
Chris Veitch
PhD Physiology, BBiomedSc (Hons)
Jump to:
- Healthy blood pressure
- Cardiovascular health
- Diabetes
- The immune system
- Inflammation
- Recovery and cell regeneration
- Exercise performance
- Obesity
- Depression and anxiety
- Resilience
- Dementia
- Alertness, Productivity and Creativity
- Libido and fertility
- Skin health
- Memory and brain health
- Longevity
- Other sleep research
- Related Questions
Everyone knows that sleep is important in a healthy life, as we often direct someone who is feeling unwell to “get some rest”.
But what scientific evidence do we have of sleep benefits on the body? In this article we’ll talk in more detail about the importance of sleep on
- healthy blood pressure
- cardiovascular health
- immunity
- diabetes
- mental health
- longevity
and a few other important areas of health that you may not know are influenced and improved by having a healthy sleep schedule.
Healthy blood pressure
Maintaining a healthy blood pressure is essential for the proper functioning of the body. Hypertension (high blood pressure) is an increasingly common condition which is associated with poor heart health long term.
Recent research has shown that inconsistent sleep schedules are associated with increased risks of hypertension.[1,2] Along with this, having differing bedtimes each day puts people at higher chances of having hypertension.
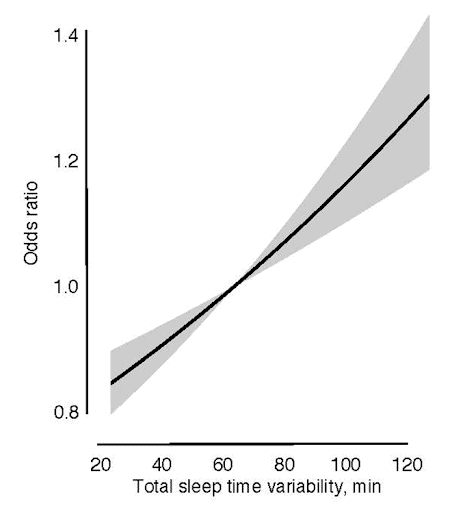
Increased prevalence of hypertension is also noted in individuals who sleep for short duration (<7 hours a night) compared to those who sleep the recommended 8 hours or more.[2]
Cardiovascular health
Coronary heart disease (a disease affecting the blood vessels supplying the heart) is thought to be linked to an imbalance in the body’s hormonal control systems, due to prolonged sleep deprivation.[3]
Individuals suffering from insomnia (a disorder impacting your ability to stay or fall asleep) have been shown to exhibit increased levels of stress hormones, suggesting the heart has been put into this state of stress from a lack of sleep.[4]
Individuals who slept 6 hours or less were also found to have a 23% higher risk of developing coronary heart disease, compared to individuals who slept 7-8 hours.
Sleep quality was also important in this relationship, as when researchers compared those with both poor quality and short duration sleep.
These individuals had a 79% higher risk of coronary heart disease compared to those with normal sleep duration and good quality sleep.[4]
The risk of diabetes
Diabetes is becoming a health concern around the world, with increasing amounts of the population being diagnosed with the disease each year.
