
Megan Rodden
(BCS, DipNat, MedHerb, MNMHNZ)
Are you waking up for months on end with exhausting body pain, headaches, brain fog, fatigue and gut problems, and are wondering what exactly is going on? The pain is continuous and you are hurting all over.
Fibromyalgia is a musculoskeletal disorder accompanied by pain, stiffness and tenderness. Though it’s not an autoimmune disease, it can be a long-term condition impacting our energy levels, mood, sleep and memory.
Fibromyalgia cannot be cured but it can be managed through a combination of stress reduction techniques, exercises and nutrition.
We talk about these in more detail below as well as recognizing signs and symptoms of fibromyalgia and how to prevent triggers and flares.
Fibromyalgia Explained - What is this syndrome?
Fibromyalgia is a disorder with a set of signs and symptoms involving the musculoskeletal system.
The cause of fibromyalgia is unknown, although it tends to run in families. There are many triggers associated with it and it is believed to involve problems with the nervous system and processing of sensations.
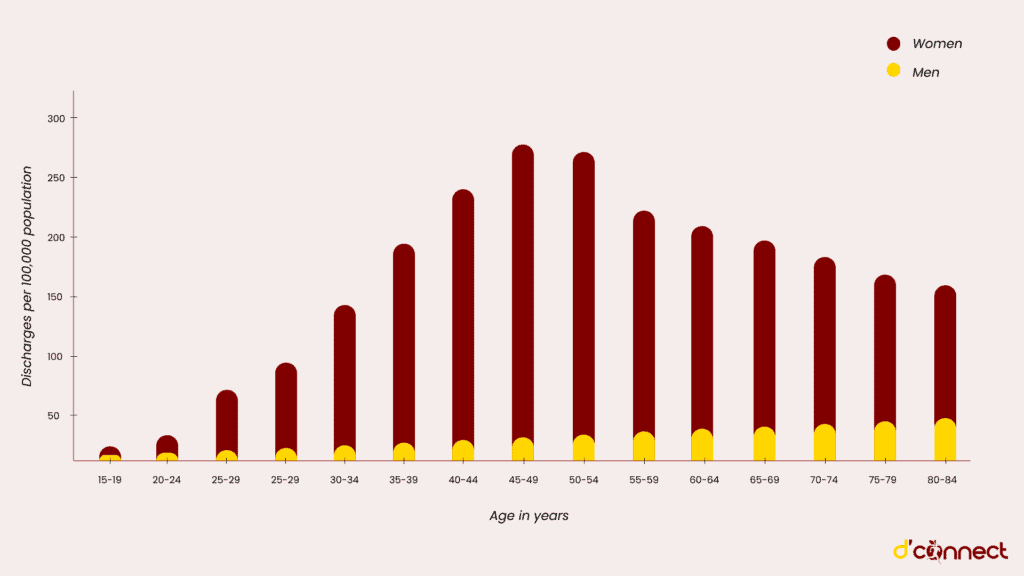
Fibromyalgia is a common condition affecting around 1 in 50 individuals in New Zealand, more frequently females as well as those with arthritic conditions.[1] We can see this in more detail in the chart below.
Fibromyalgia interferes with the nervous system and processing of sensory information
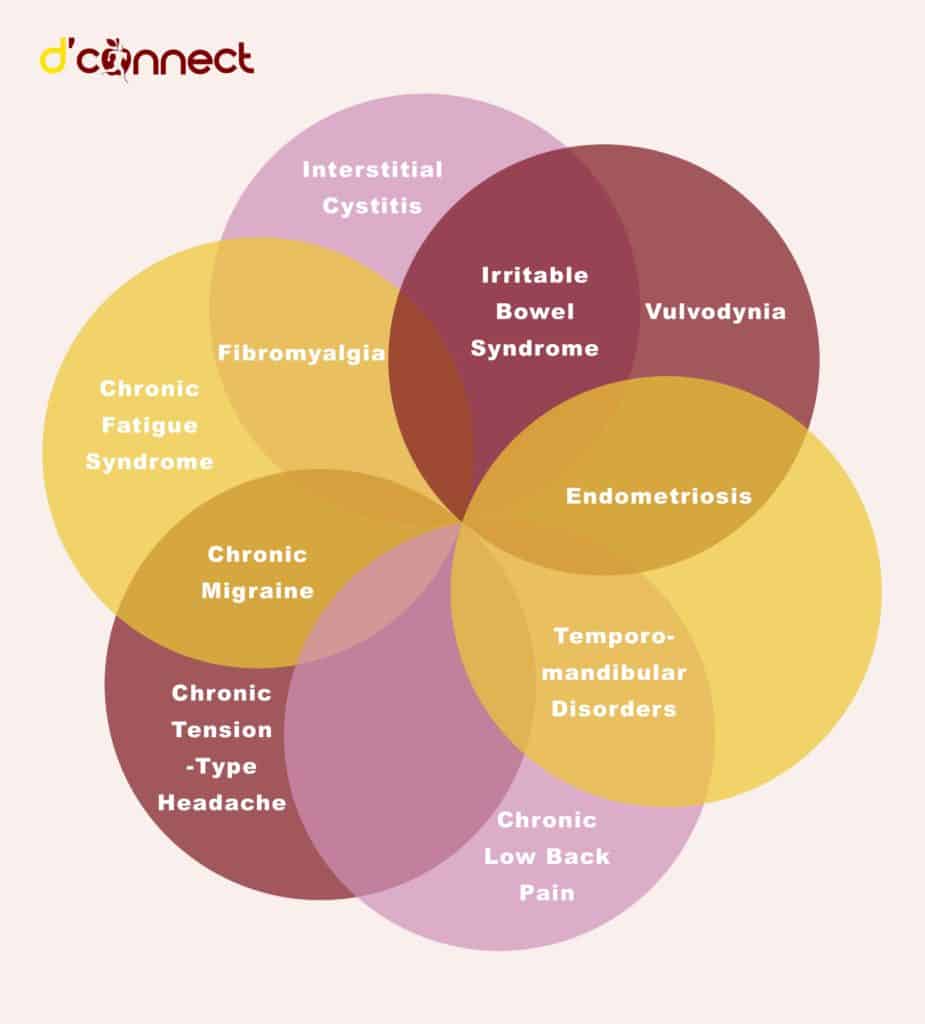
Fibromyalgia and Chronic Fatigue Syndrome (CFS) are conditions that are regularly diagnosed together and involve a set of similar symptoms; ongoing extreme tiredness and pain all over the body.
They are both complicated and difficult to diagnose because they mimic other illnesses in their symptoms.
RELATED — Fibromyalgia Misdiagnosis: Have I got Fibromyalgia or something else
People with these syndromes often also have symptoms of:
- Raynaud’s Phenomenon,
- Irritable bowel syndrome,
- Anxiety or
- Depression
RELATED — Introduction to: Depression
Although tenderness is involved, inflammation is not found in fibromyalgia.
The most common symptoms of fibromyalgia
