
Kàren Maggs
(Midlife and Menopause Coach, Menopause Doula and Certified practitioner My Menopause Transformation)

Megan Rodden
(BCS, DipNat, MedHerb, NMHNZ)
Menopause occurs when a woman’s menstrual periods have ceased for 12 months or more. It’s something all women will go through but until recently there has been little information or support for women going through this important stage of their lives.
So let’s lift the veil on menopause and dive a little deeper.
The stages of menopause
Understanding the terms used around menopause can get confusing. There are four distinct phases that women go through.
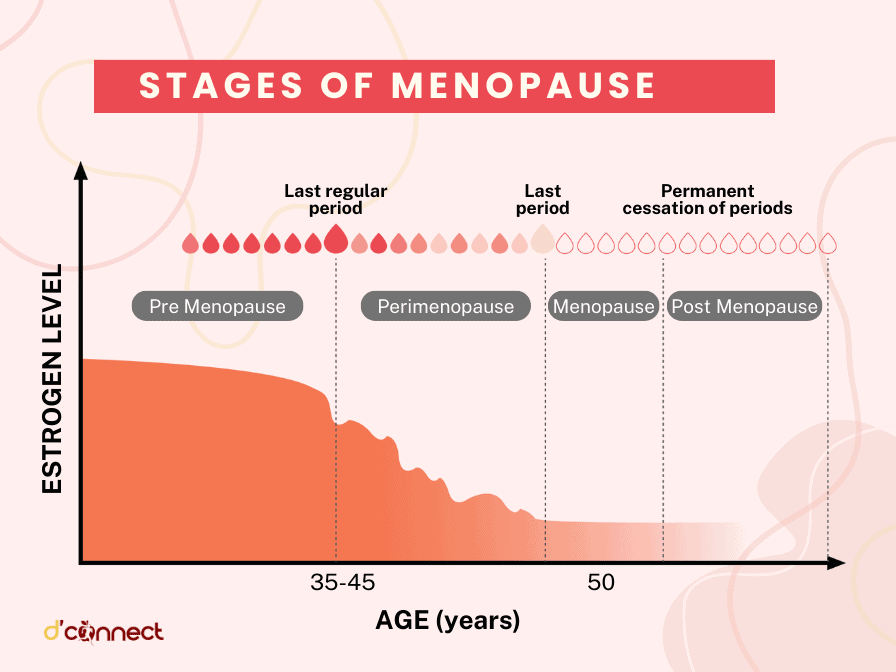
Pre menopause
This is when women are still having periods (either regular or irregular), and are considered to be in their reproductive years. Pre menopause means ‘before menopause’ and there are no signs or symptoms of perimenopause or menopause in this phase.
Perimenopause
Peri means ‘around’, so it really means ‘around menopause’. This is the time leading up to and just prior to menopause. It is when women are experiencing symptoms to a greater or lesser degree and can last anywhere from a year to 10 years or more.
Menopause
After 12 months of not having had a period you are said to be in menopause, i.e. your periods have ceased forever.
Post menopause
Post menopause is every day after you have reached menopause so in effect you are post menopausal from day 366 of your last period and will be in post menopause for the rest of your life.
Signs and symptoms of menopause
Physical symptoms
- Allergies — increase in allergies or onset of allergies.
- Bloating — tummy can feel distended, or you may be burping a lot or have a lot of flatulence.
- Breast tenderness — breasts may be tender all over or have sharp pains in certain areas. Tenderness can last all month and breasts may increase in cup size.
- Body odour changes — your normal body odour can become more pronounced.
- Burning mouth syndrome — you may feel a burning sensation on your tongue, the roof of your mouth, or on the inside of your lips.
- Digestive issues — there may be an increase in cramping with some nausea. Discomfort from increased gas can also be apparent.
- Dizziness — dizzy spells, spinning, lack of balance, and vertigo can increase during perimenopause.
- Electric shock sensations — this feels like little electric zaps occurring under the skin.
- Formication — this can feel like bugs crawling on your arms and legs, and you may find yourself constantly brushing your skin.
- Hot flushes — these can last from mere seconds to up to 30 minutes. It is when your body rapidly heats up to very high temperatures, and can cause your skin to flush and for you to break out in a sweat.
- Hair changes — hair suddenly starts to fall out more than normal, and you may also notice an increase in dark coloured facial hair.
- Headaches/migraines — these can increase in frequency and intensity, often starting in your 40s. If there’s a family history of migraines, it’s more likely you’ll experience them in perimenopause, or if you’ve had them before, they may become more intense.
- Incontinence — bladder leakage is often a result of childbirth and becomes more problematic in perimenopause, particularly if you cough, sneeze or jump.
- Irregular heartbeat — as hormones change in your body you heartbeat can be affected. It could be slow, fast or like a butterfly in your chest.
- Irregular menstrual cycle — a major symptom in perimenopause is cycles that are either shorter, longer or skipped altogether. Many women experience flooding, requiring additional support from sanitary products.
- Itchy and dry skin — caused by fluctuating hormones, skin can become very dry and itchy, and current skin conditions may worsen.
- Joint pain — often put down to over exercise, joint pain is experienced by many women in perimenopause.