While a diet is directly linked to a risk of having diabetes, so is short sleep duration, where having less than 6 hours of sleep per night is predictive of an increased risk of diabetes, along with obesity and hypertension which also increase diabetes risk.[5,6]
Sleeping less than 6 hours per night increases the risk of diabetes
One study in particular found that individuals who slept less than 5 hours were 2.06 times more likely to have diabetes compared to those who reported 7 hours of sleep.[5]
RELATED — Diabetes: Early Signs, Causes, Types and Treatment
Researchers suggest that the worse emotional state seen with sleep deprivation, such as
- irritability
- poor mood
- stress
may lower an individual’s drive to engage in healthy behaviours such as exercise and good nutrition, which would be contributing to diabetes risk.[6]
The immune system
One of the most common pieces of advice given to us when we get unwell or ill is to get some rest. Lab studies have supported this time-honoured piece of advice, with research showing that patients with reduced sleep quality or duration had an increased risk of infection of various diseases, including the common cold.[7]
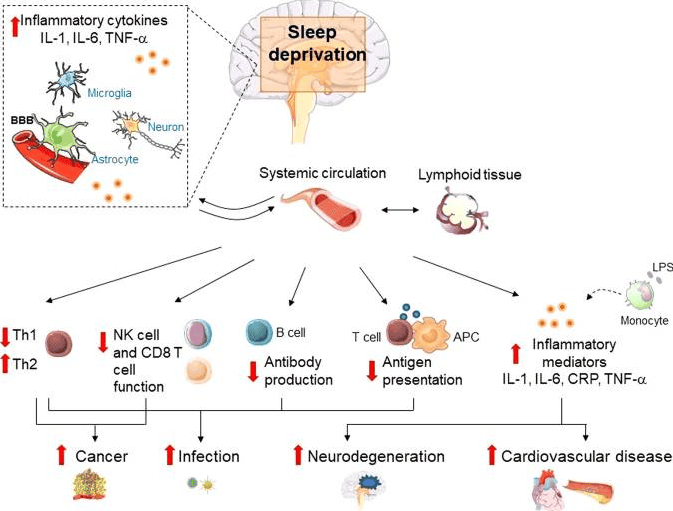
Furthermore, a reduced response to vaccination was also seen in human subjects suffering from sleep deprivation, reducing the effectiveness of the given vaccination.[7]
Sleep enhances immunological memory
That means that sleep is helping the immune system remember infection so it can fight it off more effectively in the future.[8]
Inflammation
Inflammation is the body’s natural way of fighting injury and infection, but this can cause negative long-term health effects when inflammation doesn’t naturally resolve, or occurs at inappropriate times.
This is known as chronic inflammation. Sleep loss in experimental settings has been shown to start inflammatory processes.[9]
Along with this, females specifically showed an association with sleep inconsistency (differing wake times, sleep times night by night) and inflammation, suggesting that females are at more risk from sleep-induced inflammation.[10]
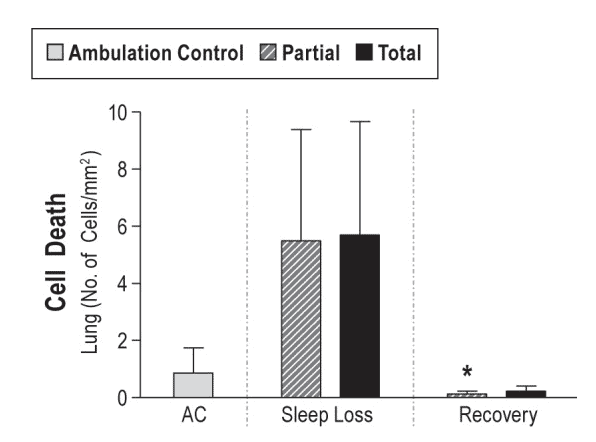
Recovery and cell regeneration
Poor sleep has even been associated with impacting the body’s ability to heal, leading to both cell damage and a decreased ability to repair cells in an animal mode.[11]
Sleep is also integral in maintaining muscle growth and reducing accumulation of fat, with short duration and poor quality sleep shown to increase fat accumulation in study participants.[12]
Along with this, even if sleep duration was maintained but sleep quality was poor, muscle growth was shown to be inhibited.[12]
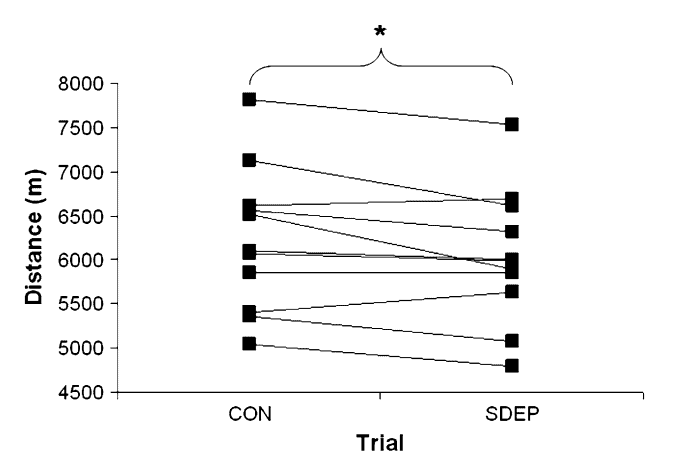
Exercise performance
