
Craig Ballard
(MSc (Sports & Exercise Nutrition), BSc, BTEC (Sports & Exercise Sciences), CYQ/QCF (Personal training and Instruction))
With the advancements in antiepileptic drugs in the mid-20th century, the ketogenic diet was more or less forgotten. Beyond its original application for epilepsy, not many were recommending it as one of potential remedies for various medical conditions.
Even more so, the food industry and manufacturing of cheap foods, that are mostly based on carbohydrates, pushed the notion of a ketogenic diet out of the mainstream nutrition and dietetics conversations.
Today, however, we are making a full circle and we’re starting to re-learn the health benefits of low carbohydrate diets.
Definition of the Ketogenic Diet
The ketogenic diet is a subcategory of low carbohydrate diets, a nutritional approach characterised by a significant reduction in carbohydrate intake and an increased emphasis on consuming higher amounts of fats.
The ketogenic diet is designed to induce a metabolic state known as ketosis, also known as nutritional ketosis, which involves a shift in the body’s primary source of energy from carbohydrates to fats. The objective definition of a ketogenic diet is based on its capacity to increase the levels of circulating ketone bodies.
Different types of Ketogenic Diets
Various versions of the ketogenic diet exist. Nonetheless, most studies focused solely on the following types of ketogenic diet.
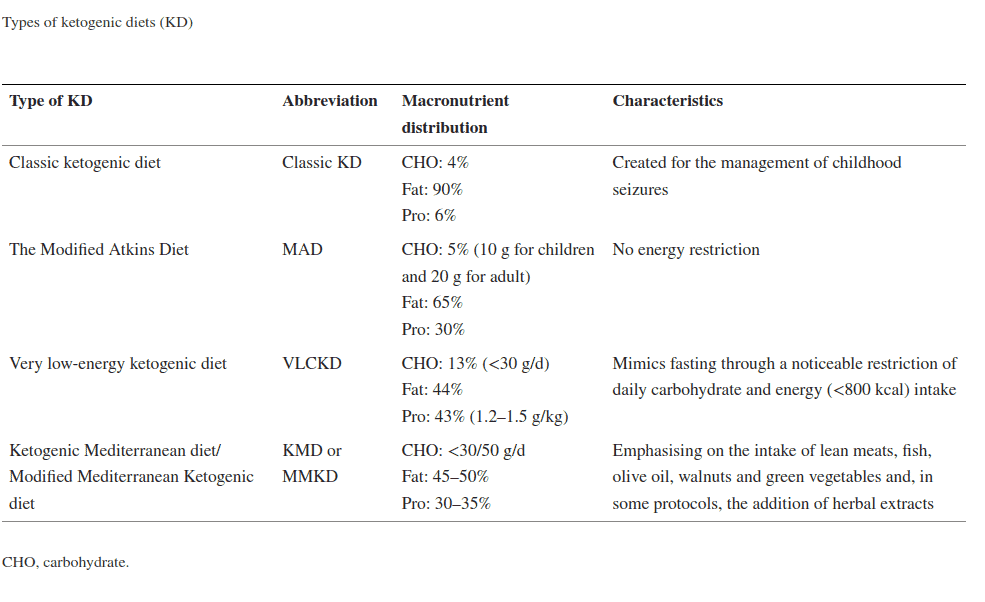
On average, the macronutrient portions of a ketogenic diet include:
High-Fat Intake
A key feature of a ketogenic diet involves a substantial rise in the intake of dietary fats, composing on average 65-75% of the overall daily calorie intake. Essential fat sources like avocados, nuts, seeds, and oils play a vital role in supporting the body during the absence of carbohydrates, supporting various bodily functions and promoting satiety.[1,2]
Nevertheless, animal fat is occasionally incorporated to achieve the targeted fat intake level.
Low Carbohydrate Intake
A ketogenic diet typically involves restricting daily carbohydrate intake to a range of 20-50 grams, usually composing only 5-10% of the total daily calorie intake. This low carbohydrate approach aims to deplete the body’s glycogen stores, triggering the utilisation of alternative energy sources like ketones.[1,2]
Nevertheless, participants following diets with carbohydrate intake of up to 192 g/day have shown elevated levels of circulating ketones.[3]
Moderate-Protein Intake
Protein intake is maintained at a moderate level, constituting around 20-30% of the daily calorie intake. Consuming an appropriate amount of protein ensures that the body has an adequate supply of amino acids for the maintenance of muscle mass and other vital functions.[1,2]
All while preventing excess protein from being converted into glucose (gluconeogenesis), which could interfere with the state of ketosis.