- Muscle tension — can be caused by hormonal fluctuations rather than overwork, and causes the muscles in the body to tighten and become fatigued.
- Night sweats — similar to hot flushes but occurring at night. Night sweats cause you to wake drenched in sweat.
- Oral problems — gums can become painful and bleed, as well as receding, causing tooth loss.
- Osteoporosis — this is when bones become less dense and more brittle, meaning the increased possibility of fracture.
- Tingling extremities — you may find your hands, feet and legs become numb, or suffer more frequently from “pins and needles”.
- Urinary Tract Infections — unfortunately these can occur more frequently, with an increased need to urinate and then pain on passing urine.
- Vaginal dryness — falling oestrogen levels cause a lack of mucosa in the vagina which makes intercourse difficult, uncomfortable and often painful if grazing occurs. Burning, itching, spotting and pain are common symptoms.
- Weakened fingernails— fluctuating oestrogen causes the keratin layer in our nails to weaken, resulting in brittle fingernails and toenails.
- Weight gain — you’ve not changed your eating or exercise habits but weight suddenly piles on, particularly around the middle and doesn’t want to budge.
Mental and emotional symptoms
- Anxiety and panic attacks — you may suddenly experience panic or anxiety attacks when you’ve not had them before and they may be related to things that didn’t concern you previously.
- Brain fog — suddenly you can’t find the right words for normal, everyday objects or situations. You have difficulty concentrating for long periods of time and seem to forget things easily. You may be concerned you are getting early onset dementia, but it’s simply a result of your body adjusting to fluctuating hormones.
- Depression — lack of sleep and broken sleep can lead to less resilience in day-to-day life and bring on feelings of sadness and hopelessness. There can also be questioning of purpose and a general lack of happiness in your current life.[3]
- Fatigue — often caused by sleep disturbances or a general unhappiness in life, there can be feelings of extreme exhaustion or complete loss of energy.
- Feelings of dread — often these are unaccounted for and it’s unclear what you dread. Feelings are usually located in the pit of the stomach.
- Insomnia — you may find your brain is too busy, making it hard to fall asleep. Alternatively you may fall asleep only to wake frequently during the night, or wake early and not be able to get back to sleep.
- Irritability — you suddenly find that you have a very short fuse and that everything/everyone irritates and annoys you.
- Loss of libido — as your hormones fluctuate you may find that you have no interest in sex or that it’s very hard to get in the mood or stay in the mood.
- Mood swings — erratic mood swings, from joy to rage, can occur literally within minutes and then leave you. There can also be lots of tears, grief and sadness, sometimes for no apparent reason.
Around 20% of women won’t experience any symptoms or will only experience mild symptoms during their menopause transition.
However, 60% of women will experience moderate symptoms and 20% of women will experience severe symptoms that dramatically disrupt their life.[4]
The good news is that there is a lot that can be done to support women through these transitions, no matter what stage you are at.
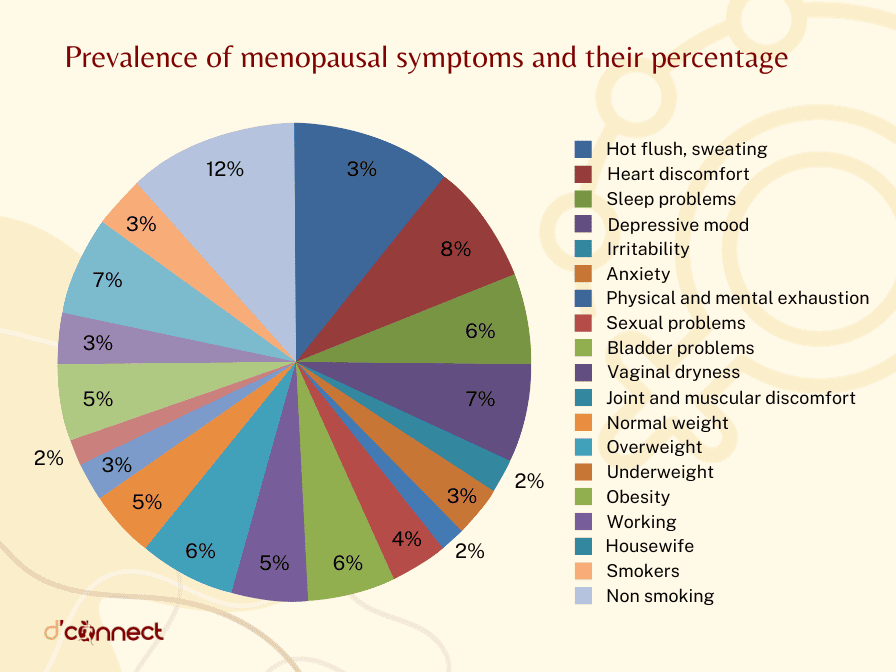
Source: Beadini, A. Menopause, Hormonal Changes and Osteoporosis among Women in Region of the Western Macedonia. International Journal of Biology. (2019).
If you are experiencing symptoms that are interfering with your day-to-day life or causing concern in some way, it is important to seek help from a health practitioner.