Good sleep is also key to maintaining your best exercise performance. A 2009 study examining treadmill performance showed that demand on the body for the same duration of exercise was increased in those with sleep deprivation compared to those with a normal night’s sleep.[13]
Along with this, these participants experienced an increased perceived effort of exercise, further impacting running performance in the study.[12]
Similar findings have also been seen in cycling. Participants exhibited significantly worse cycling performance after just one night of sleep restriction.[14]
Obesity
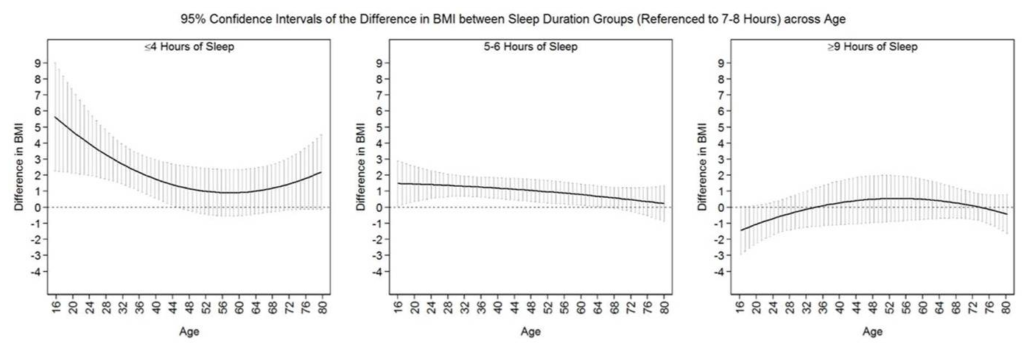
A longer sleep time is also associated with a lower body mass index (BMI), suggesting that longer sleep times are able to protect individuals from becoming overweight or obese.[15]
Interestingly, this association is not seen in older adults, which researchers suggest is due to factors such as sleep duration differing with older age.[15]
Research has also shown that sleeping for either less than 7 hours a night, or longer than 9 hours, is associated with an increased rate of being overweight or obese.[16]
Sleep deprivation is also linked to an increased risk of weight gain, as sleep deprivation impairs metabolism, as well as stimulating the feeling of hunger.[17]
Depression and anxiety
Depression and poor sleep are strongly related, with 40% of patients complaining of poor quality sleep.[18]
However, poor sleep has been noted as a risk factor for developing depression, with patients often reporting that poor sleep affected them before (40% of those studied) or at the same time (20% of those studied) as depressive symptoms.[18]
RELATED — Introduction to: Depression
Similar studies have looked at the risk of developing anxiety disorders as a result of poor sleep, with 18% of anxiety diagnoses exhibiting sleep disturbances prior to anxiety onset.[19]
Studies have also shown that people who report poor sleep have an increased chance of developing either anxiety or depressive disorders.[20]
Resilience
Sleep has also proven to be a beneficial way to deal with stress and increase resilience. Resilience has been noted in the medical field as a protective factor for many conditions/diseases, along with helping deal with everyday stresses.
Studies have identified a positive link between resilience and healthy sleep habits in various groups worldwide. A 2022 meta-analysis of 63 studies identified a significant, positive relationship with both sleep quality, duration and resilience.[21]
Not only does sleep quality help with everyday stress, but also helps with reducing the appearance of post-traumatic stress disorder (PTSD) in a study of healthcare workers during the COVID-19 pandemic.[22]
RELATED — Understanding Stress: The Silent Killer
Dementia
Having a good night’s sleep may also protect against Alzheimer’s disease and cognitive decline.
