
Kàren Maggs
(Midlife and Menopause Coach, Menopause Doula and Certified practitioner My Menopause Transformation)
Hot flushes are the most common thought people have when we mention menopause.
Although there are over 30 other signs and symptoms, hot flushes seem to be the one that most women approach their doctor for help with.
Let’s investigate what hot flushes are, why they occur and what we can do about them.
What is a hot flush?
A hot flush is a sudden sensation of heat, often rising from the feet to the top of the head, that can come on very rapidly and dissipate just as quickly.
Some women feel overwhelmed by a hot flush, and will break out in a sweat as well as go red in the face. Some women feel like they are so hot they will self combust!
For other women, a hot flush can be a mild wave of warmth that goes through their body, causing no more than a slight sensation of a heat wave which quickly passes.
Most hot flushes disappear within a few minutes
Sometimes hot flushes can last up to 15 minutes.
They can be unpleasant and often occur when you least want them to — in a meeting at work, or when you are presenting in front of a group, which can make them quite a stressful experience.
Night sweats are another version of hot flushes but they occur at night while we are asleep.
Some women only have night sweats, some only hot flushes, and others get both varieties.
What causes a hot flush?
Although the medical world is still trying to fully understand hot flushes (or flashes as they are known in the US) there is an understanding that they occur because of temperature dysregulation in our hypothalamus (the part of the brain that controls temperature).
Essentially, the body thinks we are too hot and tries to cool us down rapidly by sending blood to the surface of our skin causing us to sweat and then cool down.
Hot flushes are called vasomotor symptoms in the medical world. “Vaso” relates to veins/blood vessels and “motor” relates to the nervous system, so in effect vasomotor symptoms are talking about the constriction or dilation of the blood vessels.
If you are suffering from hot flushes or night sweats, your health professional may indicate that you are suffering from vasomotor symptoms.
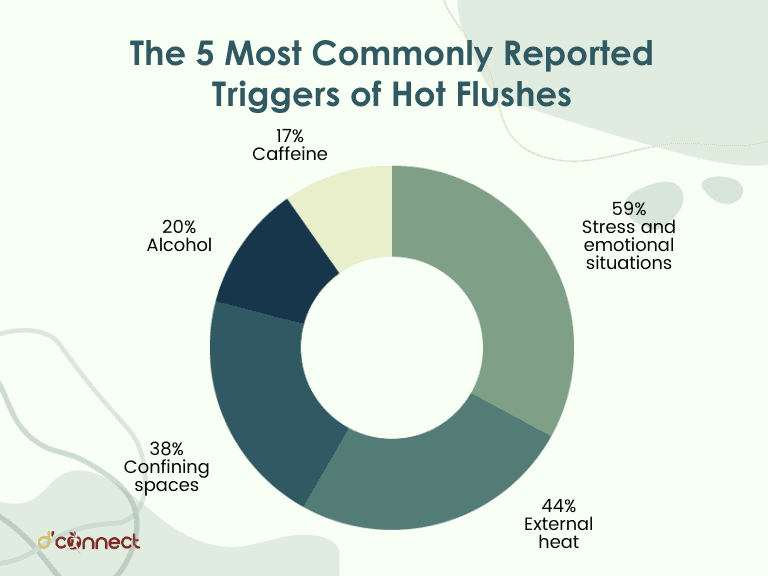
What triggers a hot flush or a night sweat?
There can be many triggers to a hot flush and they change with each individual. Sometimes it’s really hard to pinpoint but you may find some things on the list below that bring on hot flushes or night sweats for you:
- Alcohol
- Caffeine
- Smoking
- Spicy foods
- Being in a hot environment, stuffy rooms or warm weather
- Being in a situation in which you feel uncomfortable or under pressure (e.g. having to speak in front of a group of people)
- Thinking about things that make you feel uncomfortable
- Stress (even if it’s underlying and not something you are conscious of)
- A history of stressful events and/or trauma
- Lack of sleep
- Eating a big meal late at night, especially if it includes meat
- High intensity exercise
- Lack of water
- High intensity exercise[1]
What can you do to prevent hot flushes occurring?
Hot Flushes and lifestyle
Lifestyle changes can go a long way to managing hot flushes and night sweats, and some of the remedies are quite simple.
Track hot flushes and night sweats
Write down what you were doing or thinking at the time, how you were feeling, what you had been eating or drinking. This will help you to identify how many hot flushes/night sweats you are having per day or week, and what might be triggering them. You can find a downloadable tracker.
