
Megan Rodden
(BCS, DipNat, MedHerb, MNMHNZ)
Note — The article was checked and updated December 2023.
Fibromyalgia is a health condition that is defined as a musculoskeletal disorder. It is accompanied by pain, stiffness and tenderness, and it is not easy to diagnose.
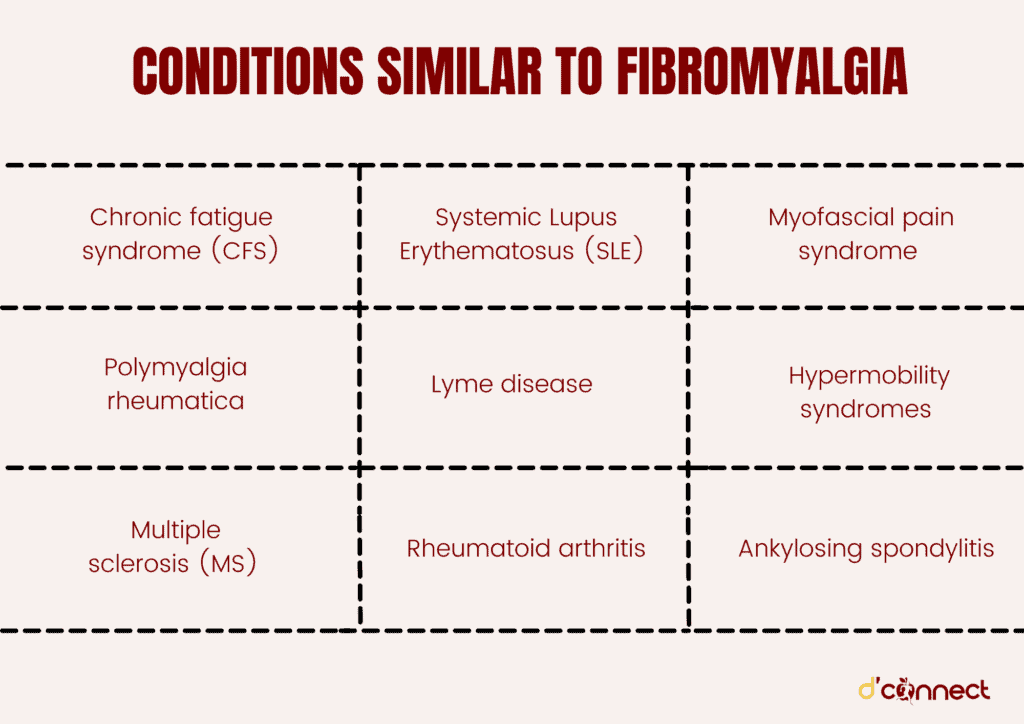
The reason why fibromyalgia diagnosis is difficult is due to fibromyalgia signs and symptoms being similar to almost a dozen other conditions, such as Ankylosing spondylitis, Systemic Lupus Erythematosus, Rheumatoid arthritis and others.
To understand the similarities between these conditions and fibromyalgia, we will look at different tests that assist in fibromyalgia diagnosis as well as some new fibromyalgia testing methods that are currently pending approval.
How is Fibromyalgia diagnosed (current and new testing)
Fibromyalgia is diagnosed by a family doctor or specialist using a set of criteria that includes signs and symptoms, such as widespread pain, fatigue and sleep problems.
This involves a process of physical examination and interviews where pain is measured and the body is checked for other potential causes, including through scans, xrays and blood tests.
Diagnosis is challenging because the symptoms of fibromyalgia mimic many other health conditions, therefore to avoid a misdiagnosis, a process of elimination is required that involves tests to rule out other conditions.
Widespread musculoskeletal pain is a key criteria, which means pain on both sides of the body and other symptoms must be chronic – experienced for at least three months.
A set of 18 tender points for pain across the body are also assessed but no longer required for diagnosis as these symptoms are now known to fluctuate.
New testing for Fibromyalgia
Recently, new research has identified a potential test capable of identifying a blood pattern for fibromyalgia that may help differentiate diagnosis from other similar conditions.
The test uses a technique measuring chemical bonds and energy of molecules in a blood sample and produces a pattern likened to a fingerprint.

The research has been led by Kevin Hackshaw, a professor and rheumatologist, in America, and has identified differences in the molecular patterns between fibromyalgia, lupus, osteoarthritis and rheumatoid arthritis.