History of the Ketogenic Diet
In 1921, Dr. Russell Wilder introduced the ketogenic diet as a therapeutic dietary approach. Coined by Dr. Wilder, the term “ketogenic diet” stemmed from his research on ketone-producing diets in the 1920s and 1930s.[4]
This diet aimed to replicate the anti-seizure effects of fasting by inducing ketosis, all without requiring complete abstinence from food. The ketogenic diet became a prominent component in comprehensive textbooks on paediatric epilepsy from 1941 to 1980.[4]
Ketogenic diet started as a therapeutic approach for epilepsy
The ketogenic diet, initially overshadowed by antiepileptic drugs in the mid-20th century, experienced a resurgence in interest in the late 20th century. Beyond its original application for epilepsy, researchers explored its potential benefits in various medical conditions.[4]
In recent years, the ketogenic diet has gained widespread popularity as a lifestyle choice for weight loss, improved metabolic health and cognitive benefits.[4]
Understanding Ketosis
How the Body Enters a State of Ketosis
The body enters a state of ketosis when it shifts from using glucose to relying on ketones as its primary energy source. Initially, the body depletes its glycogen stores, which are stored forms of glucose in the liver and muscles. This occurs during a period of reduced carbohydrate intake, such as fasting or adherence to a low carbohydrate diet.[5]
Glycogen depletion increases breakdown of stored fats. Fatty acids are converted to ketones in the liver, and as ketone levels rise, the body transitions to using ketones for energy. This typically happens after a few days to weeks of reduced carbohydrate intake. This occurrence is termed ‘keto-adaptation’ or ‘fat adapted,’ and its manifestation can differ among individuals.[2]
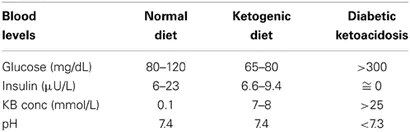
Blood ketone levels can be measured in millimoles per litre (mmol/L). Nutritional ketosis is achieved when ketone concentrations in the blood reach a range of 0.5 – 3.0 millimoles per litre (mmol/L). This is often measured through blood tests or urine ketone strips.[2,6]
While both methods are considered reliable, urine strips are generally considered less accurate compared to blood testing. However, in practical terms, ketone strips may be favoured due to their convenience and ease of use.[7]
A third approach to assessing ketone levels involves the use of commercial handheld ketone breathalysers. While current breath acetone sensors, including these handheld devices, have not undergone comprehensive testing, their versatility suggests they could be a viable option. That being said, their results may vary compared to simulated breath in laboratory conditions.[8]
In periods of drastic energy restriction it can reach a maximum of 7-8 mmol/L, often characterised as ketoacidosis. Ketoacidosis is a serious medical condition generally known as diabetic ketoacidosis because it typically only occurs in those with diabetes.[9,10]
If you would like to know more about diabetic ketoacidosis, see the link to the article below.
RELATED — Type 1 diabetes: Treatment and Management
Diagnosing diabetic ketoacidosis involves various methods, with three common indicators typically present: elevated plasma glucose, the presence of ketones in serum or urine, and the occurrence of acidosis indicated by serum bicarbonate levels.[10]
- Ketonaemia >3.0 mmol/L
- Blood glucose >11.0 mmol/L
- Bicarbonate (HCO3-) <15.0 mmol/L and/or venous pH <7.3
During ketoacidosis, ketone concentrations can escalate significantly, frequently surpassing 10 mmol/L. The pathophysiology of diabetic ketoacidosis is complex, influenced by hyperglycemia, dehydration, ketosis, and imbalances in electrolytes.[9,10]
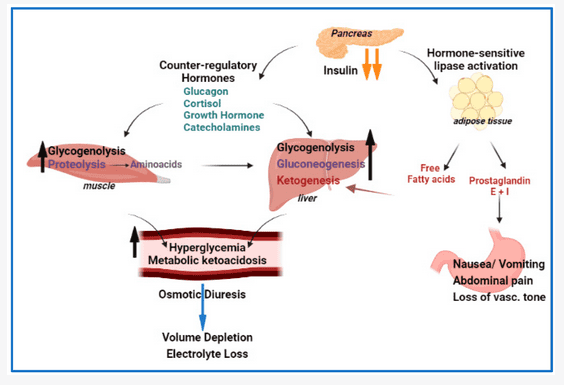
Activation of counter regulatory hormones drive hyperglycemia via various mechanisms including increased glycogenolysis, gluconeogenesis resulting in progressive volume depletion and electrolyte loss.
Role of liver-produced ketones
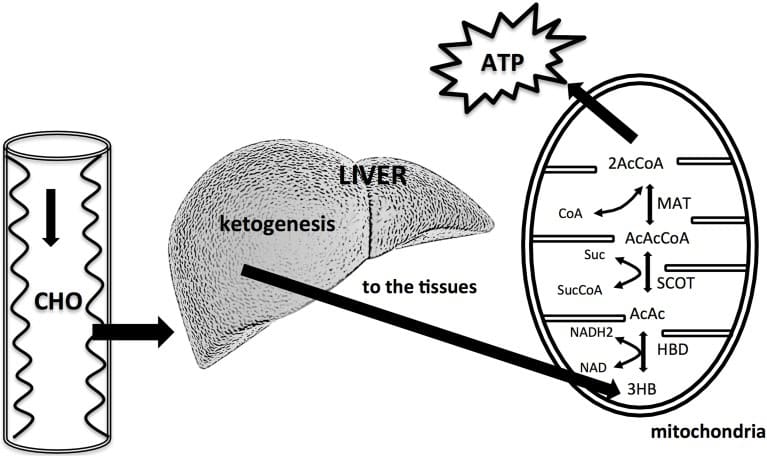
The liver is crucial in regulating the fluxes of glucose and fatty acids in both feeding and fasting states. Simultaneously, it relies significantly on the oxidation of these substrates to meet its own energy requirements.[11]
Ketones, including beta-hydroxybutyrate (BHB), acetoacetate, and acetone, are water-soluble compounds formed through the breakdown of fatty acids within the liver, known as ketogenesis.[11]
Acetoacetate, a product of fatty acid β-oxidation, can undergo two key transformations: reduction to β-hydroxybutyrate or decarboxylation to produce acetone. Acetone is the cause of the classic “keto breath”, a fruity odour produced through exhaling acetone.[11,12]
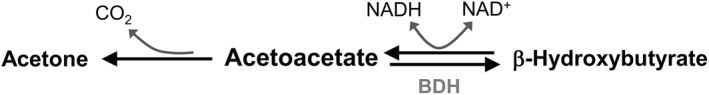
These substances are referred to as ketone bodies. Once produced, ketones are released into the bloodstream, where they serve as a source of fuel (ATP) for various tissues and organs throughout the body. However, the liver itself is incapable of utilising ketones as it lacks the enzyme 3-ketoacyl CoA transferase, which is required to convert acetoacetate into acetoacetyl-CoA.[11,12]
Ketones as brain fuel
The Central Nervous System (CNS) is unable to utilise fatty acids for energy due to the blood-brain barrier restricting the entry of free fatty acids.
