
Joyce Roberts
BHSc Nsg, Post Grad Cert Adv Nsg, Post Grad Dip Adv Nsg, Accredited Diabetes Nurse Specialist
Currently, type 1 diabetes is not curable or reversible. However, a person can still have a good quality of life with:
- Insulin therapy
- Planned meal choices and low-sugar foods
- Exercise
Also, daily glucose monitoring is important to make sure that the blood glucose doesn’t rise or fall sharply, which can cause additional complications.
Type 1 diabetes management
Type 1 diabetes places a significant burden of management on the individual with the condition.
The management of type 1 diabetes requires the tight collaboration of an interdisciplinary team which includes:
- diabetes educators and nurses
- diabetes doctors
- psychologists
- podiatrists
- dieticians
In addition to complex medication regimens, other behavioural modification is also needed, such as considerable knowledge and skill to navigate between hyperglycemia and hypoglycemia.[1] We talk about hypoglycemia later in the article.
Hyperglycemia
Hyperglycemia or high blood sugar occurs when glucose is trapped in the bloodstream due to a lack of insulin.
In New Zealand blood glucose levels in the 11–15 range are classified as high and requiring action.
Individual blood glucose ranges vary so it is important to talk with your diabetes team about your thresholds and targets.
The aim of diabetes care and management is to support people with type 1 diabetes to live a long and healthy life.
Components of management of individuals with type 1 diabetes include the following areas.
Insulin replacement therapy
The cornerstone of treatment for type 1 diabetes is insulin replacement therapy.
The discovery of insulin in 1921 has given individuals with type 1 diabetes a new lease on life, extending their lifespan dramatically.
The aims of insulin therapy are to:
- preserve life
- relieve the symptoms of hyperglycemia
- restore normal metabolism
- prevent diabetic ketoacidosis
Insulin is given subcutaneously with injection pens or pumps
Insulin is most commonly injected into the subcutaneous tissue of the abdomen. Other areas used are the upper arms, thighs or the buttocks. It is important that the same injection sites are not used day after day.

Source: FreePik
Insulin therapy is designed to most closely approximate the normal physiologic setting, in which the pancreas continuously secretes a small amount of insulin and produces larger amounts in response to a meal containing carbohydrate.[2]
Treatment also includes preventing long term complications by ensuring the person with type 1 diabetes is on other relevant medication such as cholesterol lowering treatment and antihypertensive medication as required.
Insulin pump therapy and technology has improved and has become more sophisticated and easier to use. An insulin pump delivers a pre-programmed amount of insulin at precise times.
Understanding the differences between injections and pumps is important when considering why and when pumps should be used instead of injections.
Glucose monitoring
Self-monitoring of blood glucose levels is fundamental to diabetes care.
Blood glucose meters became available to people with diabetes in the late 1970s.
It is highly recommended that the person with type 1 diabetes checks their blood sugars:
- before injecting fast acting insulin
- before their meals
- when they are feeling unwell
Frequent testing will ensure avoidance of hypoglycaemia and provide lifestyle flexibility when the results are used to assist the individual in their dietary choices, physical activity and insulin doses.

Source: FreePik
Another form of checking blood levels is continuous glucose monitoring.
This includes inserting a monitoring device in subcutaneous tissue, which then provides information about changes in glucose concentrations in real time.
Nutritional planning
Dietary advice plays a central role in the management of diabetes.
Healthy eating is essential in managing type 1 diabetes
It helps maintain the balance required between food, physical activity and insulin.
The three main nutrients in food are carbohydrate, protein and fat. A healthy balanced food plan will include all of these nutrients. Seeing a dietician for advice on tailoring a balanced food plan is strongly recommended.
RELATED — The Healthy Plate Model: Essentials of Healthy Eating
Avoidance of hypoglycemia and diabetic ketoacidosis
The goal of treatment in type 1 diabetes is to avoid the two acute complications of the disease, which are:
- diabetic ketoacidosis
- hypoglycemia
Hypoglycemia
Hypoglycemia is also known as low blood sugar.
Intensive management of type 1 diabetes increases the risk of hypoglycemia and acts as a major limiting step to achieving control.
In New Zealand a blood glucose level that is 4 and below is classified as a low level.
Some causes of low blood sugars are reduced food intake, too much insulin taken, inadequate preparation for physical activity and often the cause cannot be determined causing significant distress and frustration.
Hypoglycemia has three categories
- mild (self-recognised and treated)
- moderate (usually conscious and able to self-treat or with little help)
- severe (requiring emergency assistance and treatment)
Short term risks of hypoglycemia include potentially dangerous circumstances that may arise when someone is hypoglycemic while, for example, driving.