Fibromyalgia may be better identified by differences in molecular patterns
The process is still being refined, however researchers aim to have the test ready within five years, for use in the process of diagnosing fibromyalgia.[1]
Conditions similar to Fibromyalgia (what are the similarities and differences?)
There are several conditions that are frequently misdiagnosed as fibromyalgia. The following conditions share common signs and symptoms with fibromyalgia, however with careful assessment they can be differentiated.
Chronic fatigue syndrome (CFS)
Also known as myalgic encephalomyelitis or ME this syndrome is a complex, controversial condition, often diagnosed together with Fibromyalgia.
CFS is marked by ongoing extreme tiredness and commonly triggered by an illness or trauma.
CFS and fibromyalgia are so similar that many experts believe they are interchangeable. Both conditions have symptoms of fatigue, painful joints or muscles and trouble with sleeping, anxiety and irritable bowel syndrome, however the key differences are CFS often includes symptoms of a viral infection such as a sore throat, swollen glands and fever.
Diagnosis also requires fatigue to persist for more than 6 months for CFS rather than 3 months for fibromyalgia.
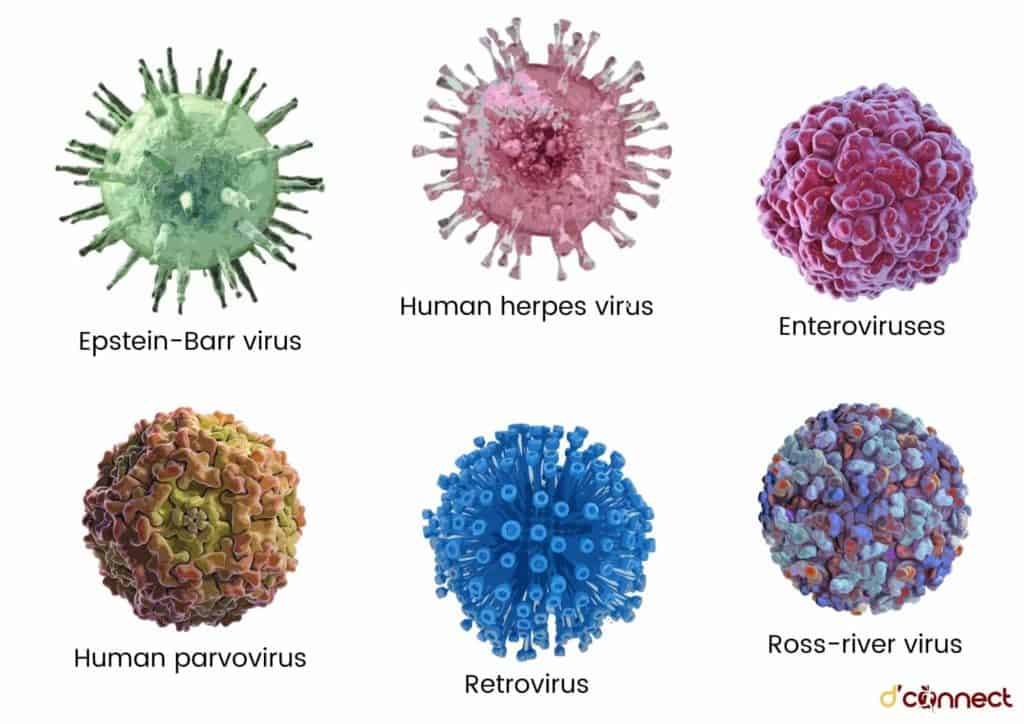
The most common illnesses associated with preceding the onset of CFS include:
- Epstein-Barr virus
- Human herpes virus
- Enteroviruses
- Human parvovirus
- Retrovirus
- Ross-river virus.[2]
Polymyalgia rheumatica
Polymyalgia rheumatica is a condition involving inflammation and the musculoskeletal system that affects more women than men and is connected to giant cell arteritis.
There are some similarities with fibromyalgia – the key symptom is pain in the muscles and joints and people may feel generally unwell and tired, however there are clear differences:
- stiffness (especially in the morning)
- mild fever
- unexplained weight loss
It also occurs more in those over 55 and blood tests show abnormalities such as increased ESR and C-reactive proteins.