Consequently, the brain primarily relies on glucose for its energy needs. When there is an absence of carbohydrate intake for 3–4 days, the CNS seeks alternative energy sources, and in this context, ketones become vital.[13,14]
Ketones possess the capability to cross the blood-brain barrier, making them a crucial energy source for the brain, particularly in situations of limited glucose availability. In periods of extended fasting or starvation, approximately 60% of the energy needed by the human brain can be supplied through a combination of acetoacetate and β-hydroxybutyrate.
Ketones can cross the blood-brain barrier
While ketones cannot completely substitute for glucose as a brain fuel, glucose remains indispensable for the brain.[13]
Ketones and preservation of muscle mass
Ketones function as an energy substrate that muscles can utilise, helping to conserve muscle proteins by preventing their breakdown for energy. This protein-sparing effect is advantageous for preserving muscle mass, especially during instances of calorie restriction or fasting, therefore supporting overall metabolic health.[14]
The preservation of lean mass is significantly influenced by energy intake. The ketogenic diet is frequently adopted by individuals aiming for rapid body mass loss. However, it is well-established that diets focused on swift body mass reduction are not effective at preserving fat free mass such as muscle tissue.[14]
Ketones and fat free mass
Building muscle mass on a ketogenic diet is possible, but it requires careful planning to ensure that you’re meeting your nutritional needs. Adopting a ketogenic diet without energy restriction, particularly in conjunction with resistance training, has the potential to result in increases in fat free mass, though is likely not optimal.[15,16]
This is primarily due to the emphasis on overall energy intake to achieve this goal. However, the satiating effect and the potential difficulty in maintaining adherence to a ketogenic diet make it less optimal as a nutritional strategy, particularly when sustained continuously for eight weeks or more.[17]
Ketones and glucose demand
With a reduced intake of carbohydrates and a reliance on fats for energy, the ketogenic diet helps stabilise blood sugar levels throughout the day. Foods with a high glycemic index can cause rapid spikes in blood sugar levels.[18]
The ketogenic diet, by nature, eliminates or limits such high glycemic foods, potentially reducing the overall glycemic response and helping to keep blood sugar levels more stable.[19]
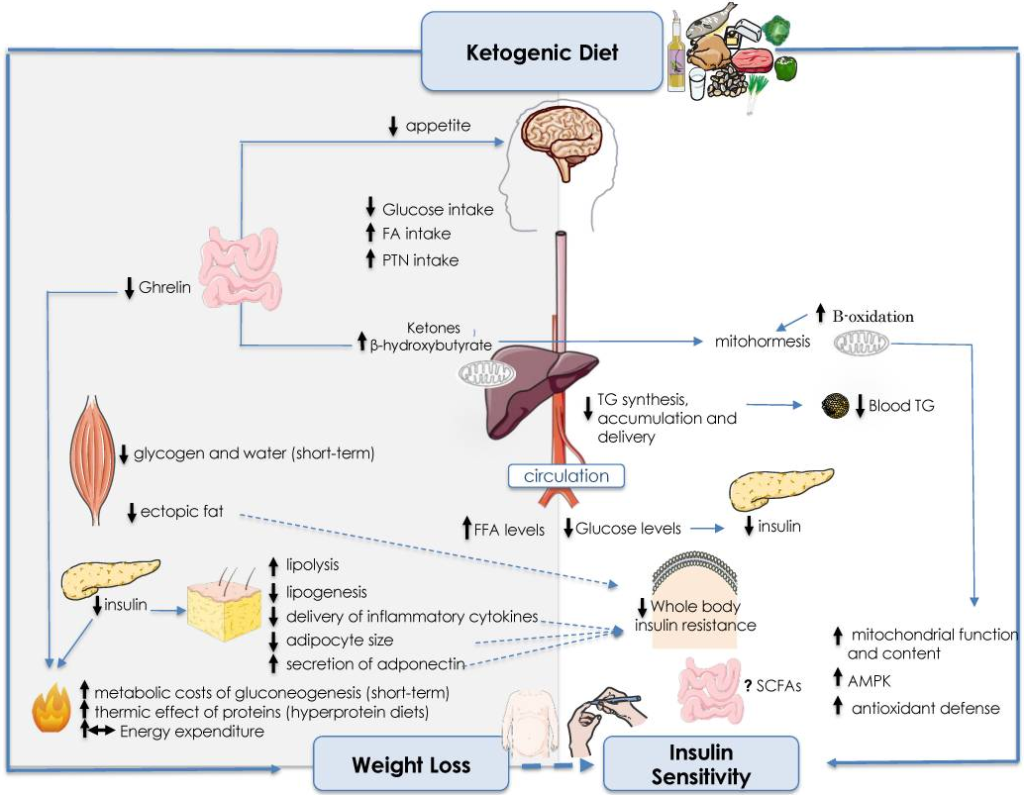
It has been proposed that the ketogenic diet might enhance insulin sensitivity. This implies that the body’s cells become more receptive to insulin, the hormone responsible for facilitating the transport of glucose into cells. Enhanced insulin sensitivity has the potential to result in improved blood sugar control.[18]
Ketones and efficient energy production
The CNS obtains energy from the production of acetyl coenzyme A. During ketosis and relative hypoglycemia, low levels of insulin directs this pathway toward the production of ketone bodies.[19]
In the extended periods of restricted carbohydrate intake, fasting or starvation, the body enhances its efficiency in oxidising fats for energy. This adaptation is prompted by hormonal shifts, including an elevation in glucagon and a reduction in insulin levels.[11,14]