Long term risks of hypoglycemia include mild cognitive impairment. Hypoglycemic episodes predispose the individual to further episodes as a result of downgraded regulatory responses.
Diabetic Ketoacidosis
Diabetic Ketoacidosis or DKA is an acute complication of type 1 diabetes and can be potentially life-threatening.[3]
The basic cause of DKA is insufficient insulin effect due to either being sick or injured or taking less insulin than the body requires.
Our main source of energy is either glucose (from carbohydrates) or ketones (from fats). When there is not enough available glucose (due to insufficient insulin), ketones are released into the blood.
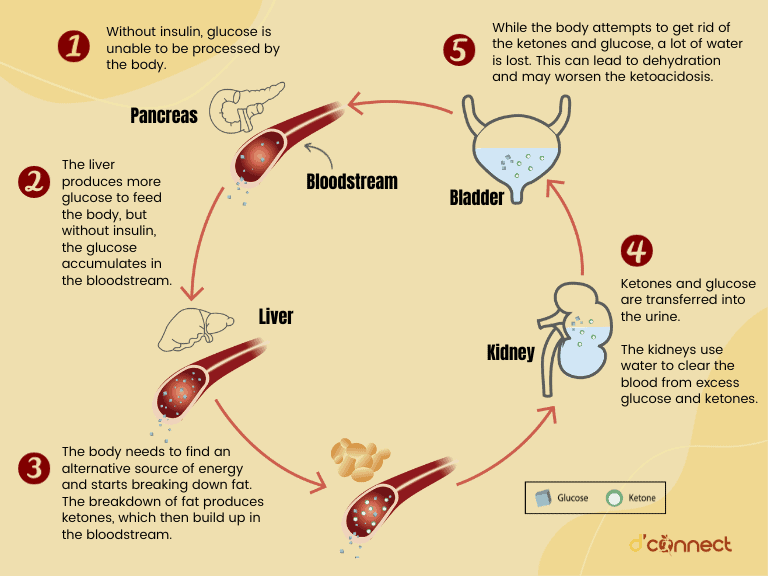
Regularly monitoring glucose levels by using the glucose monitor, and being educated on ketone testing is essential for preventing DKA developing.
Having a personalised sick day plan in place is also essential in helping with early recognition and treatment of DKA.
Screening for additional disorders
Associated autoimmune disease occurs with greater frequency in individuals who have type 1 diabetes.
Both thyroid dysfunction and coeliac disease occur more frequently and should be screened for every 1-2 years.
RELATED — Coeliac Disease: Symptoms and Effects on our health and body
Coeliac disease is more common in people with type 1 diabetes because both are autoimmune conditions and share a similar genetic profile. For most people type 1 diabetes is diagnosed before coeliac disease.
Coeliac disease is characterised by intolerance to gluten. The reaction to gluten damages the mucosal lining of the small intestine, flattening the villi and reducing the ability to absorb nutrients.[4]
It is important that the person who has developed coeliac disease consult with a dietician as the intolerance is permanent and requires complete and life-long exclusion of gluten from their diet.
RELATED — Coeliac Disease — Testing, Treatment and Diet
Both hypothyroidism and hyperthyroidism are seen to be at an increased incidence in the person with type 1 diabetes.
The person who has developed either hypothyroidism or hyperthyroidism may find it hard to manage their diabetes because the way their body uses glucose is altered.[4]
Ensuring regular screening for thyroid dysfunction enables early detection and treatment.