One of the key markers in the brain associated with Alzheimer’s disease (ß-amyloid) was noted to be significantly increased after one night of sleep deprivation in 20 healthy individuals.[23]
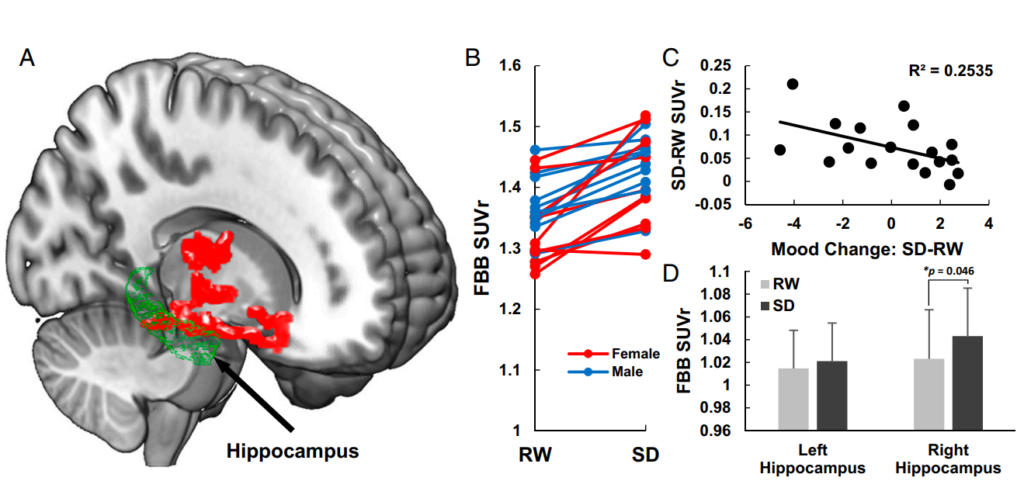
(C) Association between changes in mood from RW to SD. Mood change accounted for 35.5% of the variance. Self-report measures of alert, friendly, happy, social, and energetic significantly decreased, and measures of tired and difficulty staying awake significantly increased from RW to SD.
(D) A significant increase in ß-amyloid measured with FBB SUVr was seen in the right hippocampus only, in individuals with Sleep Deprivation (SD) compared to Rested-Wakefulness (RW).
Further studies suggest that a reduction of deep sleep may prevent the brain from clearing out a buildup of B-amyloid, leading to increased risk of cognitive decline, dementia and Alzheimer’s disease.[24]
RELATED — Introduction to: Brain Health
Alertness, Productivity and Creativity
Creatives may also benefit from a short nap to stir new ideas within the brain. In a 2023 study, individuals in light (N1) sleep were woken and asked to perform a series of tasks which were graded on creativity.
Compared to those who stayed awake, those who had a light sleep scored higher on the creative tasks.[25]
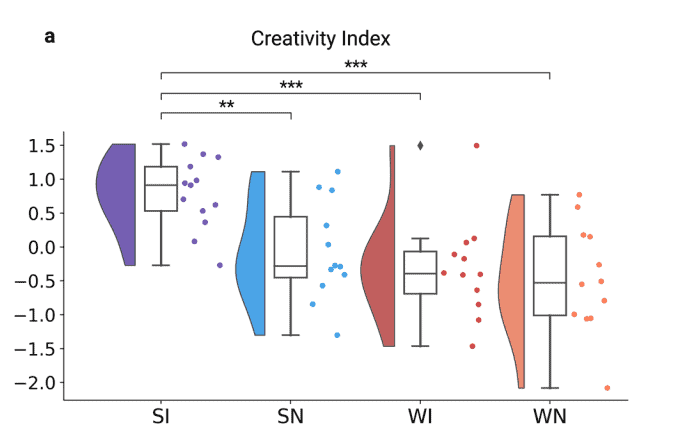
N1 sleep appears to be a “creative sweet spot”, with researchers showing that individuals who were woken immediately after entering N1 sleep had a significantly higher rate of discovering creative ways to finish a set task.[26]
RELATED — Different types of sleep: Which one do we need the most?
