Molly Nguyen
BSc (Human Nutrition)
Prostate cancer is the second most common diagnosed cancer and the fifth leading cause of death in men around the world. Age, race, geographical location, family history and genetic mutations are among the most common risk factors associated with prostate cancer.
There is currently no conclusive evidence for prostate cancer prevention.
To understand the risk factors, signs and symptoms, screening and diagnosis of prostate cancer, lets first begin with understanding the function of the prostate.
What is Prostate?
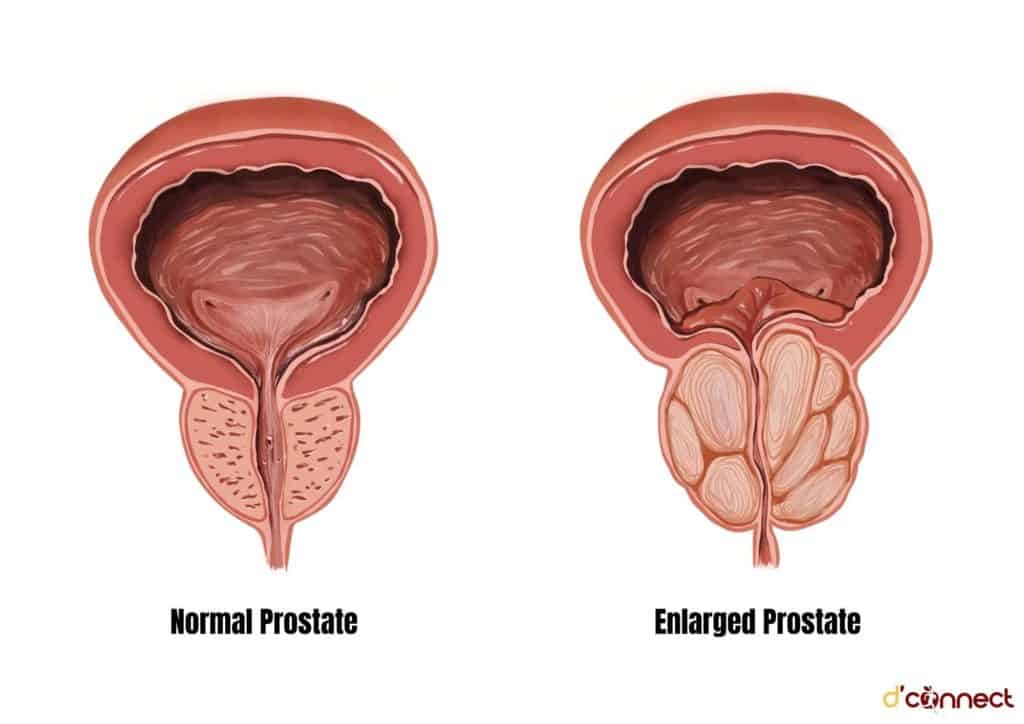
Prostate is a part of the male reproductive system that is located below the bladder (a collapsible muscular sac that stores and expels urine) and in front of the rectum (the last part of the large intestine).
It is a walnut-sized gland that wraps around the urethra, which is a tube that carries urine and semen out of the body through the penis. Prostate’s main function is to produce seminal fluid that contributes to sperm activation, viability, and motility.[1]
The size of the prostate can increase as men age. As the prostate enlarges, it squeezes the urethra and decreases urine flow, resulting in urinary retention.
Prostate is a walnut-sized gland that is found only in the male reproductive system
The enlargement of this gland is called benign prostatic hypertrophy (BPH) – a common condition of ageing men and has not been associated with prostate cancer.[1]
What is Prostate Cancer?
Prostate cancer begins when the healthy cells in the prostate gland start to divide and grow out of control resulting in abnormal prostate gland growth, forming a lump or a tumour.
Most prostate cancer cases (>95%) are adenocarcinoma, meaning that it originates from prostate glandular epithelial cells.[2]
Prostate cancer occurs when cells grow abnormally in the prostate gland
Unlike other types of cancer, many prostate cancer cells tend to grow very slowly and may not even cause any symptoms for years. In fact, most men with prostate cancer were not affected by the disease during their lives and died from other causes.
