
Joyce Roberts
BHSc Nsg, Post Grad Cert Adv Nsg, Post Grad Dip Adv Nsg, Accredited Diabetes Nurse Specialist
Note — The article was checked and updated May 2023.
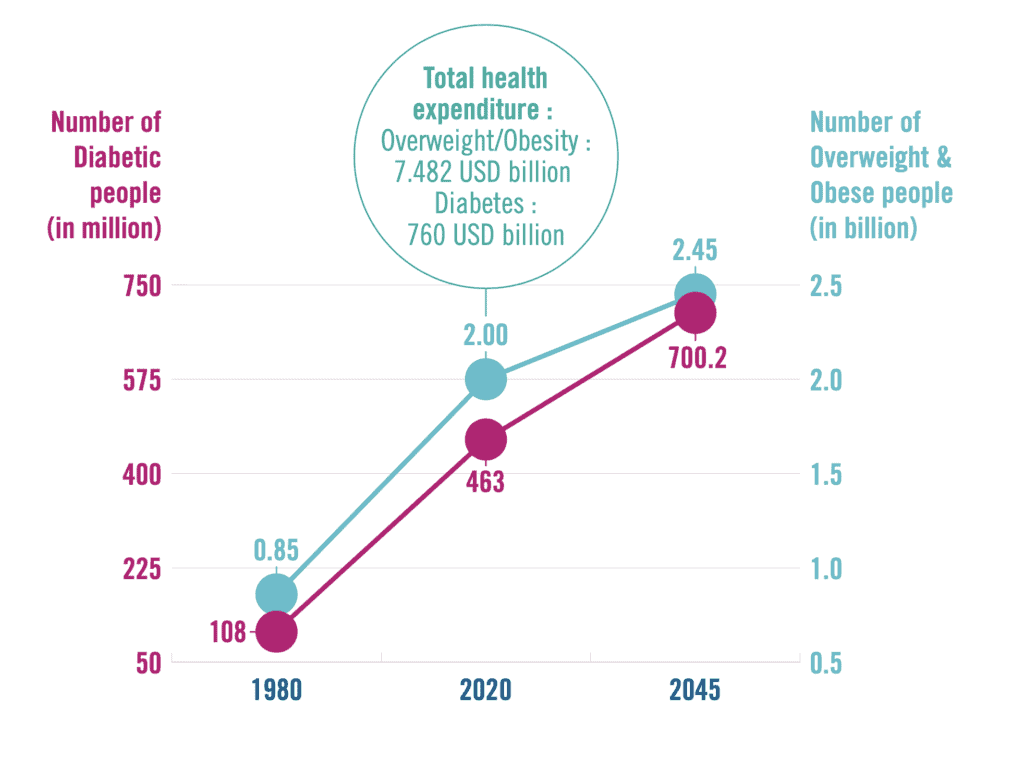
Today we have 537 million adults between 20-79 years of age who are living with diabetes worldwide. By 2045, that will increase to 700 million, which means that 1 out of 10 people will be dealing with diabetes.
Most of us think that there are only two types of diabetes – Type 1 and Type 2. However, today we know that diabetes can be split into conditions known as
- Prediabetes
- Type 1 diabetes
- Type 1.5 or Latent autoimmune diabetes in adults
- Type 2 diabetes
- Gestational diabetes
In this article we talk in more detail about these conditions, and also how we can prevent, manage and treat them in time before damage is done to the organs and the body.
What is Diabetes?
Diabetes mellitus is commonly referred to as Type 2 diabetes or diabetes which is a syndrome characterised by chronic hyperglycemia (high blood sugar) and other disturbances of carbohydrate, fats and protein metabolism.[1]
The first mention of diabetes dates back to 1500BC when the Egyptians noticed ants attracted to sweet urine.
Being diagnosed with diabetes is a life changing event
Diabetes is also classified as a chronic disease and occurs when our organ, the pancreas, is no longer able to make the necessary insulin required by our body, or our body is unable to utilise the insulin it has produced.
Diabetes also involves absent or ineffective utilisation of glucose which means the body loses access to it’s essential source of energy.
How common is diabetes?
