
Hannah Zheng
Undergraduate in BSc Nutrition
Jump to:
- What is Sodium?
- Sodium deficiency
- Different types of Sodium
- Health Benefits
- Health Claims
- Best sources of Sodium
- Daily requirements and intake
- How to take Sodium
- Signs and symptoms of deficiency
- Risk and side effects
- Interactions - herbs and supplements
- Interactions - medication
- Summary
- Related Questions
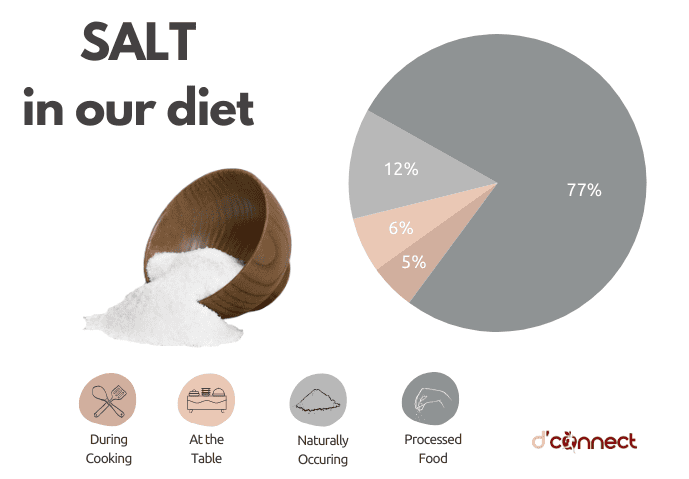
When enjoying a diet of wholefoods that have not been processed or packaged, our sodium levels are kept in check, and sometimes we might even be slightly deficient if exercising regularly.
However, with the advent of food manufacturing and the increase in processed and ultra-processed foods, many of us are consuming dangerously high amounts of sodium.
If we start in our late teens and early 20s, and continue with such nutrition for the next 20-30 years, are we putting ourselves at a higher risk of cardiovascular diseases?
What is Sodium?
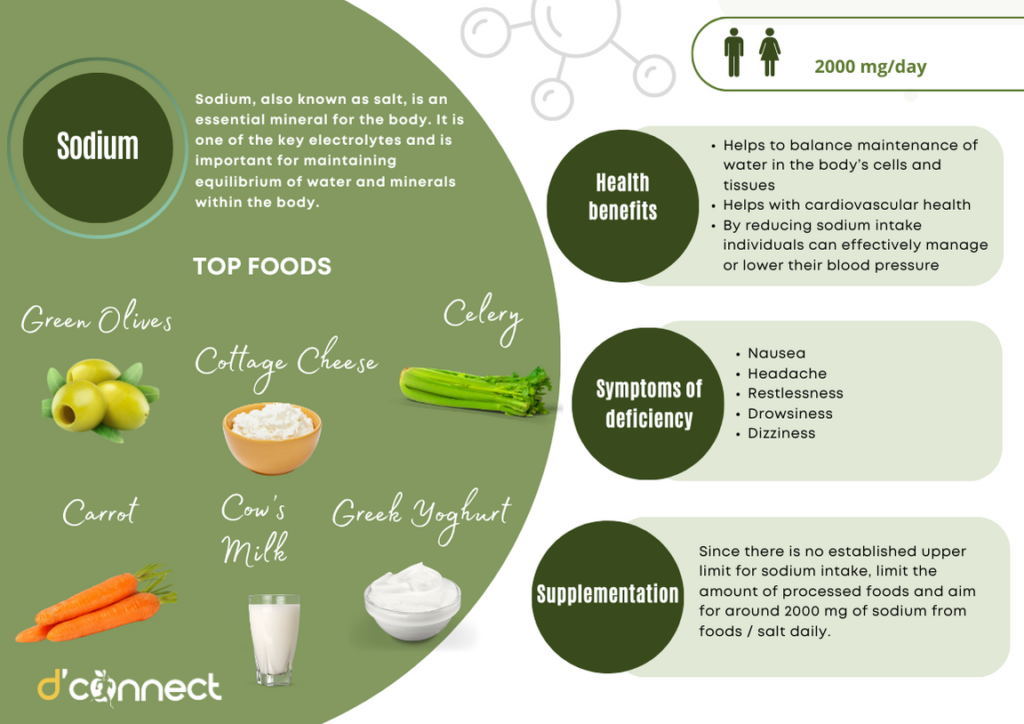
Sodium, also known as salt, is an essential mineral for the body. It is one of the key electrolytes and is important for maintaining equilibrium of water and minerals within the body.[1]
Other key electrolytes are potassium, chloride, phosphate, calcium and magnesium.