Diagnosis is often made clear through excluding other conditions and the use of corticosteroids, which works quickly for polymyalgia to reduce symptoms.[3]
Polymyalgia rheumatica is more common in individuals over 55
Multiple sclerosis (MS)
Multiple sclerosis is a disease involving the central nervous system, which affects the nerve fibres and causes a range of symptoms.
RELATED — Let’s talk about Multiple Sclerosis
MS affects more women than men with symptoms appearing most often in those aged between 20 and 50 and tends to run in families. MS shares some common symptoms with fibromyalgia such as fatigue, chronic pain, difficulty thinking, and bowel symptoms.
MS symptoms may also fluctuate, known as relapses, however there are some significant differences including symptoms such as a loss of sensation, changes to sight, speech and swallowing and unlike fibromyalgia muscle pain is associated with involuntary spasms and weakness.
To diagnose MS, a brain and spinal cord scan is performed, which can identify MS plaques and differentiate it from other conditions.[4]
Systemic Lupus Erythematosus (SLE)
Lupus is an autoimmune condition that affects many systems in the body due to a problem with the function of the immune system.
Lupus affects more women than men, especially during child bearing years and tends to run in families. It is an inflammatory condition that is often diagnosed together with fibromyalgia and presents with similar symptoms that also may fluctuate including chronic muscle and joint pain and fatigue.
Lupus also has many other possible symptoms that are different to fibromyalgia:
- facial rash across the nose
- sensitivity to light
- headaches
- mild fevers
Diagnosis of lupus involves assessment of symptoms and medical history as well as blood tests. One blood test looks at a marker called antinuclear antibody, however it is not a unique test for lupus and other criteria are needed for a diagnosis.[5]
Lupus affects more women than men, especially during child bearing years
Lyme disease
Lyme disease is a bacterial infection that is carried by ticks. It is also known as borreliosis due to the name of the bacteria – borrelia.
The infection can cause a variety of symptoms and if left untreated it affects many parts of the body. Lyme disease is not common in New Zealand and only diagnosed in people who have recently travelled to regions such as Europe or America, where it naturally occurs.
There are some similarities with the symptoms of lyme disease and fibromyalgia, including fatigue and joint pain. However, there are key differences observed in the earlier stage of the infection – after the initial tick bite a rash appears called erythema migrans, followed by fever, chills and malaise.
Antibiotics are the main treatment and diagnosis may come from identifying a tick bite and the typical red, widening rash as well as blood tests and skin biopsies.[6]
Rheumatoid arthritis
Rheumatoid arthritis is an autoimmune condition that is inflammatory in nature and affects the entire body. It is found most often in women over 50 and involves a genetic predisposition as well as environmental triggers.
In RA the immune cells have an abnormal response causing swelling and damage in the joints. Musculoskeletal pain and fatigue are the pattern of symptoms that resemble fibromyalgia, however in rheumatoid arthritis joints are often swollen, stiff and warm due to the inflammation.
Diagnosis is made by assessing a set of criteria that includes observing symmetrical arthritis, x-ray results and blood tests, in particular – rheumatoid factor, anti-CCP, CRP, and ESR.[7]
In rheumatoid arthritis the immune cells have an abnormal response that causes swelling and damage in the joints
Myofascial pain syndrome
Myofascial pain and dysfunction syndrome is a condition that affects the muscles of the jaw, head and neck.
Although myofascial pain syndrome has symptoms of pain and fatigue it can be easily differentiated from fibromyalgia as the pain is not widespread and only affects the temporomandibular area. Diagnosis is made by evaluating symptoms and assessment of the mouth.
Hypermobility syndromes
Hypermobility syndromes are a group of conditions involving excess flexibility (ligament laxity) in the joints and many have strong genetic factors, for example Ehlers Danlos Syndrome is hereditary.
In hypermobility syndromes the joints are able to move outside of the normal range of motion and this may involve problems with different aspects of the structure of connective tissue affecting joint movement, such as collagen, elastin or fibrillin.