Although numerous tissues can derive energy from ketones, certain cells, such as red blood cells and specific regions of the brain, remain dependent on glucose. The body’s adjustment to low carbohydrate diets and ketogenic diets aid in preserving glucose for these crucial functions, as ketones are utilised for other energy requirements.[14,19]
Metabolised within the cell’s mitochondria, ketones produce adenosine triphosphate (ATP), the primary energy currency of the cell. This process is more efficient than certain aspects of glycolysis, which is the breakdown of glucose.[11]
Contrast between carbohydrate and fat metabolism
On average, we only have a limited amount of glycogen stores in the body separated between the liver (~100g) and skeletal muscle tissue (~500g), roughly 2300 calories worth, which can be rapidly metabolised into glucose for energy.[20]
Adipose tissue however, can store a far greater amount of energy. A kilogram of body fat is roughly equivalent to around 7700 calories of stored energy. Fats, while offering a more sustained energy supply, require a longer, more intricate metabolic process.[20]
Glycolysis can occur without the need for oxygen (anaerobic metabolism), whereas beta-oxidation of fatty acids occurs in the mitochondria and requires oxygen, making it primarily an aerobic process.[20]
Benefits of the Ketogenic Diet
Ketones offer a steady and prolonged energy source, contrasting with the fluctuations in blood sugar levels linked to the ups and downs in energy associated with carbohydrate intake. It’s noteworthy that ketone bodies have the capacity to generate more energy than glucose, due to the changes in mitochondrial ATP production induced by KB.[11]
Weight loss
The ketogenic diet has accumulated significant popularity over the past decade, largely credited to its successful short-term impact on weight loss. Diets primarily focused on fat mass loss operate by maintaining a sustained caloric deficit.
The nature of a ketogenic diet, which involves depleting glycogen stores in the body, leads to substantial initial weight loss within the first few days. However, this initial reduction is primarily attributed to a decrease in body water, not a loss in fat mass.[1]
Glycogen stores, used for glucose storage, incorporate approximately 3 grams of water for every 1 gram of glycogen. Consequently, depleting glycogen also eliminates the water retained within it.[1]
Currently, no diet comparison, with matched protein between groups, has shown clinically significant fat loss for lower carbohydrate or ketogenic diets. Nevertheless, ketogenic diets have exhibited appetite suppressing potential, leading to spontaneous reductions in caloric intake without intentional caloric restriction.[1,21,22]
A ketogenic diet can result in significant fat mass loss without compromising muscle performance, despite reduced anabolic hormone concentrations. While studies consistently show the impact on fat mass, the effect on lean mass is not consistently confirmed.[1,16,17,21,22]
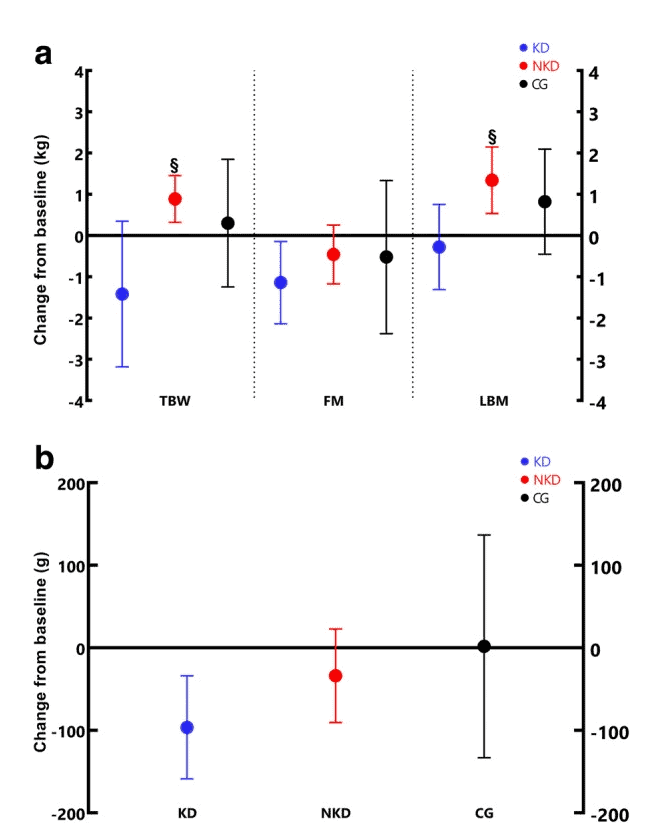
(A) Changes in BW, FM, LBM. (B) Changes in VAT. ǂ Significant difference with ketogenic diet.