Mental Health
As type 1 diabetes is primarily a self-managed condition, subjective factors such as:
- burden borne by self-management
- effect of the disease on role and social functioning
are important to understand and take into consideration.[5]
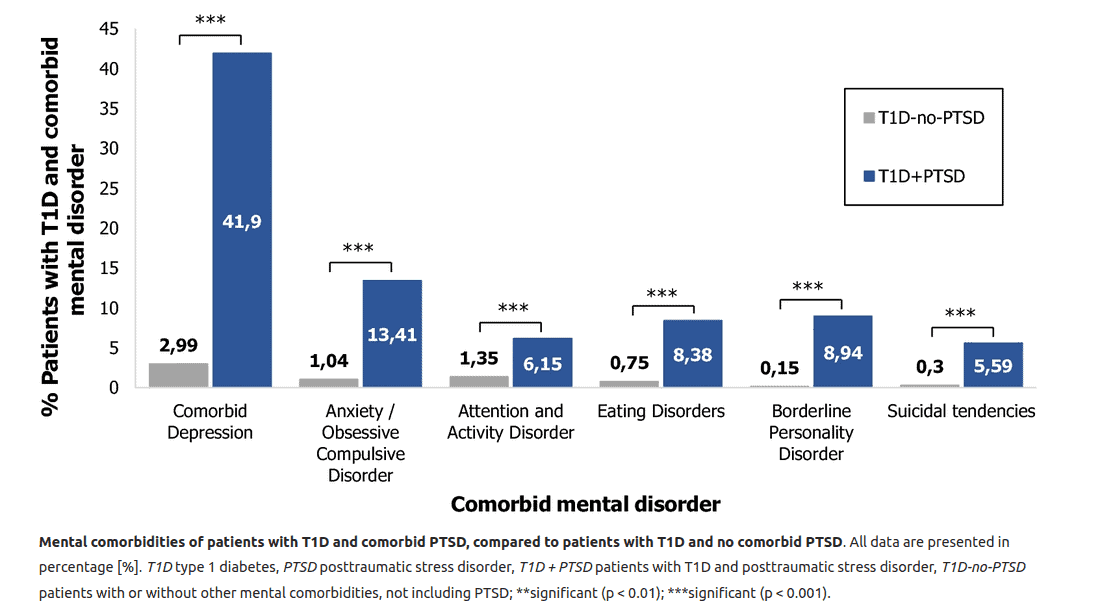
Source: Lunkenheimer, F. Posttraumatic stress disorder and diabetes-related outcomes in patients with type 1 diabetes. (2023).
The way individuals with type 1 diabetes think can affect how they feel and determine whether they will take health-promoting or illness-preventing actions.
Patient empowerment and autonomy are crucial for successful management.
The relentless physical and psychological demands of daily treatment, and the constant anxiety and fear of acute and long-term complications, have a major effect on physical, social and emotional well-being.[1]
It is crucial to normalise the psychological care that is an essential part of overall diabetes care.
Cardiovascular health
The person with type 1 diabetes is at an increased risk of developing cardiovascular complications.
Macrovascular diseases are more aggressive in type 1 diabetes
Reducing the risk of macrovascular diseases continues to be a major challenge.
RELATED — Diabetes Untreated (Part 2): Macrovascular diseases and health risks
Attention to a healthy lifestyle (weight control and physical activity), smoking cessation, with optimum glycemic blood pressure and cholesterol control reduces the risk of vascular disease developing.[1]
Macrovascular disease can be reduced or delayed by anti-hypertensive therapy, lipid-lowering therapy, and antiplatelet therapy.
Related Questions
1. How much insulin do type 1 diabetics need?
The insulin requirements of a person with type 1 diabetes is unique to the individual.
This depends on their day-to-day needs which takes into account their food, activity and information from their blood sugar results.
The person with type 1 diabetes utilises two types of insulin everyday, which are:
- long acting background insulin (taken once or twice a day)
- meal time insulin (taken at the time with every meal).
2. What foods should type 1 diabetics avoid?
The person who has developed type 1 diabetes is encouraged to learn about the carbohydrate foods as they have the biggest impact on blood glucose levels.
Learning to count carbohydrates provides an accurate and flexible approach to diabetes management.
3. What happens if type 1 diabetics eat too much sugar?
Indulging in too much sugar without enough insulin cover leads to hyperglycemia.
A one-off episode is not significant, but ongoing mismatching of carbohydrate foods plus not enough insulin leads to ongoing hyperglycemia with the risk of complications developing.
If you have been recently diagnosed with diabetes, and are looking for dishes that will keep your blood glucose in a healthy range, we suggest checking our Recipes page.
Joyce has been nursing since the 1980s, and for the past 20 years she has been focusing on patients with diabetes.
Given that diabetes can be a debilitating disease if not managed properly, Joyce’s focus is to ensure that individuals with diabetes have all the correct information. She works diligently and her focus is to prepare, inform and make sure that the individuals are well equipped with knowledge and support to live with the disease 24 hours a day.
References
(1) Katsarou, A, Gudbjornsdottir, S, et al. (2017). Type 1 diabetes mellitus. Nature reviews/Disease Primers.
(2) McDowell, Joan,Matthews, David,Brown, Florence. (2007) Diabetes: a handbook for the primary healthcare team.
(3) Fowler, M.(2009) Hyperglycemic Crisis in Adults:Pathophysiology, Presentations, Pitfalls, and Prevention. Clinical Diabetes. Retrieved from https://diabetesjournals.org/clinical/article/27/1/19/1796/Hyperglycemic-Crisis-in-Adults-Pathophysiology
(4) Holt, Richard, DeVries, J, et al.(2021). The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia.
(5) Danem, Denis. (2006). Type 1 diabetes. Lancet.