Prostate Cancer Statistics
Worldwide - how many men get prostate cancer
Prostate cancer is the second most frequently occurring cancer in men, behind only lung cancer, with approximately 1.4 million new cases in 2020 (Figure 1).[3]
Prostate cancer is also the 5th leading cause of cancer mortality (death) in males with 375,304 new deaths in 2020 (Figure 1). Globally, prostate cancer is the most commonly diagnosed cancer in 112 countries and the 2nd leading cause of cancer death in men in 48 countries.[3]
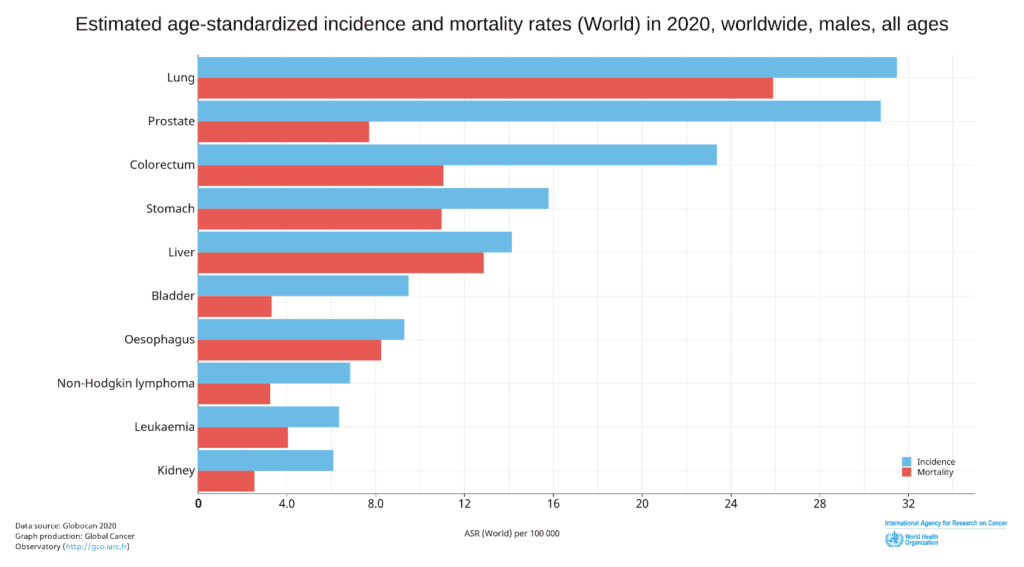
Figure 1. Incidence and Mortality Age-Standardised Rates for the Top 10 Most Common Cancers in 2020 for men worldwide. (Source: https://gco.iarc.fr/today/home)
Incidence rates of prostate cancer vary greatly across different regions (6.3 to 83.4 per 100,00 men), with higher rates found in Northern and Western Europe, followed by the Caribbean, Australia/New Zealand, and Northern America, and the lowest rates found in Asia and Northern Africa.[3]
Prostate cancer in New Zealand men
Prostate cancer is the most commonly diagnosed cancer and 3rd leading cause of death in men in New Zealand. There are approximately 3100 men diagnosed with and 650 men die from prostate cancer every year in New Zealand.