Within the European region (2021 data) it was estimated that 61 million people were living with diabetes.[2]
This figure was produced from data collected within the last 5 years from 39 countries by the International Diabetes Federation.
The European region has the highest number of children and adolescents living with Type 1 diabetes
The Western Pacific region was found to have 206 million people living with diabetes in 2021. The Western Pacific region accounts for the 3rd highest prevalence of diabetes in the world.
The South Pacific region was estimated to have over 90 million people living with diabetes. The data collected for this region found that 25.9% of pregnancies were affected by hyperglycemia.[2]
In New Zealand over 250,000 people are living with diabetes, mostly Type 2.
This is about 5% of the population which according to the Ministry of Health is predicted to increase to 7% of the population by the year 2040.
About 5-10% of the population are living with Type 1 diabetes and this number is also growing.[3]
Type 2 diabetes is on the rise and is driven partly by our obesity problem
The International Diabetes Federation reported that in 2021, 537 million adults between 20-79 years of age are living with diabetes globally. In New Zealand Type 2 diabetes is more common in our Maori, Pacific and South Asian populations.
What Causes Diabetes?
The leading causes and most recognised risk factors for developing Type 2 diabetes are
- Age (over 40)
- Obesity
- Hypertension (high blood pressure)
- Physical inactivity
- Family history
There also appears to be an environmental-genetic interaction responsible for the development of Type 2 diabetes.[1]
The development of Type 2 diabetes often occurs in adulthood, usually after the ages 30-40, however, an increasing number of our teenagers and children are developing and being diagnosed with Type 2 diabetes.
In our modern day society one leading cause for developing Type 2 diabetes is being overweight. The extra weight we carry, especially if it is around our waist, sometimes causes insulin resistance which is commonly seen in people who have developed Type 2 diabetes.
In New Zealand the most likely groups at risk of developing Type 2 diabetes are those
- Aged over 40 and
- European
- Maori
- Asian
- Pacific Island, or Middle Eastern descent
- Aged over 30, with family history of
- Diabetes
- Hypertension
- Diagnosed with pre-diabetes
- Diagnosed with gestational diabetes
- Overweight
The exact cause of Type 1 diabetes has still not been fully established. It is much less common than Type 2 diabetes.
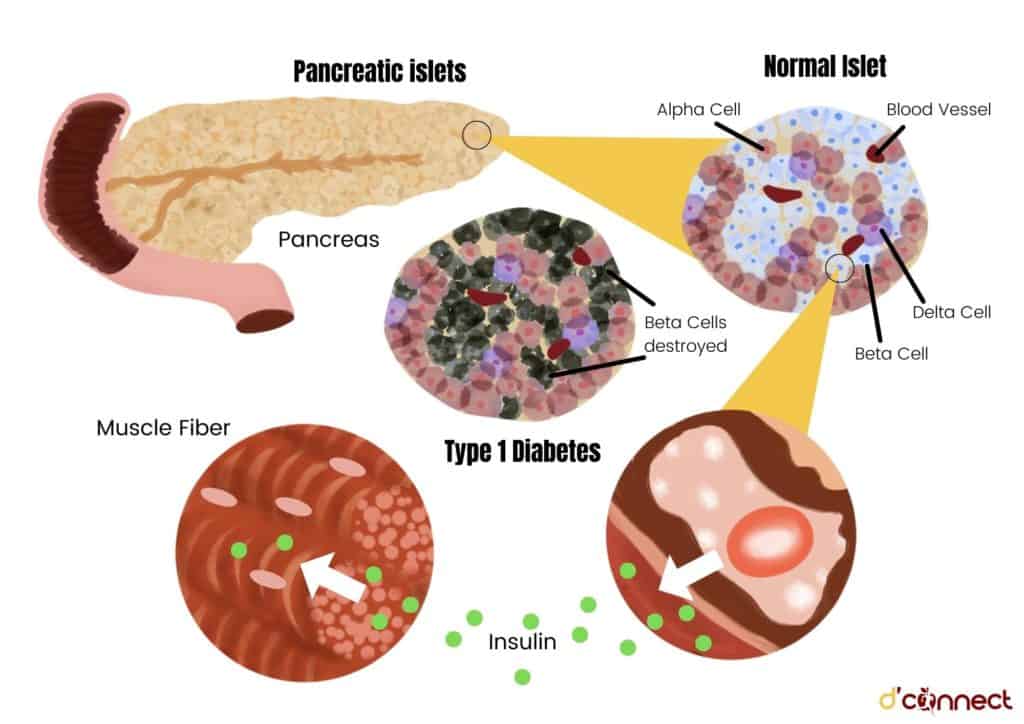
Type 1 diabetes is an auto-immune disease which occurs when our body’s immune system attacks and destroys the insulin producing beta cells of the pancreas.