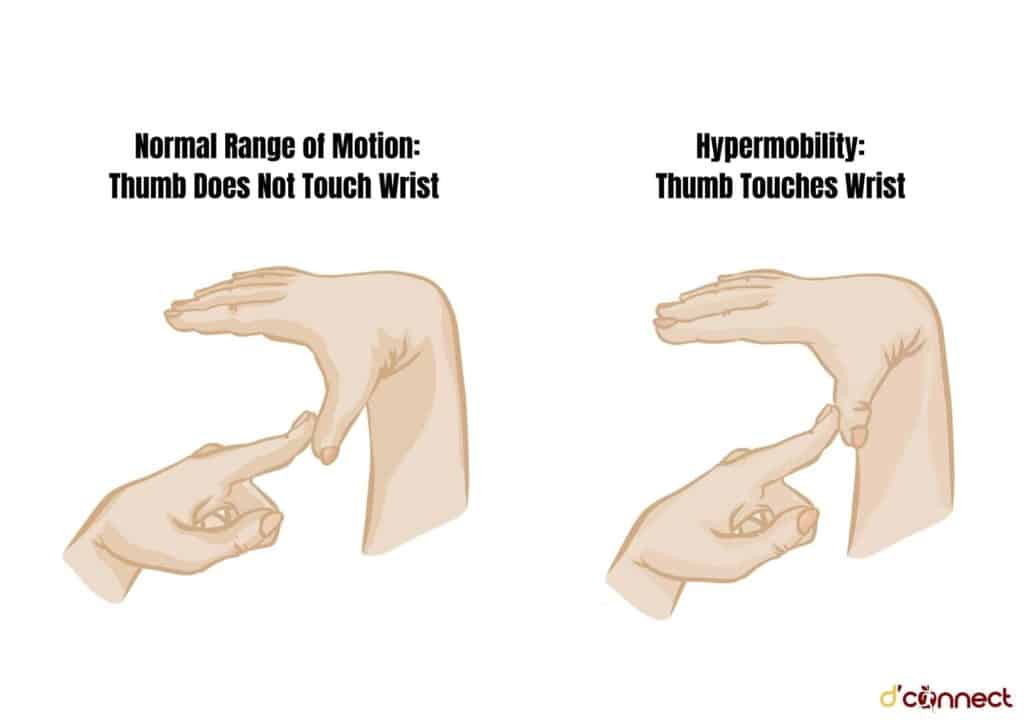
Each syndrome has different symptoms and some are similar to those of fibromyalgia. Studies have linked fibromyalgia with hypermobility syndromes and they are often diagnosed together.[8] More research is needed to understand this connection.
In hypermobility syndromes the joints are able to move outside of the normal range of motion
Diagnosis of hypermobility syndromes can be complex as there are no specific tests and involves experienced rheumatologists evaluating symptoms and family medical history. In some cases genetic tests are used and other assessments to rule out other conditions.
Ankylosing spondylitis
Also called Bechterew’s disease, is an inflammatory arthritic condition that affects more men than women and involves bones and joints, including the spine.
Symptoms may be similar to fibromyalgia, such as chronic pain throughout the body and fatigue, however ankylosing spondylitis is differentiated by pain being significantly in the back, especially at night, curving of the spine, morning stiffness (due to the arthritic nature) and in some cases eye abnormalities.
There are also early signs and symptoms such as mild fever, anorexia and weight loss. Ankylosing spondylitis commonly develops in ages 13-35 and is diagnosed through an x-ray.[9]
Fibromyalgia tests needed to rule out other conditions
There are several different tests that may be performed to help build an accurate assessment before a fibromyalgia diagnosis can be made. The following tests are commonly used as part of a process of elimination to rule out the presence of other diseases or conditions that may mimic fibromyalgia.
Complete blood count test looks at the number of blood cells – red and white, platelets and hemoglobin and is used to check for abnormalities that might indicate another diagnosis. For example, white blood cells increase when the body is fighting an infection.
Erythrocyte sedimentation rate (ESR) is used to rule out polymyalgia rheumatica as it measures levels of inflammation in the body. ESR looks at the way blood settles in a test tube and is a measurement of the speed of this. When outside of the normal range it can indicate chronic inflammation.
Cyclic citrullinated peptide (anti-CCP) test is used to help diagnose rheumatoid arthritis (RA) as it tests for levels of an antibody that is found in most cases of RA.
This antibody is one that the immune system makes and is associated with the autoimmune response of RA because it is known to accidentally attack healthy tissue.
Rheumatoid factor test helps diagnose rheumatoid arthritis as it also tests levels of an antibody and when found high in the blood it is associated with autoimmune conditions.
Rheumatoid factor is often found high in people with RA and used alongside other tests and information to diagnose RA, however can be present in other conditions and blood tests can be negative in people with RA.