Mechanisms behind ketogenic-induced weight loss
The ketogenic diet, focusing on reduced carbohydrate intake, enhances fat oxidation and promotes the production of appetite suppressing ketones. This approach aids weight management by stabilising blood sugar levels and improving insulin sensitivity. While it has the potential for fat loss and lean mass preservation, individual responses vary, and the diet’s long-term sustainability is a consideration.[1,14]
Weight loss on ketogenic diets may be linked to reduced appetite, related to observations in very low energy diets. However, evidence on the appetite suppressing effects of ketosis is largely anecdotal, and the specific mechanisms remain incompletely understood.[14,19,21]
Research findings on the effectiveness for weight management
Individuals with increased insulin resistance may benefit from a ketogenic diet due to reduced insulin needs for processing lower carbohydrate levels. Genotype variations might influence body mass loss responses to different diets.
Ketone bodies have both direct and indirect effects on appetite, potentially altering hunger-related hormones. Scientific evidence suggests that ketogenic diets are more effective, especially in the short to medium term, for fat loss by reducing energy intake.[23,24,25]
The limited food choices in a ketogenic diet may contribute to decreased energy intake and, consequently, fat mass reduction. Higher protein intake in ketogenic diets, with heightened dietary fat oxidation and elevated beta-hydroxybutyrate concentration, plays a role in enhanced appetite suppression.
Increasing protein intake is crucial for appetite suppression
While ketogenic diets are effective for fat mass loss, long-term effectiveness beyond six months may not surpass that of a well-balanced, energy-restricted diet.[22,26]
Brain Health
Cognitive benefits associated with ketosis
The ketogenic diet may support overall brain health by promoting mitochondrial function, reducing oxidative stress, and influencing the expression of genes related to brain function.[27,28]
RELATED — Introduction to: Brain Health
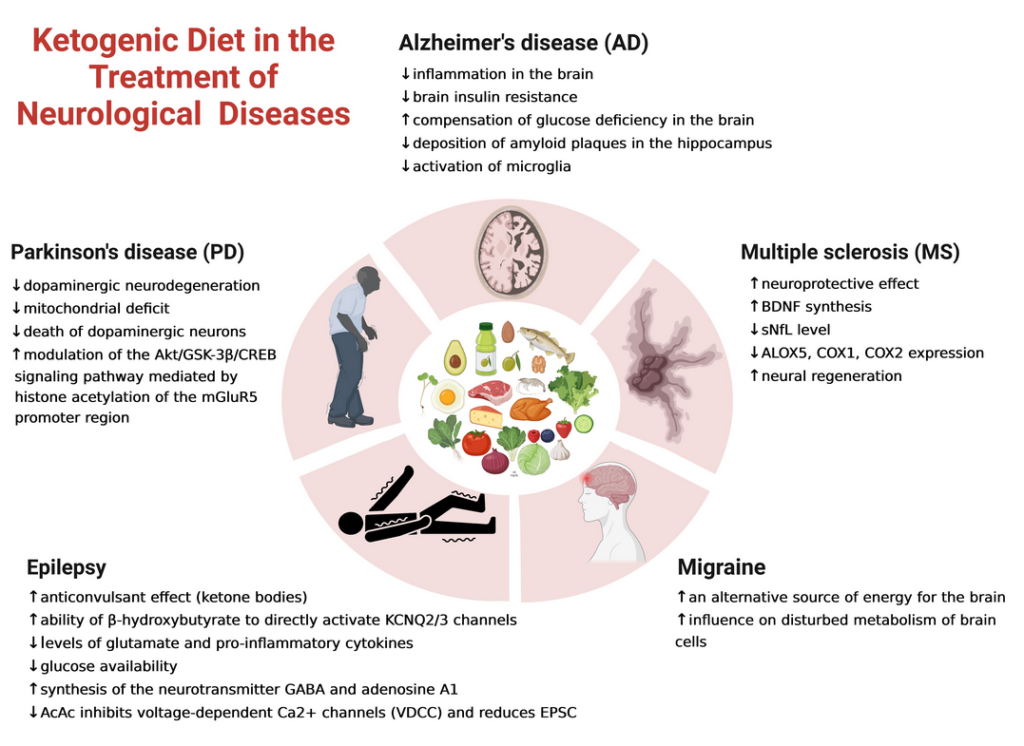
The ketogenic diet has been researched and applied as a therapeutic approach for specific neurological conditions, including:
- Epilepsy
- Alzheimer’s disease
- Parkinson’s disease
While the exact mechanisms are not completely understood, ketosis is believed to offer neuroprotective benefits in these cases.[27,28]
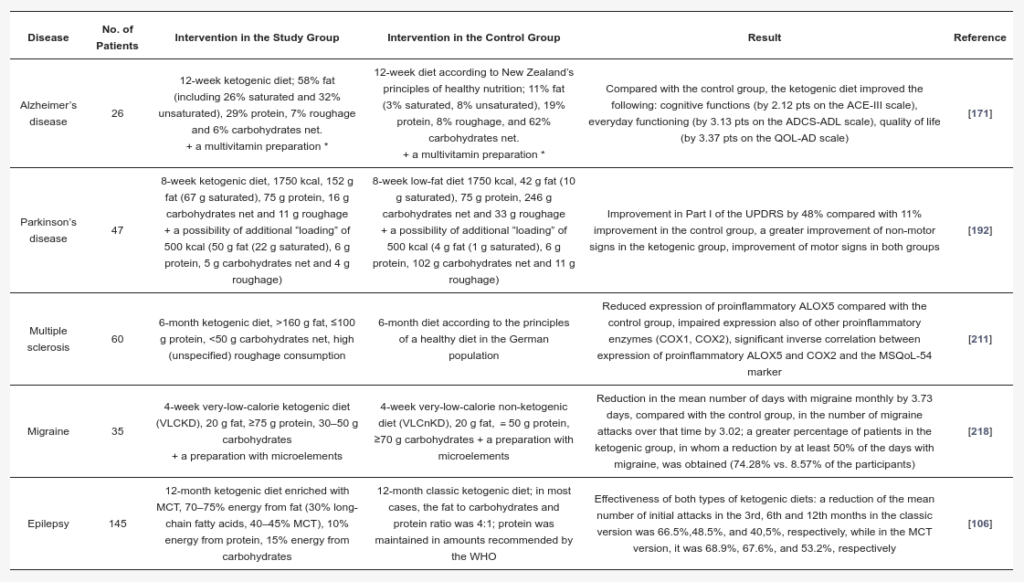
The most robust evidence supports a modest effect in slowing neurodegeneration, particularly in individuals experiencing the early stages of dementia or mild neurocognitive disorder. However, it’s crucial to note that research in this area is still in its early stages.[27,29]
The ketogenic diet’s anti-inflammatory effects may enhance cognitive function and memory, offering protection against neuroinflammation linked to cognitive decline and neurological disorders.