Type 1 diabetes can occur at any age but is commonly seen in children and young adults.
It is suspected that it follows exposure to an environmental trigger such as an unidentified virus which stimulates an immune attack on our beta cells. Scientists believe there are some genetically predisposed people who are more susceptible than others for developing Type 1.
What are the early signs and symptoms of diabetes?
The signs and symptoms felt by the person who has developed Type 1 or Type 2 diabetes is mostly related to hyperglycemia (high blood glucose levels).
The 3 most commonly reported signs and symptoms are
- Polydipsia – a thirst we cannot quench.
- Polyuria – abnormally large amounts of urine which is diluted.
- Polyphagia – excessive eating or appetite.
It is not uncommon for the person who has developed Type 2 diabetes to report that they had no signs or symptoms.

Type 2 diabetes generally develops gradually while Type 1 diabetes develops more suddenly and over a shorter period of time.
The earlier signs of diabetes most reported by the newly diagnosed person include:
- Blurry vision
- Frequent urination
- Increased thirst
- Weight loss (mainly associated with Type 1 diabetes)
- Increased hunger
- Non-healing wounds
- Urinary tract infection and/or yeast infection (mostly woman)
Later signs of diabetes are
- Decreased sex drive
- Erectile dysfunction (men)
- Extreme fatigue
- Dry itchy skin
Blurry vision
Blurry vision is a common early sign and is what often takes a person off to see their doctor. The person’s vision returns to normal once treatment has started to reduce the high blood glucose levels.
Diabetes can affect both the small blood vessels in the eyes as well as the lenses
High blood sugar causes the lens inside the eye to swell while the small blood vessels, called the retina, are damaged over time by high blood glucose levels.
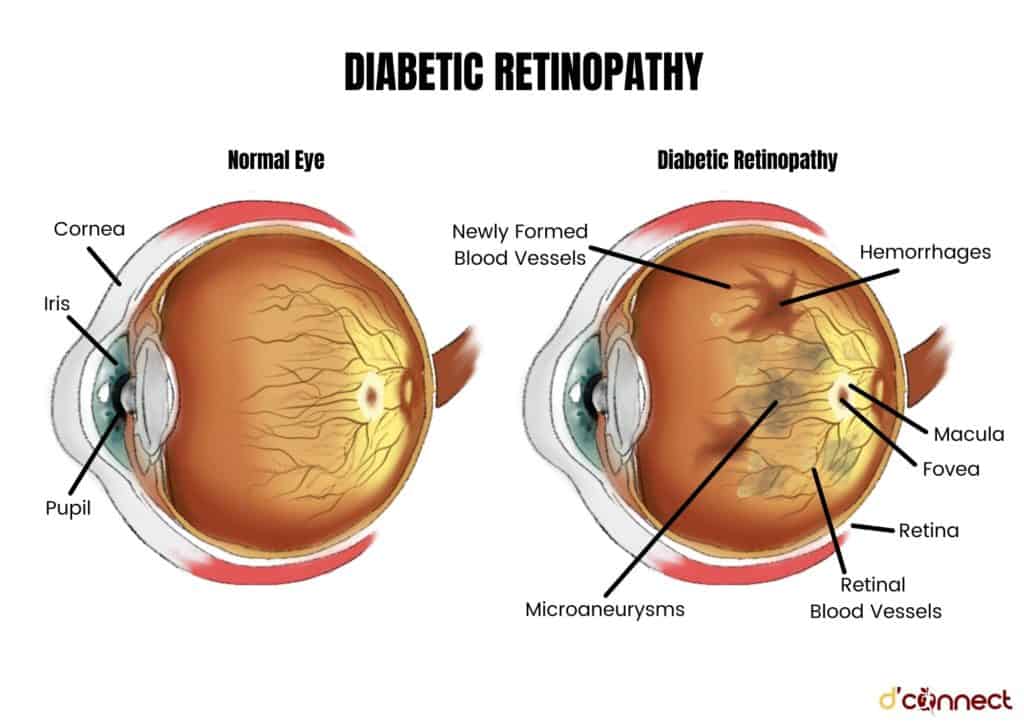
This damage is called diabetic retinopathy and it means that only some of the information about an image can be transmitted via the eye nerve from our retina to our brain.[4]
Frequent Urination
Polyuria is one of the most common symptoms of undiagnosed diabetes or a symptom of ongoing high blood glucose levels with a person who already has either Type 1 or Type 2 diabetes.