It probably comes at no surprise that shift workers suffer worse performance than those on day shift, but interestingly research has found that even though shift workers self-report that they feel more adjusted on the second night of night-shift, they still have similar performance impairment to the first night.[27]
Libido and fertility
Healthy sleep habits may have its benefits in the bedroom in more ways than one. Extended sleep duration by 1 hour from the group average of 7 hours and 22 minutes increased the studied individuals’ rated sexual desire the next day.[28]
Along with this, in studied individuals with sexual partners, an increased sleep duration by 1 hour corresponded to a 14% increase in the likelihood of engaging in partnered sexual activity the next day.[28]
However, sleeping longer than this (8 hours and 22 minutes) was associated with a decrease in sexual desire. In saying that, individuals who had a longer sleep time on average reported greater arousal than those with shorter average sleep.[28]
More than 7.5 hours of sleep increases libido
While the exact mechanism is unknown, researchers have also identified poorer fertility in women with worse quality sleep, such as shift workers.[29]
Researchers suggest that alterations in the sleep wake cycle have impacts on the hormones responsible for fertility, leading to impaired fertility in those with lower quality sleep.[29]
Skin health
Beauty sleep isn’t just a way to feel better, it’s researched to have measurable impacts on our skin health. A 2015 study showed that poor sleep had significant negative impacts on skin health, using a number of skin ageing metrics including
- wrinkles
- scars
- freckles
- uneven pigmentation[30]
Subjects that were classified as chronically poor sleepers exhibited significantly increased levels of uneven skin pigmentation, wrinkles, skin laxity and benign growths compared to good sleepers.[30]
Furthermore, these studied individuals rated themselves as more attractive after a good night’s sleep.[30]
Not only does poor sleep affect skin ageing, but it also has impacts on skin health and our natural skin microbiome.
Late bedtime (after 11pm) was associated with worse skin health, and a reduction in health of the skin microbiome, which is key for skin to stay healthy and functional.[31]
Memory and brain health
Memory consolidation is a process in which the brain strengthens memories, making it less likely for memories to be lost over time. Sleep is essential for this process, and enables us to remember learned processes for years to come.
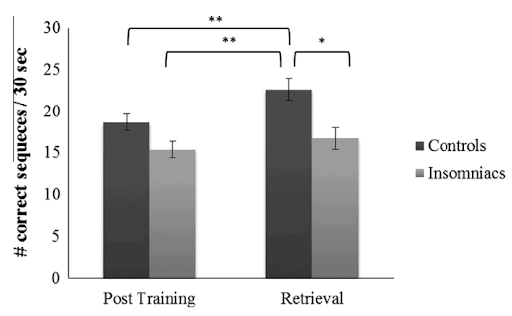
Research has shown that individuals with disrupted sleep patterns have impaired memory consolidation, which could lead to impaired cognition and memory in the long term.[32]
Individuals suffering from insomnia performing a memory test exhibited significantly worse performance compared to a control group, as shown below.[32]
Even aside from disrupted sleep patterns, getting proper sleep has been shown to improve learning of a task. Studied individuals were taught a task, then following either 8 hours of wakefulness, sleep, or a 90 minute nap, performed the task again.
Individuals who napped or slept performed better in the task than those who stayed awake.[33]
Longevity
Aside from the specific ailments and illnesses listed above that sleep protects against, it is overall associated with a longer lifespan and healthspan (duration of life without a significant medical condition).
RELATED — The Blue Zones: Learn the Secrets of Living Longer and Being Healthier
Both short sleep duration (<6 hours per night) and long sleep duration (>9 hours per night) were associated with significantly higher rates of death, in individuals who consistently sleep for this length of time.[34]
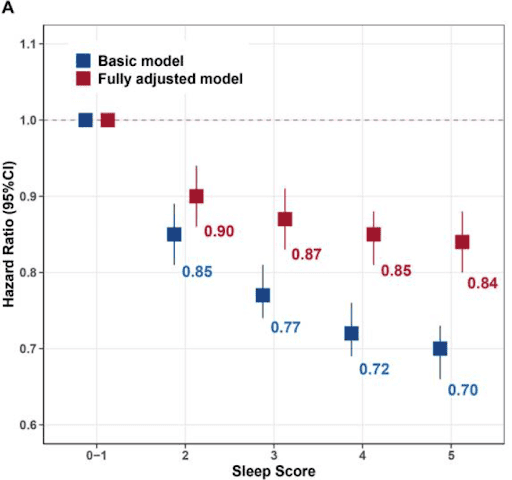
Another study showed that individuals with poor quality sleep (short duration, feeling tired often) were significantly more likely to have a shorter healthspan.[35]
This means these individuals had fewer years of their life living without a significant medical condition.