Reduce alcohol intake
Alcohol affects our thermoregulating system, and widens our blood vessels causing more blood to flow to the skin and causing us to heat up.
Hot flushes are due to a dysregulated thermoregulating system. So reducing alcohol intake will support you in reducing your hot flushes.
In addition, liver can reduce by up to 40% in menopause, meaning it doesn’t have the capacity to process the alcohol in your system like it used to. If you are waking with night sweats between 2.00-4.00 am when your liver is most active, this could be why.
Liver can reduce by up to 40% in menopause
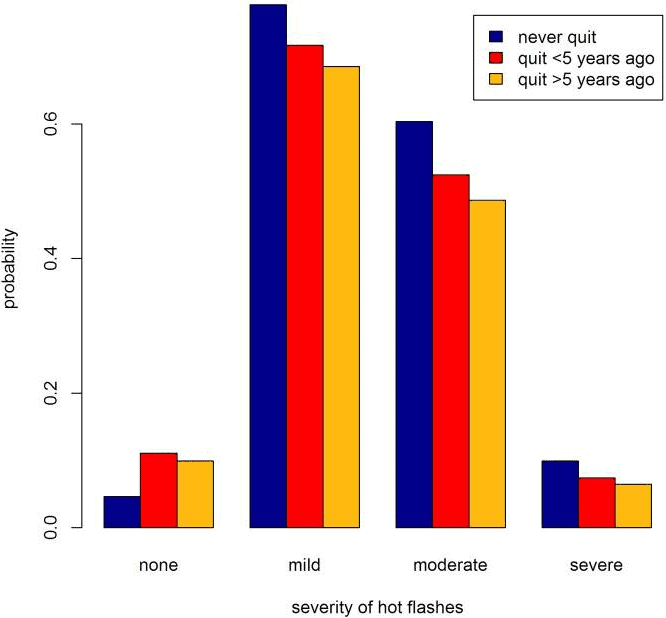
Stop smoking
Studies have shown that the sooner you stop smoking the less you will experience hot flush symptoms. Even if you are in the middle of experiencing hot flushes, it’s not too late. Stopping now may well reduce symptoms.[2]
Drink more water
Dehydration causes overheating. Increasing water intake can help the body stay cooler.
Avoid eating a large meat meal late in the evening
Meat is thermogenic, which means it takes a lot of energy to digest and causes body heat to rise.
Eating a big protein meal late in the evening means the body is trying to process this while you sleep and this can cause night sweats. Eat your meal earlier in the evening to allow your body time to digest food before sleep.
Eat folate rich fruits and vegetables
Eating foods that are high in folate/folic acid helps reduce the severity, duration and frequency of hot flushes.
You can find folate in spinach, silverbeet, broccoli, parsley, wholemeal breads and fresh citrus juices.[3]
Reduce your stress levels
Easier said than done, I know, but stress plays a big role in hot flushes and night sweats.
RELATED — Understanding Stress: The Silent Killer
Any way you can, reducing stress will help to decrease the load on your body and potentially reduce the frequency and/or severity of hot flushes.
Delegating work, saying no, practicing mindfulness and meditation, and healthy exercising will all help to reduce stress.
Avoid wearing synthetic fabrics
Synthetic clothes tend to be clingy and retain the heat. Try natural fibres like cotton and bamboo, or anything that wicks away the sweat when you are in the middle of a hot flush.
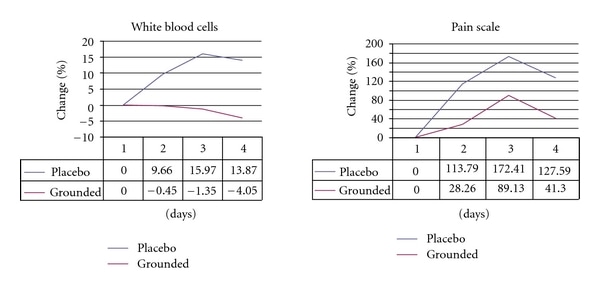
Put your feet on the ground
Believe it or not, the simple act of grounding, where we have our feet directly on the earth, helps to manage our heat regulation.
It also helps with stress, inflammation, pain and poor sleep. Standing or walking on the grass in bare feet for 15 minutes every day may help with hot flushes.[4]
Hot Flushes and medicinal drugs
Hormone Replacement Therapy (HRT) or Menopausal Hormone Therapy (MHT) as it is now called, is known and acknowledged to reduce hot flushes in women in perimenopause, menopause and post menopause.
