidence Based Complement Alternative Medicine. Retrieved from https://sci-hub.se/10.1155/2015/432467