Other sleep research
Sleep research is an ever-evolving topic, with new discoveries being made frequently in the field. This section will explore some new and intriguing studies surrounding sleep science.
A 2023 study showed that after either partial sleep deprivation (sleeping <7 hours a night) or total sleep deprivation (staying awake all night), individuals who engaged in moderate intensity exercise performed better in tasks testing a broad range of brain function, such as reaction time, maths problems and logic puzzles, than individuals who did not exercise.[36]
The researchers suggest that engaging in moderate intensity exercise may be able to lessen the effects of partial sleep deprivation on brain function.
Subjects also reported feeling less sleepy on a subjective scale following exercise in either partial or total sleep deprivation conditions.[36]
Screen time around bed is an increasingly frequent issue, with the use of smartphones becoming widespread. Researchers from the University of Copenhagen reported that individuals who use smartphones frequently before bed were more likely to report having poor health.[37]
In a survey of over 3,500 young adults, females were more likely to report poor quality sleep compared to males.[38]
This association was noted to be independent of other factors such as depression and lifestyle factors, suggesting that women suffer a greater burden of sleep disturbance than men.
Related Questions
1. Which hormone is responsible for sleeping?
Melatonin is the main hormone responsible for sleep, which starts getting produced as the sun goes down.
This causes a gradual increase in sleepiness.[39]
2. What happens to my blood sugar levels while I’m asleep?
Blood sugar levels naturally increase during sleep. These increased sugar levels are handled by the hormone insulin, which allows cells to absorb sugar.[39]
3. Why can’t diabetics sleep properly?
In diabetes, insulin’s ability to work is impaired. This can lead to either too high or too low blood sugar during sleep, leading to insomnia and increased need to urinate.[41]
Chris is currently working as a clinical physiologist, specialising in sleep medicine. He is also currently studying towards his Postgraduate Diploma in Medical Technology endorsed in sleep medicine…
If you would like to learn more about Chris, see Expert: Chris Veitch.
References
(1) Scott, H., Lechat, B., Guyett, A., Reynolds, A. C., Lovato, N., Naik, G., Appleton, S., Adams, R., Escourrou, P., Catcheside, P., & Eckert D. J. (2023). Sleep Irregularity Is Associated With Hypertension: Findings From Over 2 Million Nights With a Large Global Population Sample. Hypertension.
(2) Makarem, Nour., Alcántara, C., Williams, N., Bello, N. A., & Abdalla, M. (2021). Effect of Sleep Disturbances on Blood Pressure. Hypertension.
(3) Nagai, M., Hoshide, S., & Kario, K. (2010). Sleep Duration as a Risk Factor for Cardiovascular Disease – a Review of the Recent Literature. Current Cardiology Reviews. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2845795/
(4) Grandner, M. A., Alfonso-Miller, P., Fernandez-Mendoza, J., Shetty, S., Shenoy, S., & Combs, D. (2016). Sleep: important considerations for the prevention of cardiovascular disease. Current Opinion in Cardiology.
(5) Grandner, M. A., Seixas, A., Shetty, S & Shenoy, S. (2016). Sleep Duration and Diabetes Risk: Population Trends and Potential Mechanisms. Current Diabetes Reports. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5070477/
(6) Gangwisch, J. E., Heymsfield, S. B., Boden-Albala, B., Buijs, R. M., Kreier, F., Pickering, T. G., Rundle, A. G., Zammit, G. K., & Malaspina, D. (2007). Sleep Duration as a Risk Factor for Diabetes Incidence in a Large US Sample. Sleep. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2276127/
(7) Garbarino, S., Lanteri, P., Bragazzi, N. L., Magnavita, N., & Scoditti, E. (2021). Role of sleep deprivation in immune-related disease risk and outcomes. Communications Biology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8602722/
(8) Besedovsky, L., Lange, T., & Born, J. (2012). Sleep and immune function. Pfulgers Archiv: European Journal of Physiology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3256323/
(9) Mullington, J. M., Simpson, N. S., Meier-Ewert, H. K., & Haack, M. (2010) Sleep Loss and Inflammation. Best Practice & Research Clinical Endocrinology & Metabolism. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3548567/
(10) Dzierzewski, J. M., Donovan, E. K., Kay, D. B., Sannes, T. S., & Bradbrook, K. E. (2020). Sleep Inconsistency and Markers of Inflammation. Frontiers in Neurology. https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2020.01042/full
(11) Everson, C. A., Henchen, C. J., Szabo, A., & Hogg, N. (2014). Cell Injury and Repair Resulting from Sleep Loss and Sleep Recovery in Laboratory Rats. Sleep. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4548518/
(12) Song, J., Park, S. J., Choi, S., Han, M., Cho, Y., Oh, Y. H., & Park, S. M. (2023). Effect of changes in sleeping behaviour on skeletal muscle and fat mass: a retrospective cohort study. BMC Public Health.