RELATED — Magnesium (for a great night of sleep)
It often acts in conjunction with potassium to regulate blood pressure and is integral for:
- Facilitation of muscle contraction and relaxation
- Transmitting nerve impulses
- Acid-base balance
- Regulating body temperature[2]
In 1938, sodium was first fortified with iodine to help New Zealanders consume sufficient amounts of iodine.[3]
Sodium is present in most processed foods
Since then sodium is present in many processed and packaged foods like bread, canned soup, and sauces. Its inclusion helps individuals meet their sodium needs as natural food sources may not supply adequate amounts.
History behind Sodium
Sodium was first discovered in 1807 by an English chemist, Humphry Davy. He used a method called electrolysis, which he also used to discover potassium. He used electricity from batteries through sodium hydroxide to get pure sodium.[4]
RELATED — Potassium (for blood pressure, heart rhythm and pH balance)
The discovery of sodium played a key role in advancing various industries, including food preservation and manufacturing, water treatment, and pharmaceuticals.
Sodium deficiency
Sodium deficiency, also known as hyponatremia, occurs when the body has a lower amount of sodium in the blood (normal range 135-145 mEq/L).[5]
It can be caused by factors like inadequate sodium intake, excessive sweating, diarrhoea, vomiting, certain medications, and medical conditions like kidney disease or heart failure.[6]
Sodium deficiency can be a result of:
- Inadequate dietary intake
- Poor absorption
- Increased loss
- Disorders and Diseases
- Age
However, both commercial foods and home-cooked meals typically contain sodium, making it unlikely for healthy individuals to experience sodium deficiency especially solely due to inadequate consumption of sodium.[7]
Who is most at risk of Sodium deficiency?
Hyponatremia is the most common electrolyte imbalance, defined as serum sodium level of less than 135 mEq/L. Individuals with hyponatremia are more prone to adverse outcomes like falls, fractures or prolonged hospitalisation.[8]
Athletes and intensive exercise
Elderly individuals and medications
As people age, the sense of thirst can diminish causing elderly individuals to not voluntarily consume fluids. This in turn can cause dehydration leading to sodium imbalance due to inadequate hydration levels.
Medications like diuretics more specifically thiazide diuretics is a common cause for sodium deficiency especially in elderly individuals. Thiazide diuretics inhibit the reabsorption of sodium ions on the distal convoluted tubule of the kidneys to help promote excretion of sodium along with water.[10,11]
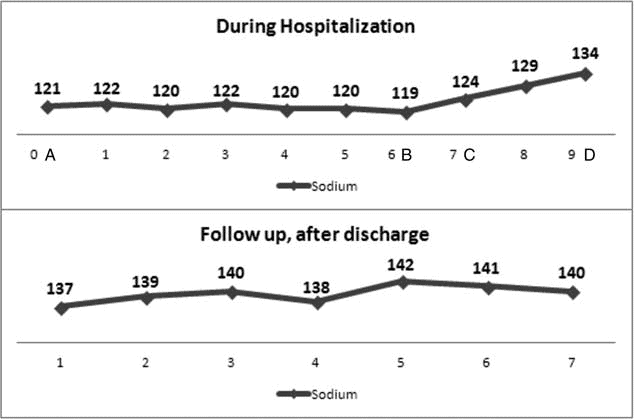
(A) Sodium level on admission was 121mEq/l.
(B) Sodium level on day 6 after admission was still 119mEq/l. On day 6 ACTH-stimulation test and CRH test took place, the initial diagnosis was made and the treatment with hydrocortisone started.
(C) 24 hours after starting treatment with hydrocortisone sodium level was 124mEq/l.
(D) Sodium level on day 9 after admission (Discharge date) was 134mEq/l.
Source: Grammatiki, Maria & Rapti, Patient With Severe Hyponatremia Caused by Adrenal Insufficiency Due to Ectopic Posterior Pituitary Lobe and Miscommunication Between Hypothalamus and Pituitary. (2016).
Certain medical conditions
In the majority of individuals with normal kidney function and blood pressure, the kidney typically has the capacity to manage fluctuations in sodium intake without resulting in elevated blood pressure.[12]
However, individuals with certain medical conditions become more susceptible to sodium deficiency such as:
- Heart Failure – causes fluid retention and dilution of sodium in the bloodstream.[13]
- Cirrhosis – impairs the liver’s ability to produce the protein (albumin) required to help maintain fluid balance in the body.[14]
- Kidney disease – disrupts the body’s ability to regulate sodium levels by impairing sodium excretion or retention.[15]
- Adrenal insufficiency/Addison’s disease – insufficient production of hormones (cortisol) which is key to sodium balance within the body.[16]
Different types of Sodium
There are a range of different types of sodium, most importantly they all contain the same compound, 40% sodium and 60% chloride.