Ketones, studied for their potential neuroprotective effects, may contribute to the ketogenic diet’s positive impact on cerebral circulation and metabolic functions. The duration of maintaining high ketone body levels in the blood is thought to influence the positive effects on cognitive, metabolic, and biochemical functions.[13,27,29]
Physical Performance
The combination of a ketogenic diet with resistance training interventions may enhance the rate of fat mass loss, which may be advantageous for those wanting to improve power to weight ratio. However, compared to non-ketogenic diet approaches, it may not be a suitable dietary strategy for increasing muscle mass.[16,17,21]
A ketogenic diet can enhance endurance performance by increasing fat oxidation, especially in long-distance events. However, it may hinder muscle hypertrophy. For activities requiring lower intensities, a ketogenic diet may be beneficial or neutral, but it could reduce performance for activities above 70% VO2 max.
Related Questions
1. What are the top 5 keto foods?
We would suggest enjoying the following foods:
- Avocados: Rich in healthy fats, particularly monounsaturated fats. They are also low in carbohydrates and high in fibre, making them an excellent choice for a keto diet.
RELATED — Types of Fats: Healthy and Unhealthy Dietary Fats
- Eggs: Versatile and nutritious food that is naturally low in carbohydrates. They are an excellent source of protein and healthy fats, including omega-3 fatty acids.
RELATED — Everything You Need to Know When Buying Eggs (Part 1)
- Meat and Fatty Fish: Meats, such as beef, poultry, and pork, are staples of the keto diet. Fatty fish like salmon, mackerel, and sardines are rich in omega-3 fatty acids and provide a good source of protein without adding many carbs.
- Non-Starchy Vegetables: Low in carbohydrates and high in fibre, making them suitable for a keto diet. Examples include leafy greens (spinach, kale, lettuce), broccoli, cauliflower, zucchini, and bell peppers.
- Nuts and Seeds: Examples include almonds, walnuts, chia seeds, and flaxseeds. Be mindful of portion sizes, as nuts and seeds can be calorie-dense.
RELATED — Anti-cancer foods: The Healthiest Nuts (Part 1)
2. What are the symptoms of being in ketosis?
The following are the symptoms when your body is in ketosis:
- Keto Breath: Fruity or acetone smell on the breath.
- Increased Thirst and Dry Mouth: Dehydration may cause dryness in the mouth, leading to increased thirst.
- Increased Urination: Ketosis results in the breakdown of glycogen stores and increased loss of water.
- Keto Flu: Flu-like symptoms (fatigue, headaches, dizziness, irritability, nausea) during the initial transition.
- Appetite Suppression: Many experience a decrease in appetite due to the satiating effects of fat and protein.
- Improved Mental Clarity: Some report enhanced focus as the brain efficiently uses ketones for energy.
3. Does fasting enhance the effects of a ketogenic diet?
Fasting and a ketogenic diet share some similarities in terms of metabolic effects, as both can lead to increased ketone production and utilisation of fat for energy.