Thyroid function tests measure levels of hormones produced by a gland called the thyroid. The hormones work in a feedback loop and interact with other tissues in the body and influence metabolism. A poor functioning thyroid can cause symptoms, such as fatigue.
Antinuclear antibody (ANA) is another test relating to the diagnosis of RA and detects the levels of an immune response cell in the blood that has the ability to attack healthy cells and cause inflammation in the body leading to symptoms like pain, swelling and fatigue. Large amounts of ANA in the blood can be a sign of an autoimmune condition like RA.
Coeliac serology may be done if Coeliac disease is suspected. The test measures levels of antibodies related to this condition. Coeliac disease is a gastrointestinal disorder involving an intolerance to gluten and can cause inflammation in the body that leads to symptoms similar to those seen in fibromyalgia.
RELATED — Coeliac Disease — Testing, Treatment and Diet
Vitamin D test measures fat soluble vitamins that have an important role in musculoskeletal health. People get vitamin D from their diet and exposure to sunlight.
RELATED — Vitamin D: The sunshine hormone for stronger bones
Also, if cofactors such as
are missing then deficiency may occur.
Deficiency symptoms are muscle pain and fatigue, and supplements may be used as treatment. Studies have been conflicting in connecting fibromyalgia and vitamin D levels, however it is an area of continued research.[10]
Need help?
If you are struggling with symptoms seek professional help, it is not recommended that you try to diagnose yourself. See a GP or request an appointment with a specialist, such as a rheumatologist.
Keep a diary of your symptoms and make a list of any questions that you have – this can be helpful for you and your doctor at your appointment.
What can a naturopath do?
Once you have been given a diagnosis, a naturopath may be able to support you in your journey to wellness by offering complementary natural treatments, such as herbal medicine, lifestyle techniques and holistic nutritional support.
RELATED – Visit our Nutrition page for great articles on healthy dieting and nutrition.
Disclaimer – D’Connect does not provide medical diagnosis, advice or treatment and any information published on our website, app and other D’Connect platforms is not intended as a substitute for medical advice. Before taking any action, please consult with your healthcare professional.
Megan is a qualified, registered naturopath and medical herbalist based in Laingholm, Auckland. She is also a trained journalist with a bachelor’s degree in communication studies and a mother of two, with a passion for plant medicine and holistic nutrition.
A personal health journey has directed Megan to develop a specific interest in digestive and respiratory health, allergies, autoimmune conditions and children’s wellness. You can find more about Megan and her practice at Megan Rodden – Naturopath.
References
(1) Hackshaw, K. Aykas, D.P. Sigurdson, G.T. et.al (2019) Metabolic fingerprinting for diagnosis of fibromyalgia and other rheumatologic disorders. Journal of Biological Chemistry, Volume 294, Issue 7
Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6378985/
(2) Rasa, S., Nora-Krukle, Z., Henning, N. et al. (2018) Chronic viral infections in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). J Transl Med. Retrieved from https://doi.org/10.1186/s12967-018-1644-y
(3) Villa-Forte, A. (2020) Polymyalgia Rheumatica. Merck Manual Professional Edition. www.merckmanuals.com
(4) Levin, M.C. (2021) Multiple Sclerosis (MS). Merck Manual Professional Edition. www.merckmanuals.com
(5) Lupus Foundation of America. (2021). How is lupus diagnosed: an overview. www.lupus.org
(6) Ngan, V. (2003). Lyme Disease. Dermnet New Zealand Trust. http://dermnetnz.org
(7) Craft, J., Gordon, C., Huether, S., McCance, K., Brashers, V., & Rote, N. (2015). Understanding Pathophysiology. Victoria: Mosby.
(8) Ofluoglu, D. Gunduz, OH. Kul-Panza, E. Guven, Z. (2006) Hypermobility in women with fibromyalgia syndrome. Clin Rheumatol. Retrieved from https://www.researchgate.net/publication/7537343_Hypermobility_in_women_with_fibromyalgia_syndrome
(9) Arthritis New Zealand. (2021). Ankylosing spondylitis. www.arthritis.org.nz
(10) Makrani, AH. Afshari, M. Ghajar, M. Forooghi, Z. Moosazadeh, M. (2017). Vitamin D and fibromyalgia: a meta-analysis. Korean J Pain. 2017 Oct;30(4):250-257. doi: 10.3344/kjp.2017.30.4.250. Epub 2017 Sep 29. PMID: 29123619; PMCID: PMC5665736.