- Table salt
- Sea salt
- Rock salt
- Pink Himalayan salt
- Kosher salt
If you’re choosing a salt, pink himalayan salt is a healthy option! If in need of more iodine in your diet you can opt for iodised salt.
Health benefits of Sodium
Sodium is present in all body tissues and is crucial for normal cell function. While it’s important to maintain a balanced diet that includes sodium, moderation is key.
Consuming adequate amounts of sodium offers various health benefits which are discussed further.
Fluid regulation and pH balance
Sodium, potassium and chloride, the main electrolytes in the body, help water balance maintenance in the body’s cells and tissues. Rapid changes in fluid and electrolyte level disrupt equilibrium, causing imbalances as cells struggle to adjust.[17,18]
The brain is vital for regulating body sodium by managing kidney function for water and salt balance.[19]
Sodium helps regulate the body’s acid-base balance and blood pH through mechanisms like sodium and hydrogen ion exchange, ensuring a balanced pH.[20]
Healthy blood pressure
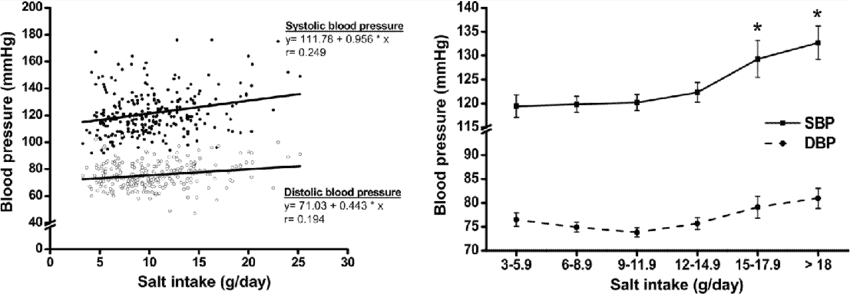
Excessive sodium consumption has been closely linked to elevated blood pressure. By reducing sodium intake or ensuring a balanced dietary approach, individuals can effectively manage or lower their blood pressure, thus mitigating the risk of cardiovascular complications implicated by high blood pressure.
Sodium works in blood pressure regulation primarily through its influence on fluid balance and vascular function.
Excessive sodium consumption is linked to elevated blood pressure
High sodium levels in the body can lead to increased water retention and heightened blood volume, exerting pressure on the arterial walls and contributing to elevated blood pressure.[21]
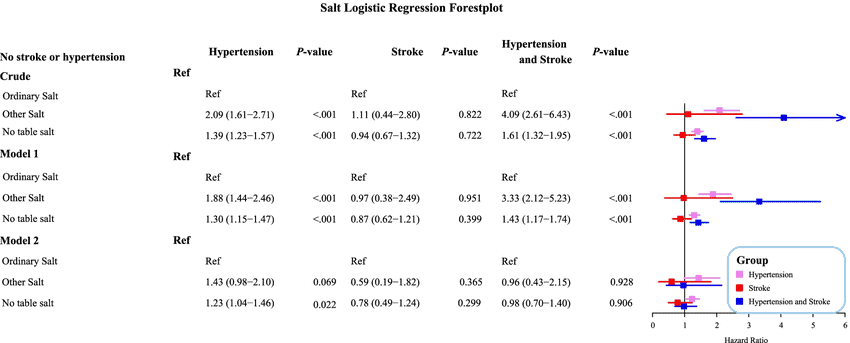
Reduction in stroke and cardiovascular diseases
Research suggests that lowering sodium intake is associated with reduced risk of stroke and cardiovascular disease.[22]
A high sodium diet draws water into the bloodstream in turn increasing the volume of blood, as well as blood pressure.