RELATED — Intermittent Fasting: Diet with actual health benefits
Combining intermittent fasting with a ketogenic diet may enhance some of the effects, but it’s important to approach this approach carefully and consider individual health needs. It’s crucial to approach fasting safely and ensure adequate nutrient intake during eating windows to support overall health.[32]
Are you looking to start a ketogenic diet, but have a few questions, and are unsure how to start. Let us know in the comments, and we’ll get back to you shortly.
Craig is a New Zealand registered nutritionist and personal trainer with over a decade of experience in the health and fitness sector delivering practical, evidence informed exercise and nutrition services. Most recently, Craig has qualified as a performance nutritionist from Leeds University in 2020.
With a strong inclination towards performance nutrition, Craig is particularly passionate about the utilisation of plant-based nutrition in the context of sports and athletics.
Throughout his extensive 12-year career as a health and fitness professional, Craig has collaborated with a diverse range of clients, which includes athletes at all levels, individuals competing in physique contests, and the general population.
Craig is dedicated to imparting knowledge to others by advocating for principles and practices related to physical well-being and lifestyle management.
References
(1) Ashtary-Larky, D., Bagheri, R., Bavi, H., Baker, J. S., Moro, T., Mancin, L., & Paoli, A. (2022). Ketogenic diets, physical activity and body composition: a review. The British journal of nutrition, 127(12). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9244428/
(2) Roekenes, J., & Martins, C. (2021). Ketogenic diets and appetite regulation. Current opinion in clinical nutrition and metabolic care, 24(4), 359–363. https://pubmed.ncbi.nlm.nih.gov/33883420/
(3) Deemer, S. E., Plaisance, E. P., & Martins, C. (2020). Impact of ketosis on appetite regulation-a review. Nutrition research (New York, N.Y.), 77, 1–11. https://doi.org/10.1016/j.nutres.2020.02.010
(4) Wheless J. W. (2008). History of the ketogenic diet. Epilepsia, 49 Suppl 8, 3–5. https://doi.org/10.1111/j.1528-1167.2008.01821.x
(5) El-Remessy, Azza B. 2022. Diabetic Ketoacidosis Management: Updates and Challenges for Specific Patient Population. Endocrines 3, no. 4. https://www.mdpi.com/2673-396X/3/4/66
(6) Harvey, C. J. D. C., Schofield, G. M., Zinn, C., & Thornley, S. (2019). Effects of differing levels of carbohydrate restriction on mood achievement of nutritional ketosis, and symptoms of carbohydrate withdrawal in healthy adults: A randomized clinical trial. Nutrition (Burbank, Los Angeles County, Calif.), 67-68S, 100005.
(7) Goffinet, L., Barrea, T., Beauloye, V., & Lysy, P. A. (2017). Blood versus urine ketone monitoring in a pediatric cohort of patients with type 1 diabetes: a crossover study. Therapeutic advances in endocrinology and metabolism, 8(1-2), 3–13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5298446/
(8) Alkedeh, O., & Priefer, R. (2021). The Ketogenic Diet: Breath Acetone Sensing Technology. Biosensors, 11(1), 26. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7835940/
(9) Fazeli Farsani, S., Brodovicz, K., Soleymanlou, N., Marquard, J., Wissinger, E., & Maiese, B. A. (2017). Incidence and prevalence of diabetic ketoacidosis (DKA) among adults with type 1 diabetes mellitus (T1D): a systematic literature review. BMJ open, 7(7), e016587. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5642652/
(10) Evans K. (2019). Diabetic ketoacidosis: update on management. Clinical medicine (London, England), 19(5), 396–398. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6771342/
(11) Paoli, A., Bosco, G., Camporesi, E. M., & Mangar, D. (2015). Ketosis, ketogenic diet and food intake control: a complex relationship. Frontiers in psychology, 6, 27. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4313585/
(12) Anderson, J. C., Mattar, S. G., Greenway, F. L., & Lindquist, R. J. (2021). Measuring ketone bodies for the monitoring of pathologic and therapeutic ketosis. Obesity science & practice, 7(5), 646–656. https://pubmed.ncbi.nlm.nih.gov/34631141/
(13) Cunnane, S., Nugent, S., Roy, M., Courchesne-Loyer, A., Croteau, E., Tremblay, S., Castellano, A., Pifferi, F., Bocti, C., Paquet, N., Begdouri, H., Bentourkia, M., Turcotte, E., Allard, M., Barberger-Gateau, P., Fulop, T., & Rapoport, S. I. (2011). Brain fuel metabolism, aging, and Alzheimer’s disease. Nutrition (Burbank, Los Angeles County, Calif.), 27(1), 3–20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3478067/
(14) Paoli, A., Bianco, A., Moro, T., Mota, J. F., & Coelho-Ravagnani, C. F. (2023). The Effects of Ketogenic Diet on Insulin Sensitivity and Weight Loss, Which Came First: The Chicken or the Egg?. Nutrients, 15(14), 3120. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10385501/
(15) Paoli, A., Cenci, L., Pompei, P., Sahin, N., Bianco, A., Neri, M., Caprio, M., & Moro, T. (2021). Effects of Two Months of Very Low Carbohydrate Ketogenic Diet on Body Composition, Muscle Strength, Muscle Area, and Blood Parameters in Competitive Natural Body Builders. Nutrients, 13(2), 374. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7911670/