Our kidneys act as a natural filter removing excess glucose from our blood sending it to our bladder to excrete as urine. If our blood sugars are too high this forces our kidneys to work harder to remove the excess glucose, resulting in frequent urination.
Increased thirst
Polydipsia is another well known symptom of either undiagnosed diabetes or ongoing poorly treated hyperglycemia in a person with Type 1 or Type 2 diabetes.
Polydipsia is a feeling of extreme thirst
On a scientific level, excessive thirst is related to the fact that our brain is being told that we are thirsty due to the excessive amount of fluid being expelled by our kidneys. It is a vicious cycle and often the person is drinking excessive amounts of sugar laden drinks making the situation worse.
Weight loss
Excessive unintentional weight loss is mainly associated with a new diagnosis of Type 1 diabetes.
This excess weight loss occurs due to our body burning it’s fat and muscle stores as its energy source, which occurs mostly due to the effects of insulin deficiency.
Excessive hunger or increased appetite
Polyphagia happens when blood glucose levels remain abnormally high due to either being newly diagnosed with diabetes or ongoing poorly managed diabetes.
This means that the glucose from our bloodstream cannot enter our cells to be used as energy. In other words, our body has been unable to convert the food we eat into energy due to lack of insulin or insulin resistance.
The ongoing lack of energy drives the person’s hunger and leads to ongoing abnormally high blood glucose levels due to eating.
Non-healing wounds
Often a person who has been undiagnosed with diabetes presents to their doctor a wound that is taking a long time to heal.
Microorganisms in the wound are attracted to the elevated blood glucose levels
This then means the wound is slower to heal related to diabetes inhibiting the body’s capabilities of healing due to the hormones and enzymes that are produced by the body.
Elevated blood glucose levels also slow down the body’s circulation, leading to a slower delivery of essential nutrients that aid in wound healing.
Urinary tract infections
Presenting to the doctor with a urinary tract infection or complaining of thrush (candida) is a common presentation mainly in women.
Urinary tract infections develop due to frequent urination caused by elevated blood glucose levels. The high glucose levels acts as a favourable environment providing food for the pathogens and/or the yeast to grow and flourish.
Types of Diabetes
To better understand diabetes, we need to be aware of the different types as well as several less mentioned or known diabetes conditions.
Type 1 diabetes
Type 1 diabetes comes under the umbrella of auto-immune diseases where our body’s defence system attacks the cells that produce insulin – the beta cells.
RELATED — Type 1 Diabetes: Autoimmune disease that is on the rise
This then leads to the body producing very little or no insulin at all. It is mostly unknown why a person develops Type 1 diabetes but there appears to be some form of an environmental-genetic factor.
Person with Type 1 diabetes needs to take insulin everyday in order to survive
Type 2 diabetes
The most common form of diabetes in New Zealand is Type 2 diabetes, and unfortunately it is increasing in numbers.
In Type 2 diabetes either the cells in the body do not recognise the insulin that is present or the body is not producing enough insulin.
If Type 2 is diagnosed early enough the pancreas is usually producing enough insulin, but, for unknown reasons the body cannot use the insulin effectively. This is insulin resistance which is common in the newly diagnosed person with diabetes.
After a number of years insulin production declines resulting in glucose building up and the body unable to make efficient use of its main source of fuel – this is insulin deficiency.
Important to mention is that in some people Type 2 diabetes can be prevented.