The incidence rate of prostate cancer in New Zealand is significantly higher than other types of cancers with 92.9 per 100,000 men in 2020 and the trend appears to be increasing (Figure 2).[3,4]
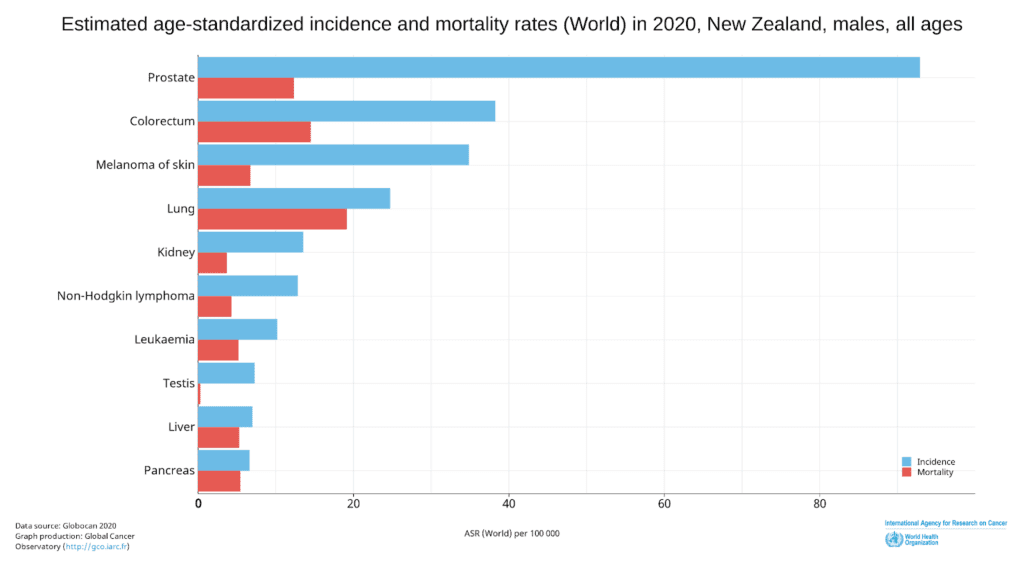
Figure 2. Incidence and Mortality Age-Standardised Rates for the Top 10 Most Common Cancers in 2020 for men in New Zealand. (Source: https://gco.iarc.fr/today/home)
What Causes Prostate Cancer (Risk Factors)
Although the cause of prostate cancer remains unclear, our current understanding of individual biological and lifestyle risk factors help to identify individuals at high risk and to reduce the burden of disease.
Some non-modifiable risk factors for prostate cancer established by researchers include:
Age
Ethnicity
There are significant differences in the incidence and mortality rate of prostate cancer across ethnic groups.
- African American men, Caribbean men of West African ancestry, and South American men are more likely to be diagnosed with prostate cancer than men of other ethnicities.[6]
- Black men are more than twice as likely to die from prostate cancer than other men.[7]
- Prostate cancer risks are lowest among Asian/Pacific Islanders and Hispanic men.[7]
The reasons for these disparities are still not fully understood.
Geographical location
Family history
Genetic factor is a well-established risk factor for prostate cancer in men. A family history of prostate cancer can influence the risk of prostate cancer in men.
Compared with men without affected family members, men with a first-degree relative (father or brother) diagnosed with prostate cancer have 2 to 3 times increased risk for prostate cancer. The risk also increases with the number of affected relatives.[7,9]
Hereditary prostate cancer, the inheritance of susceptibility genes of prostate cancer, maybe suspected if:
- More than one first-degree relative is diagnosed with prostate cancer
- Relatives with prostate cancer in 3 generations on the same side of the family
- 2 or more close relatives on the same side of the family were diagnosed with prostate cancer before age 55.
Mutated genes that are involved in the hereditary factors of familial prostate cancer include BRCA1 and BRCA2 genes (genes associated with increased risk for breast cancer and ovarian cancer), HPC1, HPC2, HPCX, PCaP, CAPB, and other mutated repair genes.[5,6]
RELATED — How common is Breast Cancer and what are the Risk Factors
Established risk factors of prostate cancer include advanced age, ethnicity, location, family history, and certain genetic mutations
Modifiable risk factors
These include dietary and lifestyle factors[10]:
- Greater body fatness (defined by BMI, waist circumference, and waist-to-hip ratio), such as being overweight or obese, increases the risk of advanced prostate cancer
- Developmental factors during childhood and adolescence that lead to greater linear growth (taller men) could increase the risk of prostate cancer
- Consumption of beta-carotene in supplements or foods is unlikely to have a substantial effect on the risk of prostate cancer
- Limited evidence suggests that diets high in dairy products or calcium increase the risk of developing prostate cancer
- Limited evidence suggests that low blood alpha-tocopherol (vitamin E) concentration or low blood selenium concentration increase the risk of prostate cancer.
However, the evidence is still unclear and inconsistent. Further research is needed to provide a better insight into the association between diet, nutrition, physical activity and prostate cancer.
The Signs and Symptoms to be aware of
The signs and symptoms of prostate cancer vary from man to man. Early prostate cancer usually has no symptoms, but can be detected through screening.
With more advanced prostate cancer, some symptoms may include:
- Weak or interrupted urine flow
- Difficulty to start or stop urine flow
- The need to urinate frequently, especially at night
- Blood in urine
- Pain or burning during urination
- Trouble getting an erection (erectile dysfunction)
- Pain in the back, hips, pelvis, shoulders, or other bones if cancer has spread outside of the prostate gland[5,10,11]
Keep in mind that these symptoms are not specific to prostate cancer and can be caused by other noncancerous (benign) conditions of the prostate, such as benign prostate hypertrophy (BPH).