(16) Vargas, S., Romance, R., Petro, J. L., Bonilla, D. A., Galancho, I., Espinar, S., Kreider, R. B., & Benítez-Porres, J. (2018). Efficacy of ketogenic diet on body composition during resistance training in trained men: a randomized controlled trial. Journal of the International Society of Sports Nutrition, 15(1), 31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6038311/
(17) Vargas-Molina, S., Gómez-Urquiza, J. L., García-Romero, J., & Benítez-Porres, J. (2022). Effects of the Ketogenic Diet on Muscle Hypertrophy in Resistance-Trained Men and Women: A Systematic Review and Meta-Analysis. International journal of environmental research and public health, 19(19), 12629. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9564904/
(18) Napoleão, A., Fernandes, L., Miranda, C., & Marum, A. P. (2021). Effects of Calorie Restriction on Health Span and Insulin Resistance: Classic Calorie Restriction Diet vs. Ketosis-Inducing Diet. Nutrients, 13(4), 1302. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8071299/
(19) Paoli A. (2014). Ketogenic diet for obesity: friend or foe?. International journal of environmental research and public health, 11(2), 2092–2107. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3945587/
(20) Murray, B., & Rosenbloom, C. (2018). Fundamentals of glycogen metabolism for coaches and athletes. Nutrition reviews, 76(4), 243–259. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6019055/
(21) Aragon, A. A., Schoenfeld, B. J., Wildman, R., Kleiner, S., VanDusseldorp, T., Taylor, L., Earnest, C. P., Arciero, P. J., Wilborn, C., Kalman, D. S., Stout, J. R., Willoughby, D. S., Campbell, B., Arent, S. M., Bannock, L., Smith-Ryan, A. E., & Antonio, J. (2017). International society of sports nutrition position stand: diets and body composition. Journal of the International Society of Sports Nutrition, 14, 16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5470183/#CR45
(22) Brinkworth, G. D., Noakes, M., Buckley, J. D., Keogh, J. B., & Clifton, P. M. (2009). Long-term effects of a very-low-carbohydrate weight loss diet compared with an isocaloric low-fat diet after 12 mo. The American journal of clinical nutrition, 90(1), 23–32. https://pubmed.ncbi.nlm.nih.gov/19439458/
(23) Sumithran, P., Prendergast, L. A., Delbridge, E., Purcell, K., Shulkes, A., Kriketos, A., & Proietto, J. (2013). Ketosis and appetite-mediating nutrients and hormones after weight loss. European journal of clinical nutrition, 67(7), 759–764. https://pubmed.ncbi.nlm.nih.gov/23632752/
(24) Di Rosa, C., Lattanzi, G., Spiezia, C., Imperia, E., Piccirilli, S., Beato, I., Gaspa, G., Micheli, V., De Joannon, F., Vallecorsa, N., Ciccozzi, M., Defeudis, G., Manfrini, S., & Khazrai, Y. M. (2022). Mediterranean Diet versus Very Low-Calorie Ketogenic Diet: Effects of Reaching 5% Body Weight Loss on Body Composition in Subjects with Overweight and with Obesity-A Cohort Study. International journal of environmental research and public health, 19(20), 13040. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9603454/
(25) Qi, Q., Bray, G. A., Hu, F. B., Sacks, F. M., & Qi, L. (2012). Weight-loss diets modify glucose-dependent insulinotropic polypeptide receptor rs2287019 genotype effects on changes in body weight, fasting glucose, and insulin resistance: the Preventing Overweight Using Novel Dietary Strategies trial. The American journal of clinical nutrition, 95(2), 506–513. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3260076/
(26) Tremblay, A., & Bellisle, F. (2015). Nutrients, satiety, and control of energy intake. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme, 40(10), 971–979. https://pubmed.ncbi.nlm.nih.gov/26394262/
(27) Pietrzak, D., Kasperek, K., Rękawek, P., & Piątkowska-Chmiel, I. (2022). The Therapeutic Role of Ketogenic Diet in Neurological Disorders. Nutrients, 14(9), 1952. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9102882/
(28) Crosby, L., Davis, B., Joshi, S., Jardine, M., Paul, J., Neola, M., & Barnard, N. D. (2021). Ketogenic Diets and Chronic Disease: Weighing the Benefits Against the Risks. Frontiers in nutrition, 8, 702802. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8322232/
(29) Dyńka D, Kowalcze K, Paziewska A. (2022). The Role of Ketogenic Diet in the Treatment of Neurological Diseases. Nutrients. 14(23), 5003. https://www.mdpi.com/2072-6643/14/23/5003#
(30) Cao, J., Lei, S., Wang, X., & Cheng, S. (2021). The Effect of a Ketogenic Low-Carbohydrate, High-Fat Diet on Aerobic Capacity and Exercise Performance in Endurance Athletes: A Systematic Review and Meta-Analysis. Nutrients, 13(8), 2896. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8400555/
(31) Burke L. M. (2021). Ketogenic low-CHO, high-fat diet: the future of elite endurance sport? The Journal of physiology, 599(3), 819–843. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7891323/
(32) Arora, N., Pulimamidi, S., Yadav, H., Jain, S., Glover, J., Dombrowski, K., Hernandez, B., Sarma, A. K., & Aneja, R. (2023). Intermittent fasting with ketogenic diet: A combination approach for management of chronic diseases. Clinical nutrition ESPEN, 54, 166–174. https://pubmed.ncbi.nlm.nih.gov/36963859/