(13) Oliver, S. J., Costa, R. J. S., Laing, S. J., Bilzon, J. L. J., & Walsh, N. P. (2009). One night of sleep deprivation decreases treadmill endurance performance. European Journal of Applied Physiology.
(14) Chase, J. D., Roberson, P. A., Saunders, M. J., Hargens, T. A., Womack, C. J., & Luden, N. D. (2017). One night of sleep restriction following heavy exercise impairs 3-km cycling time-trial performance in the morning. Applied Physiology, Nutrition, and Metabolism.
(15) Grandner, M. A., Schopfer, E. A., Sands-Lincoln, M., Jackson, N., & Malhotra, A. (2015). The Relationship between Sleep Duration and Body Mass Index Depends on Age. Obesity (Silver Spring). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4700549/
(16) Li, Q. (2021). The association between sleep duration and excess body weight of the American adult population: a cross-sectional study of the national health and nutrition examination survey 2015-2016. BMC Public Health. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-10369-9
(17) Fry, A., & Rehman, A. (2023). Obesity and Sleep. Sleep Foundation. https://www.sleepfoundation.org/physical-health/obesity-and-sleep
(18) Franzen, P. L., & Buysse, D. J. (2008). Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues in Clinical Neuroscience. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3108260/
(19) Staner, L. (2003). Sleep and anxiety disorders. Dialogues in Clinical Neuroscience. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181635/
(20) Batterham, P. J., Glozier, N., & Christensen, H. (2012). Sleep disturbance, personality and the onset of depression and anxiety: Prospective cohort study. Australian & New Zealand Journal of Psychiatry.
(21) Arora, T., Grey, I., Östlundh, L., Alamoodi, A., Omar, O. M., Lam, K. H., & Grandner, M. (2022). A systematic review and meta-analysis to assess the relationship between sleep-duration/quality, mental toughness and resilience amongst healthy individuals. Sleep Medicine Reviews.
(22) Geng, S., Zhou, Y., Zhang, W., Lou, A., Cai, Y., Xie, J., Sun, J., Zhou, W., Liu, W., & Li, X. (2021). The influence of risk perception for COVID-19 pandemic on posttraumatic stress disorder for healthcare workers: A survey from four designated hospitals. Clinical Psychology & Psychotherapy.
(23) Shokri-Kojori, E., Wang, G., Weirs, C. E., Demiral, S. B., Guo, M., Kim, S. W., Lindgren, E., Ramirez, V., Zehra, A., Freeman, C., Miller, G., Manza, P., Srivastava, T., Santi, S. D., Tomasi, D., Benveniste, H., & Volkow, N. D. (2018). ß-Amyloid accumulation in the human brain after one night of sleep deprivation. PNAS.
(24) Spira, A. P., Chen-Edinboro, L. P., Wu, M. N., & Yaffe, K. (2014). Impact of sleep on the risk of cognitive decline and dementia. Current Opinion in Psychiatry.
(25) Horowitz, A. H., Esfahany, K., Gálvez, T. V., Maes, P., & Stickgold, R. (2023). Targeted dream incubation at sleep onset increases post-sleep creative performance. Scientific Reports.