Problem with urinating is a common symptom of prostate cancer
It is important to talk to your healthcare provider if you experience any of the symptoms to get the diagnosis and treatment if needed.
How to get checked and diagnosed
Screening and Early Detection
Most prostate cancer cases show no symptoms until the advanced stage. Therefore, screening helps to detect cancer early and provide a better chance of successfully treating prostate cancer in men. You should discuss with your doctor the possible risks and benefits of screening to make an informed decision.
Currently, there is no standard test for prostate cancer screening. Two commonly used screening tests for prostate cancer are:
- Prostate Specific Agent (PSA) Test: PSA is a protein produced by cells in the prostate gland. PSA test measures the PSA level in the blood, which is sometimes found to be elevated in men with prostate cancer. However, the PSA level can be affected by other factors and conditions.
- Digital rectal examination (DRE): The DRE involves a doctor inserting a gloved, lubricated finger into a man’s rectum to palpate the prostate gland through the wall of the rectum for any abnormality, such as enlarged prostate.[5,12]
Diagnosis
If the results from the screening tests (PSA and/or DRE) are abnormal, further tests are needed. The most common diagnostic tests for prostate cancer include biopsy, transrectal ultrasound (TRUS), and/or MRI fusion biopsy (a combination of an MRI scan and TRUS).[5,12]
Staging and Grading of Prostate Cancer
If diagnosed with prostate cancer, doctors will begin to conduct many tests to assess cancer’s location, whether cancer has spread, and whether it is affecting other parts of the body. This process is called staging and it helps doctors to find out the best treatment for you based on the extent (stage) of prostate cancer.
There are 2 types of staging used for prostate cancer:
- Clinical stage
This is determined by using PSA testing, DRE, Gleason score (via biopsy), CT, MRI scans and bone scans. - Pathologic stage
This is determined based on the information obtained during surgery and the pathology laboratory results.
There are 3 main components to staging prostate cancer:
- PSA level
The PSA testing, besides being used for screening, can also be useful for staging prostate cancer as well as to assess the effectiveness of the treatment by regular monitoring of PSA levels. - The grade of the tumour
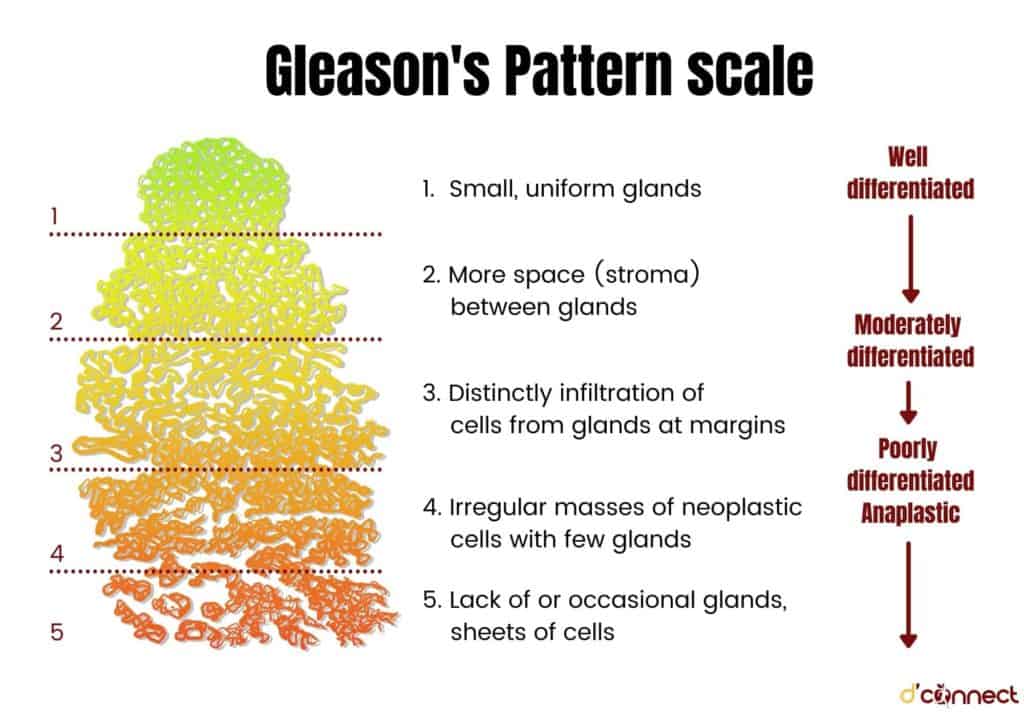
If prostate cancer is found via biopsy diagnostic test, it will be assigned a grade based on how abnormal cancer is viewed under a microscope. There are currently 2 grading systems in use for prostate cancer, which are the Gleason score and Grade Groups.[5,12,13]
The doctors will then plan and recommend the best treatment options based on stages and grades of prostate cancer.