Prediabetes
Impaired glucose tolerance or prediabetes develops as a result of our blood glucose levels being higher than normal but not in the diabetic range yet.
This is mainly related to the insulin that our body is producing as being inefficient.
The person who has developed prediabetes has the same risk of developing heart disease as the person who already has type 2 diabetes.
A change in lifestyle with a small weight loss, reduces our chance of going on to develop Type 2 diabetes.
Gestational diabetes
This type of diabetes can develop during pregnancy and is only temporary and usually disappears after giving birth. Women who have had gestational diabetes are at greater risk of developing Type 2 diabetes later in life.
Gestational diabetes is related to the high blood glucose levels that have developed during pregnancy related to the body’s increase in insulin requirements.
The 2 main reasons for the increase in requirements are related to the hormones produced by the placenta, making it difficult for insulin to do its job, and the increased need for insulin due to the growth demands of the developing baby.
Latent autoimmune diabetes (Type 1.5 diabetes)
LADA or latent autoimmune diabetes in adults is also known as Type 1.5. This is another form of diabetes diagnosed during adulthood.
Latent autoimmune diabetes can often be initially misdiagnosed as Type 2 diabetes as it shares some features of Type 2.
LADA is an autoimmune disease similar to Type 1 diabetes
In the early stages, the pancreas is still making enough insulin, confusing the situation, but within 3-5 years of diagnosis insulin will be required for survival, same as in Type 1 diabetes.
How to treat diabetes
Being on the right treatment pathway for the management of diabetes is crucial. We are all unique individuals and the same treatment might not work for everyone. If left untreated, or poorly treating and managing diabetes can have severe health complications.
RELATED — Diabetes untreated (Part 1): Microvascular diseases and health risks
A healthy lifestyle is always the first step followed by whatever recommended medication might be necessary.
The management plan should also include building a support team that includes a diabetes doctor, nurse, dietitian, podiatrist, and clinical health psychologist to name a few.
Type 1 diabetes treatment
For Type I diabetes insulin is crucial for survival.
Insulin is a naturally occurring hormone in our bodies which is deficient in people with Type 1, which is why they need to replace insulin everyday.

There are several types of insulin:
- Rapid acting
- Short acting
- Intermediate acting
- Mixed insulin*
- Long acting
On a day to day basis, the person with Type 1 diabetes will need to take a background insulin, also called long-acting insulin, once or twice a day, while rapid acting insulin is taken at meal times.
Some may find that using a mixed insulin, which is a combination of fast and long acting insulin, is easier to manage. In New Zealand, insulin is funded and readily available.
Insulin pumps are also an option for Type 1, either self-funded or through Pharmac if they meet the criteria.
Type 2 diabetes treatment
The first line treatment is always lifestyle management. Healthy eating, losing weight, if overweight, and encouraging physical activity are the mainstays.
Medication is added into the treatment plan as the disease progresses.
Healthy eating and Type 2 diabetes
I try not to use the word diet as it implies restrictions. Managing diabetes is about healthy eating, something we all should be doing.
The person who has developed Type 2 diabetes needs to be supported in making a healthy meal plan that is going to be sustainable for the rest of their life.
RELATED — The Healthy Plate Model: Essentials of Healthy Eating
In our current climate due to the vast choices of unhealthy foods readily available it is very difficult to keep making healthy food choices.
Gaining knowledge on how to eat well and make healthy food choices is key to living well and long with diabetes.
It is highly recommended that you meet with a registered dietitian and work out what a healthy meal plan might look like for you.
How exercise helps with Type 2 diabetes
Regular physical exercise is extra important for those who have developed diabetes.
The mantra of 30 minutes a day on most days is also recommended for people with diabetes.

Aerobic exercise is the most recommended form of exercising, such as a 30 minute walk with your dog, or a swim or having a dance class.
Regular exercise aids with keeping the blood sugars in control
Exercise also supports our mental health, aids with weight loss if needed and so much more.
If you have not been active for a while, it is recommended that you see your doctor first before undertaking an exercise programme.
Medications for Type 2 diabetes
Diabetes medications are grouped into how they help lower our blood glucose levels and support the rest of your body.