(26) Lacaux, C., Andrillon, T., Bastoul, C., Idir, Y., Fonteix-Galet, A., Arnulf, I., & Oudiette, D. (2021). Sleep onset is a creative sweet spot. Science Advances. https://www.science.org/doi/10.1126/sciadv.abj5866
(27) Ganesan, S., Magee, M., Stone, J. E., Mulhall, M. D., Collins, A., Howard, M. E., Lockley, S. W., Rajaratnam, S. M. W., & Sletten, T. L. (2019). The Impact of Shift Work on Sleep, Alertness and Performance in Healthcare Workers. Scientific Reports.
(28) Kalmbach, D. A., Arnedt, J. T., Pillai, V., & Ciesla, J. A. (2015). The impact of sleep on female sexual response and behaviour: a pilot study. Journal of Sexual Medicine.
(29) Beroukhim, G., Esencan, E., & Seifer, D. B. (2022). Impact of sleep patterns upon female neuroendocrinology and reproductive outcomes: a comprehensive review. Reproductive Biology and Endocrinology.
https://rbej.biomedcentral.com/articles/10.1186/s12958-022-00889-3
(30) Oyetakin-White, P., Suggs, A., Koo, B., Matsui, M. S., Yarosh, D., Cooper, K. D., & Baron, E. D. (2015). Does poor sleep quality affect skin ageing? Clinical and Experimental Dermatology.
(31) Shao, L., Jian, S., Li, Y., Shi, Y., Wang, M., Liu, T., Yang, S., & Ma, L. (2022). Regular Late Bedtime Significantly Affects the Skin Physiological Characteristics and Skin Bacterial Microbiome. Clinical, Cosmetic and Investigational Dermatology.
(32) Cellini, N., Zambotti, M. D., Covassin, N., Sarlo, M., & Stegagno, L. (2014). Impaired off-line motor skills consolidation in young primary insomniacs. Neurobiology of Learning and Memory. https://www.sciencedirect.com/science/article/abs/pii/S1074742714001208
(33) Van den Berg, N. H., Pozzobon, A., Fang, Z., Al-Kuwatli, J., Toor, B., Ray, L. B., & Fogel, S. M. (2022). Sleep Enhances Consolidation of Memory Traces for Complex Problem-Solving Skills. Cerebral Cortex.
(34) Cappuccio, F. P., D’Elia, L., Strazzullo, P., & Miller, M. A. (2010). Sleep Duration and All-Cause Mortality: A Systematic Review and Meta-Analysis of Prospective Studies. Sleep. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2864873/
(35) Sambou, M. L., Zhao, X., Hong, T., Fan, J., Basnet, T. B., Zhu, M., Wang, C., Hang, D., Jiang, Y., & Dai, J. (2021). Associations Between Sleep Quality and Health Span: A Prospective Cohort Study Based on 328,850 UK Biobank Participants. Frontiers in Genetics. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8239359/
(36) Williams, T. B., Badariotti, J. I., Corbett, J., Miller-Dicks, M., Neupert, E., McMorris, T., Ando, S., Parker, M. O., Thelwell, R. C., Causer, A. J., Young, J. S., Mayes, H. S., White, D. K., de Carvalho, F. A., Tipton, M. J., & Costello, J. T. (2024). The effects of sleep deprivation, acute hypoxia, and exercise on cognitive performance: A multi-experiment combined stressors study. Physiology & Behaviour. https://www.sciencedirect.com/science/article/pii/S0031938423003347
(37) Drews, H. J., Sejling, C., Andersen, T. O., Varga, T. V., Jensen, A. K., & Rod, N. H. (2024). Tracked and self-reported nighttime smartphone use, general health, and healthcare utilization: results from the SmartSleep Study. Sleep.
(38) Fatima, Y., Doi, S. A. R., Najman, J. M., & Mamun, A. A. (2016). Exploring Gender Difference in Sleep Quality of Young Adults: Findings from a Large Population Study. Clinical Medicine & Research. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5302457/
(39) Bryan, L., & Cotliar, D. (2024). Melatonin: Usage, Side Effects and Safety. Sleep Foundation.
(40) Beil, L. (2023). How Sleep Affects Your Blood Sugar. WebMD.
(41) Pacheco, D., & Singh, A. (2023). Lack of Sleep and Diabetes. Sleep Foundation.