Prostate Cancer Treatment (can it be cured)
Prostate cancer, if detected early, can have many possible curative treatments available. Advanced (metastatic) prostate cancer, however, is more difficult and unlikely to be cured.[5]
Treatment options for prostate cancer differ for each individual depending on the type and stage of cancer, individual cancer progression, possible side effects, personal lifestyles and preferences.[2,5,14]
Some current treatment options for prostate cancer are listed as follows:
Active monitoring
Because prostate cancer in an early stage grows very slowly, thus treatment may not be necessary. Instead, the doctor will recommend monitoring. If the symptoms or test results become worsening, treatment might be recommended.
Local treatments
Treatment that is directed to a specific, limited area of the body. It is a common choice to potentially cure prostate cancer if it has not spread to other parts of the body.
- Surgery
Surgical techniques involve the removal of the prostate gland and some surrounding tissues, including lymph nodes. - Radiation therapy
The use of high-energy radiation to control the growth or destroy prostate cancer cells.
Focal therapies
Less invasive treatment that destroys small prostate tumors while preserving the rest of the gland.
- Cryotherapy (cryosurgery)
The use of low (cold to freeze) temperature to freeze and remove prostate cancer.
Systemic treatments
The use of substances that circulate around the body and destroy cancer cells.
- Hormonal therapy. Used to lower male sex hormone (androgens) levels in the body to help slow the growth of prostate cancer cells.
- Chemotherapy. The use of drugs to destroy prostate cancer cells and are usually given orally (by mouth) or intravenously (into the veins).
- Immunotherapy (biological therapy). It is a type of treatment that uses and stimulates the immune system to fight cancer.
- Targeted therapy. The use of drugs to target cancer cells’ genes and proteins to prevent the cells from growing and dividing while doing little damage to healthy cells.
- Bone-modifying drugs. The use of bone-modifying agents to reduce bone complications (e.g. fractures or pain) from bone metastases (when cancer has spread to the bones).
Besides standard treatments, clinical trials are also considered as a treatment option. A clinical trial is a type of medical research study that involves testing the safety and effectiveness of new treatments. There are many prostate cancer clinical trials going on at the moment, including:
- investigating new drugs (e.g. Jevtana, Provenge, or Xgeva)
- new approaches for surgery
- different doses of radiotherapy
- different combination of treatment
- new treatment methods[5,13]
Even though prostate cancer is common, the treatment success rates of prostate cancer are high if prostate cancer is detected early and limited to the prostate gland.
Survival rates for localized or regional stages (prostate cancer found only in the prostate and nearby organs) are nearly 100%
Keep in mind that the estimated survival rate is only the percentage of people who survive cancer for a specific amount of time and it cannot predict how long a particular person will live after being diagnosed with cancer.
How to Prevent Prostate Cancer
Currently, there is no proven way to prevent prostate cancer. Many main risk factors of prostate cancer such as age, ethnicity, family history cannot be controlled or changed.
There are, however, some dietary suggestions, including nutrition and lifestyle changes that can reduce or delay the risk of developing prostate cancer.[2,6,7]
1. Maintain a healthy weight by eating a balanced diet and exercising regularly.
RELATED — Make exercise a part of your daily routine
2. Maintain healthy eating patterns that are high in vegetables, fruits, whole grains, and legumes (i.e. beans or peas).
RELATED — What is a plant-based diet: Vegan or Vegetarian?
3. Limit the amount of fat from red meat, highly processed foods, and dairy products.
RELATED — The Healthy Plate Model: Essentials of Healthy Eating
4. Incorporating some compounds such as soy, lycopene (carotenoid), tomato, green tea into the diet may be beneficial to lower the risk.