There are varying alternatives for how this might be provided including pills, transdermal patches or IUD coils. Speak to your doctor about what MHT is right for you.
If you are on MHT and you are still experiencing hot flushes, talk to your doctor about changing to a different form.
Hot Flushes and supplements
Supplements such as Black Cohosh, Red Clover and Evening Primrose are suggested as options to manage hot flushes.
RELATED — 5 Natural Remedies for Menopause
However, there is much debate on the effectiveness of the supplements and studies show conflicting evidence in relation to their efficacy.[5]
Many supplements contain a range of anti-inflammatory and anti-anxiety herbs which may or may not be beneficial to you.
There is some concern about the interaction between herbal supplements and other medications you may be on, so talk to your doctor before taking any supplements to ensure it is safe for you to do so.
What can you do if you are in the middle of having a hot flush?
Hot flushes often occur at the most inopportune times which can be embarrassing. Being prepared and knowing your triggers will mean you manage them more easily, and make them less stressful.
Wear layers
Simple but effective; wearing multiple layers means you can strip off to quickly cool down and then add layers back on to warm up again.
Carry a handheld fan
These can be great for a quick cool down. You can even get some that spray a fine mist of water onto your face.
Frozen water bottle
If you are able to, keep a water bottle in the freezer and when a hot flush occurs, roll it under your feet, hold it in your hands or roll it on the back of your neck. This can help you to cool down quickly but be sure to wrap it in a cloth to ensure you protect your skin while doing so.
Cold/frozen items can help you cool down faster
Deep breathing
If your hot flush is induced by stress, then slow, deep breaths have been shown to help. Try breathing in for four and out for four until you feel calmer.
Related Questions
1. When should I be worried regarding hot flushes?
If you have five or more hot flushes in an hour, this could be an indicator that you are at risk of cardiovascular disease.
See your doctor to check whether cardiovascular disease is an issue for you.
2. At what age do hot flushes start?
This depends on when you start going through perimenopause.
Typically, hot flushes will appear in late perimenopause, so they’ll most likely start in your mid to late forties.
3. What happens right before having a hot flush?
More often than not, there is no warning that you are about to have a hot flush.
However, some women experience feelings of anxiety or nausea beforehand.
4. Why do I have hot flushes but I’m not in menopause?
If you are experiencing hot flushes but are not in perimenopause or menopause these could be caused by any medications you are taking or underlying health concerns.
See your doctor to investigate further.
5. How many hot flushes per day is considered normal?
The average number of hot flushes a day is 4-5, but some women experience up to 20 per day.
One in four women report having a hot flush every day.[6]
If you are nearing menopause, or are currently experiencing it, and have questions, please feel free to let us know in the comment section below.
Kàren supports women who are juggling the multiple challenges of midlife, managing their perimenopause and menopause symptoms, rediscovering themselves, as well as stepping into their Second Spring (their post menopause years), which is full of excitement, passion and purpose…
If you would like to learn more about Kàren, see Expert: Kàren Maggs.
References
(1) Carolyn J. Gibson, PhD, MPH1,2,3; Alison J. Huang, MD, MAS4; Brigid McCaw, MD, MPH, MS5; et al: 2019: Associations of Intimate Partner Violence, Sexual Assault, and Posttraumatic Stress Disorder With Menopause Symptoms Among Midlife and Older Women. Retrieved from https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2715160
(2) Rebecca L Smith; Jodi A Flaws; Lisa Gallichhio; June 2015: Does quitting smoking decrease the risk of midlife hot flashes? A longitudinal analysis. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4546860/
(3) S Bani; S Hasanpour; L Farzad Rik; H Hasankhani; SH Sharami: 2013: The Effect of Folic Acid on Menopausal Hot Flashes: A Randomized Clinical Trial. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4161099/
(4) G Chevalier; S T Sinatra; JL Oschman; K Sokal; P Sokal: 2012: Earthing: Health Implications of Reconnecting the Human Body to the Earth’s Surface Electrons. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3265077/
(5) Stacie E Geller; Laura Studee: 2005: Botanical and Dietary Supplements for Menopausal Symptoms: What Works, What Doesn’t. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1764641/
(6) Nancy E Avis; Sybil L Crawford; Robin Green: 2018: Vasomotor Symptoms Across the Menopause Transition: Differences Among Women. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6226273/