Fibromyalgia involves a variety of symptoms that may affect many parts of the body with muscular pain being the most significant complaint. People may not experience all of these, however, the following are the most common symptoms of fibromyalgia:
- Pain and tender points through the body for more than three months. Aching and stiffness may be felt in at least three areas
- Fatigue may feel like constant, unshakeable tiredness, despite resting or involve an inability to recover from exercise. Fatigue may be debilitating and make daily tasks difficult.
- Trouble with sleeping, which often involves difficulty staying asleep. Feeling unrefreshed despite sleeping all night and feeling restless during sleep is also common.
RELATED — Different types of sleep: which one do we need the most?
- Digestive problems such as alternating constipation and diarrhoea.
- Cognitive dysfunction is often described as brain fog where thought processing feels slow and simple tasks require more concentration.[4]
Pain, fatigue and digestive problems are some of the most common symptoms of fibromyalgia
Fibromyalgia is a condition that affects individuals in many different ways and it is common for these symptoms to vary in intensity and be worsened by environmental changes like temperature, weather and exposure to toxins.
Fibromyalgia diagnosis
Initially symptoms may be assessed by a GP, who can run tests and navigate referrals but generally rheumatologists or internal medicine specialists use a set of criteria and tests to rule out other conditions.
Testing will depend on personal health history and may involve physical examination, laboratory tests and imaging.
Examples of common tests include:
- thyroid function
- diabetes blood tests
- full blood count
- CRP (looking at inflammation markers)
- lymph node palpation (to rule out pathology)
- liver and kidney function
- rheumatoid factor and antibodies (to rule out rheumatic disorders)
Naturopathic assessment may also include testing for food allergy/intolerances, heavy metals as well as adrenal hormone level, such as cortisol.
Fibromyalgia is considered difficult to diagnose and criteria have changed recently.