As the disease progresses, a person will need more medications to aid in maintaining good control. It is important to understand and gain knowledge on what medication you are taking to help support you with your journey in diabetes.
Alpha-glucosidase inhibitors belong to the group of drugs that prevent carbohydrate absorption. In New Zealand the drug used is called Acarbose but is not often provided due to its side effects that can cause significant gastrointestinal upset.
Biguanides belong to the group of medications that decrease peripheral insulin resistance and hepatic gluconeogenesis.
This drug is known as metformin and has been the long standing front line medication for diabetes for a long time. It is also popular due to its assistance with a mild loss in weight and cardiovascular protection.
DPP-IV inhibitors (Dipeptidyl peptidase-4) is the enzyme that is inhibited by the drug Vildagliptin, the only DPP-IV funded in New Zealand.
DPP-IV inhibitors increase insulin secretion which is glucose induced and decreases glucagon secretion.
Dulaglutide is a GLP-1 receptor agonist and is only funded in New Zealand under special authority criteria.
Dulaglutide is a subcutaneous injection taken once a week that acts on the GLP-1 receptor activating it to decrease gastric emptying, reducing appetite and glucagon secretion.
Glucose induced insulin secretion is also targeted by this drug and has been shown to have a significant impact on reducing blood sugars.
Meglitinides are oral medications similar to the sulfonylureas due to their action of encouraging insulin secretion. These medications are currently not available in New Zealand.
SGLT2 inhibitors are another new set of drugs available in New Zealand, also under special authority. This medication called Empagliflozin works by targeting the sodium glucose co-transporter 2 encouraging it to increase urinary excretion of glucose and sodium.
The drugs in the Sulfonylurea category have been available for a long time. In New Zealand the drugs called gliclazide and glipizide are the 2 most commonly used.
Sulfonylurea drugs help with increasing insulin secretion.
Once these medications have been started it is important for the person to be taught how to take their capillary blood sugar and also learn about hypoglycemia.
Pioglitazone is a member of the thiazolidinediones. Through its action of improving insulin sensitivity and reducing insulin resistance it allows any insulin the body may still be producing to work more effectively. It is still used in New Zealand but not widely.
Treatment for gestational diabetes
Women who have developed diabetes during their pregnancy are seen in specialist clinics. Some will need to start with taking insulin to help keep their blood sugars in control.
The targets for control of diabetes in pregnancy are much tighter in order to protect the mother and her baby. The pregnant mother is also supported by a diabetes dietitian in order to maximise diabetes control.
Related Questions
1. Can diabetes be cured?
There is no cure for Type 1 diabetes, but research is ongoing.
For Type 2 diabetes it is similar, but Type 2 diabetes can be placed into remission. Type 2 diabetes can be prevented for most people by ensuring a healthy lifestyle and being aware of our risks.
2. What is the main cause of diabetes?
With Type 1 diabetes it is still not known what the cause is. If you have family members with Type 1 diabetes, there is always a risk that you will develop it as well.
In Type 2 diabetes it appears that our current lifestyle of eating poorly and being less active plays a significant part towards developing the disease. There is also a risk if you have family members who have Type 2 diabetes.
3. What is the best diet for diabetes?
We must try and move away from the “dieting” mindset and accept a lifestyle perspective.
A healthy and balanced way of eating is recommended with help from a registered dietitian.
If you have any questions regarding diabetes, you can simply post them in the comments below, and we will reply.
Joyce has been nursing since the 1980s, and for the past 20 years she has been focusing on patients with diabetes.
Given that diabetes can be a debilitating disease if not managed properly, Joyce’s focus is to ensure that individuals with diabetes have all the correct information. She works diligently and her focus is to prepare, inform and make sure that the individuals are well equipped with knowledge and support to live with the disease 24 hours a day.
References
(1) McCance, K. L., Huether, S. E. Pathophysiology: The Biologic Basis for Disease in Adults and Children. (2012)
(2) Diabetes facts and figures. Retrieved from https://www.idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html
(3) Diabetes. Retrieved from https://www.health.govt.nz/
(4) Diabetic retinopathy. Retrieved from https://www.healthnavigator.org.nz/health-a-z/d/diabetic-retinopathy/