Related Questions
1. What is the typical age for menopause?
The average age for menopause globally is 51.4 years.
However, the range for menopause can be as early as late 30’s to 60. Most women go through menopause anywhere between their late 40’s and early 50’s.
2. How long does perimenopause last?It can range anywhere from 18 months to 10 years or more.
3. How do you know you are in perimenopause?
If you are in your 40’s, and are experiencing a number of the symptoms we shared earlier, you are likely to be in perimenopause.
Fluctuating menstrual cycles (longer or shorter, heavy or lighter bleeds) is a good indicator that you are in perimenopause.
4. What can you do to alleviate your symptoms?
There are a number of lifestyle changes you can make that will help you alleviate your symptoms. These are:
- Getting a good night’s sleep which means:
- Sleeping in a cool dark room
- Avoiding screens an hour before bedtime
- Avoiding stimulants such as caffeine before bedtime
- Keeping your bedroom for sleeping and sex (no TV)
- Having a regular wind down routine (e.g. reading a book before turning out your light)
- Maintain a healthy diet
- Include lots of fruit and vegetables
- Avoid alcohol and spicy foods as they bring on hot flushes and reduce deep sleep
- Identify your triggers for hot flushes in order to manage them better
- Reduce stress by delegating, practicing meditation and mindfulness, yoga, or walking in nature.[5]
RELATED — Understanding Stress: The Silent Killer
5. What are the best natural remedies for menopause?
Depending on your overall health, nutrition and other activities, as well as your symptoms, you might decide on including the following nutrients and herbs into your diet.
Magnesium is a nutrient that women may benefit from supplementing during both perimenopause and menopause.
- Magnesium improves resistance to physical and psychological stress that may be heightened during menopause and when taken in the evening may improve sleep.
- Magnesium supplementation may reduce the incidence and intensity of hot flashes.
RELATED — Magnesium (for a great night of sleep)
Vitex (also called Chaste tree/chasteberry or monk’s pepper) is a herb that may support women with symptoms of menopause.
- Vitex has been shown to reduce hot flashes, and improve mood and sleep.
- Vitex works by influencing receptors in the body that produce hormones, including progesterone.
Sage (Salvia officinalis) is another well known herbal remedy for menopause.
- Sage has properties that can modulate hormones and has been used in traditional herbal medicine to balance a deficiency in oestrogen. (Oestrogen levels naturally decline with the onset of menopause and this withdrawal is believed to contribute to symptoms)
- Sage contains phytoestrogens and has been found to reduce excess sweating and hot flashes. (Phytoestrogens are substances that are chemically similar to the hormone oestrogen but they occur naturally occur in plants)
Soy is a food supplement made from soybeans that is high in phytoestrogens and is often used to support menopause.
- A substance in soybeans called soy isoflavones and when eaten in high amounts may reduce hot flashes and night sweats.
- Soy foods high in isoflavones include miso and tofu.[6]
Fennel is a herb used to support menopause with an influence on levels of the hormone testosterone.
- Excess testosterone may contribute to symptoms during menopause and fennel has been used successfully to balance this.
- Fennel has been found to support symptoms of vaginal atrophy in menopause.
If you are interested in learning more about different herbs, we suggest visiting our Natural Medicine section.
Kàren supports women who are juggling the multiple challenges of midlife, managing their perimenopause and menopause symptoms, rediscovering themselves, as well as stepping into their Second Spring (their post menopause years), which is full of excitement, passion and purpose…
If you would like to learn more about Kàren, see Expert: Kàren Maggs.
Megan is a qualified, registered naturopath and medical herbalist based in Laingholm, Auckland. She is also a trained journalist with a bachelor’s degree in communication studies and a mother of two, with a passion for plant medicine and holistic nutrition…
If you would like to learn more about Megan, see Expert: Megan Rodden.
References
(1) Clinical manifestations and diagnosis of menopause. Author: Robert F Casper, MD. Retrieved from https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-menopause?search=Clinical%20manifestations%20and%20diagnosis%20of%20menopause%20Author:%20Robert%20F%20Casper,%20MD&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2
(2) Australian Menopause Society – Menopause management, Retrieved from https://www.menopause.org.au/hp/management
(3) Menopause and Depression: is there a link? Reviewed: Josephine Vivian-Taylor, Martha Hickey; Maturitas. 2014 Oct;79(2):142-6. doi: 10.1016/j.maturitas.2014.05.014. Epub 2014 Jun 2.
(4) Symptoms during the menopause: prevalence, severity, trajectory and significance in women’s lives. American Journal of Medicine (2005), vol 118 (12B) 14S-24S
(5) Polo-Kantola P. Sleep and Menopause. Women’s Health. 2007;3(1):99-106. doi:10.2217/17455057.3.1.99. Retrieved from https://journals.sagepub.com/doi/full/10.2217/17455057.3.1.99#bibr48-17455057-3-1-99
(6) Kargozar R, Azizi H, Salari R. A review of effective herbal medicines in controlling menopausal symptoms. Electron Physician. 2017 Nov 25;9(11):5826-5833. doi: 10.19082/5826. PMID: 29403626; PMCID: PMC5783135.