5. Avoid smoking and limit alcohol consumption.
6. Watch calcium intake from the diet and limit calcium supplements.
Related Questions
1. How often is prostate cancer misdiagnosed?
Prostate cancer can be misdiagnosed with benign prostate hypertrophy (BPH) due to both conditions presenting similar symptoms, although it is uncommon.
The effectiveness and advancement of many prostate cancer diagnostic tests provide more chances for cancer to be detected and diagnosed at an early stage.
2. Secondary cancer risk – Is prostate cancer linked with other types of cancers?
Survivors of prostate cancer can still develop a different type of cancer later in life (called secondary cancer).
Some secondary cancers that prostate cancer survivors are more likely to have include small intestine cancer, soft tissue cancer, thyroid cancer, thymus cancer, melanoma skin cancer. Common secondary cancers associated with radiotherapy treatment for prostate cancer are bladder cancer and rectum cancer.[15]
Disclaimer – D’Connect does not provide medical diagnosis, advice or treatment and any information published on our website, app and other D’Connect platforms is not intended as a substitute for medical advice. Before taking any action, please consult with your healthcare professional.
With a special interest in food and nutrition, Molly’s passion is to become a dietitian with expertise in nutrition and chronic diseases. Molly’s aim is to advocate the role that diets play in the prevention, treatment and reversal of non-communicable diseases that many are facing nowadays. By using the scientific evidence behind healthy eating, Molly’s focus is to help people follow a healthful and balanced diet to achieve their desired health outcomes.
References
(1) Patton KT, Thibodeau GA. Prostate Gland. Anatomy & physiology. USA: Elsevier Inc; 2018. p. 1053-4.
(2) Schatten H. Brief Overview of Prostate Cancer Statistics, Grading, Diagnosis and Treatment Strategies. Springer International Publishing; 2018. p. 1-14.
(3) Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-49.
(4) Prostate Cancer Foundation NZ. Prostate Cancer New Zealand: Prostate Cancer Foundation NZ; [cited 2021 Oct 20].
(5) Cancer.Net. Prostate Cancer: American Society of Clinical Oncology (ASCO); 2020 [cited 2021 Oct 20]. Available from: https://www.cancer.net/cancer-types/prostate-cancer.
(6) Perdana NR, Mochtar CA, Umbas R, Hamid AR. The Risk Factors of Prostate Cancer and Its Prevention: A Literature Review. Acta Med Indones. 2016;48(3):228-38.
(7) Pernar CH, Ebot EM, Wilson KM, Mucci LA. The Epidemiology of Prostate Cancer. Cold Spring Harb Perspect Med. 2018;8(12).
(8) American Cancer Society. Prostate Cancer: Cause, Risk Factors, and Prevention: American Cancer Society 2020 [cited 2021 Oct 20]. Available from: https://www.cancer.org/cancer/prostate-cancer/causes-risks-prevention.html.
(9) Patel AR, Klein EA. Risk factors for prostate cancer. Nat Clin Pract Urol. 2009;6(2):87-95.
(10) World Cancer Research Fund, American Institute for Cancer Research. Diet, nutrition, physical activity and prostate cancer 2018 [cited 2021 Oct 20]. Available from: http://dietandcancerreport.org/.
(11) Dunn MW, Kazer MW. Prostate cancer overview. Semin Oncol Nurs. 2011;27(4):241-50.
(12) American Cancer Society. Prostate Cancer: Early Detection, Diagnosis, and Staging: American Cancer Society 2020 [cited 2021 Oct 20]. Available from: https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging.html.
(13) Prostate Cancer Foundation. About Prostate Cancer 2021 [cited 2021 Oct 20]. Available from: https://www.pcf.org/about-prostate-cancer/.
(14) American Cancer Society. Prostate Cancer: Treatment: American Cancer Society 2020 [cited 2021 Oct 20]. Available from: https://www.cancer.org/cancer/prostate-cancer/treating.html.
(15) American Cancer Society. Prostate Cancer: Second Cancers After Prostate Cancer: American Cancer Society 2020 [cited 2021 Oct 20]. Available from: https://www.cancer.org/cancer/prostate-cancer/after-treatment/second-cancers.html.