Fibromyalgia trigger points and flares
Fibromyalgia diagnosis previously involved identifying 18 tender points across the body. The trigger points include areas such as:
- hips
- shoulders
- knees
- chest
The pain in these areas tends to be ongoing, without redness or swelling. The clinical relevance of these pain points alone, in terms of diagnostic criteria, is still debated between health professionals, with more recently a focus on the syndrome as a whole, assessing five key areas:
- Pain
- Fatigue
- Unrefreshing sleep
- Cognitive symptoms
- Somatic symptoms[5]
Why do flares occur?
Fibromyalgia is known to have symptoms that fluctuate regularly, however, the cause of this is not completely understood.
It is theorized that neurotransmitters, the immune system and the HPA- axis (the system involved in regulating stress), are involved.[6]
Triggers connected with fibromyalgia involve internal and external stressors, such as infections or trauma, overworking the stress response and adrenal glands. This caused exhaustion and disordered hormone secretion such as cortisol, in response to further stress.
Fibromyalgia flares usually occur due to internal and external stress
Can Fibromyalgia be cured?
There is no known cure for fibromyalgia and allopathic treatments focus on symptom management, such as pain relief, antidepressant medication and lifestyle treatments. These include exercise and stress management.
It is common for fibromyalgia symptoms to have periods of both remission and flares with stress being a known trigger.[7]
Fibromyalgia Management
The treatment and management of fibromyalgia is multifaceted, targeting many systems in the body and may be very individualised because of the complex nature of the condition. People often seek the support of holistic complementary therapies as part of their treatment.
A holistic approach
Pain and tiredness are natural warning signals in the body telling us that something is out of balance, this may involve looking at all aspects of our health, including the mind, body and spirit. The development of fibromyalgia is believed to involve the brain, muscles, and stress response system.
Central changes in pain detection and response are also considered to be involved and often follow an invasive or environmental factor such as a viral infection, a stressful event, another syndrome or condition such as arthritis and HIV.[8]
Changing our diet, lifestyle and habits have been found supportive, using a holistic approach including the following techniques and therapies:
- Herbs prescribed by a naturopath may support and encourage healing processes in the body.
- Relaxation Massage prescribed by a qualified practitioner may assist managing pain.
- Reduce toxin exposure – a variety of toxins have been found to be involved in the development of chronic health conditions, including fibromyalgia.
- Exercise including yoga and tai chi have been found to help with symptom management.
- Nutrition and nutrient deficiencies are important to address and nutrients such as magnesium may be supportive.
RELATED — Nutrient of the month: Magnesium (for a great night of sleep)
Disclaimer – D’Connect does not provide medical diagnosis, advice or treatment and any information published on our website, app and other D’Connect platforms is not intended as a substitute for medical advice. Before taking any action, please consult with your healthcare professional.
Megan is a qualified, registered naturopath and medical herbalist based in Laingholm, Auckland. She is also a trained journalist with a bachelor’s degree in communication studies and a mother of two, with a passion for plant medicine and holistic nutrition…
If you would like to learn more about Megan, see Expert: Megan Rodden.
References
(1) Arthritis New Zealand. (2011). Fibromyalgia. Arthritis New Zealand: https://www.arthritis.org.nz
(2) Graham, W. (1953) The fibrositis syndrome. Bull Rheum Dis. Apr;3(8):33-4. PMID: 13032696.
(3) Smythe HA, Moldofsky H. (1997) Two contributions to the understanding of the “fibrositis” syndrome. Bull Rheum Dis.. PMID: 199304.
(4) Millea, P., & Holloway, R. (2000). Treating Fibromyalgia. 1;62(7):1575-1582. American Family Physician: https://www.aafp.org/afp/2000/1001/p1575.html
(5) Guymer, EK. Maruff, P. Littlejohn, GO. (2012) Clinical characteristics of 150 consecutive fibromyalgia patients attending an Australian public hospital clinic. International Journal of Rheumatic Diseases. Aug;15(4):348-357. DOI: 10.1111/j.1756-185x.2012.01767.x. PMID: 22898214.
(6) Wolfe, F. Clauw, DJ. Fitzcharles, MA. Goldenberg, DL. Katz, RS Mease, P. Russell, AS. Russell, IJ. Winfield, JB. Yunus, MB. (2010) The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken). May;62(5):600-10. doi: 10.1002/acr.20140. PMID: 20461783.
(7) Biundo, J. (2018). Fibromyalgia. Merck Manuals Professional version: https://www.msdmanuals.com
(8) Craft, J., Gordon, C., Huether, S., McCance, K., Brashers, V., & Rote, N. (2015). Understanding Pathophysiology. Victoria: Mosby.