Uncontrolled high blood pressure can raise the risk of heart attack, heart failure, stroke, kidney disease, and blindness. In addition, blood pressure generally rises as we get older, so managing our sodium intake becomes even more important each year.[23,24]
Renal function
Increased sodium intake leads to an increase in intraglomerular pressure, which can cause or exacerbate chronic kidney damage and increase the risk of progressive kidney disease.[5]
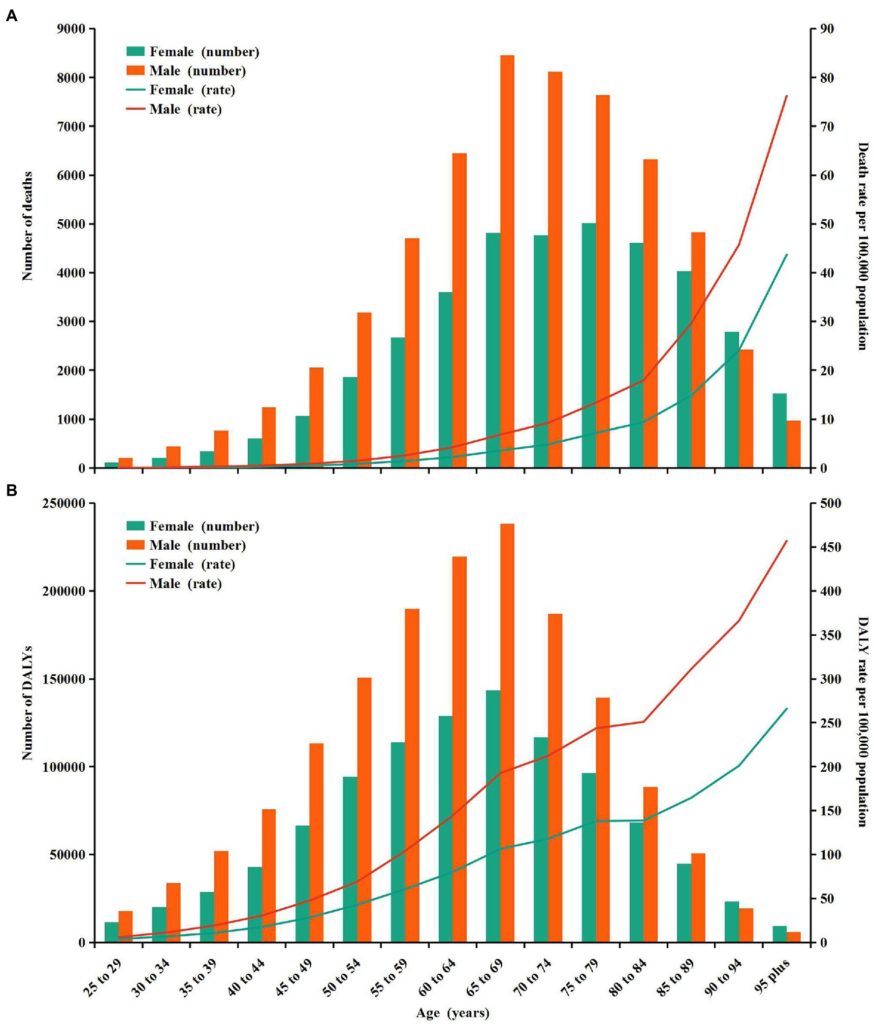
Source: Liu, W. Global, regional, and national burden of chronic kidney disease attributable to high sodium intake from 1990 to 2019. (2023)
Chronic kidney disease (CKD) is a major global public health concern, affecting nearly one in ten individuals.
Health claims that still need more evidence and research
While the impact of sodium on various aspects of health is well-documented, there are still some ongoing discussions about potential benefits that require further research before definite conclusions can be drawn.
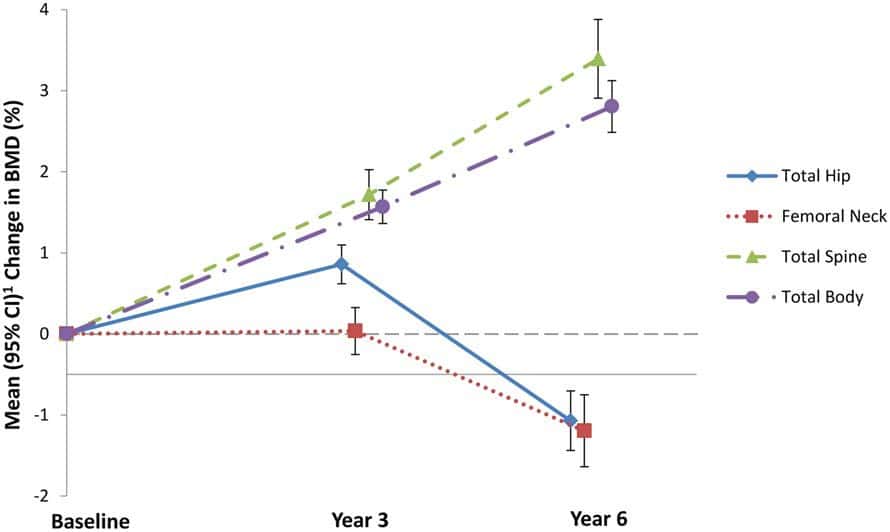
Bone Health
There is research that suggests that high sodium intake is associated with poor bone quality. Therefore, it is assumed that consuming less sodium, resulting in decreased sodium excretion, in turn preserving bone density and strength.[25,26]
Enhancing athletic performance
Although sodium plays a role in muscle function, and as previously discussed, sodium is excreted through sweating during exercise.
Athletes engaging in exercise can experience significant sodium loss through sweat causing an electrolyte imbalance.
Therefore, sodium supplementation plays a role in preserving electrolyte equilibrium, and is particularly beneficial during intense exercise or prolonged periods of sweating.
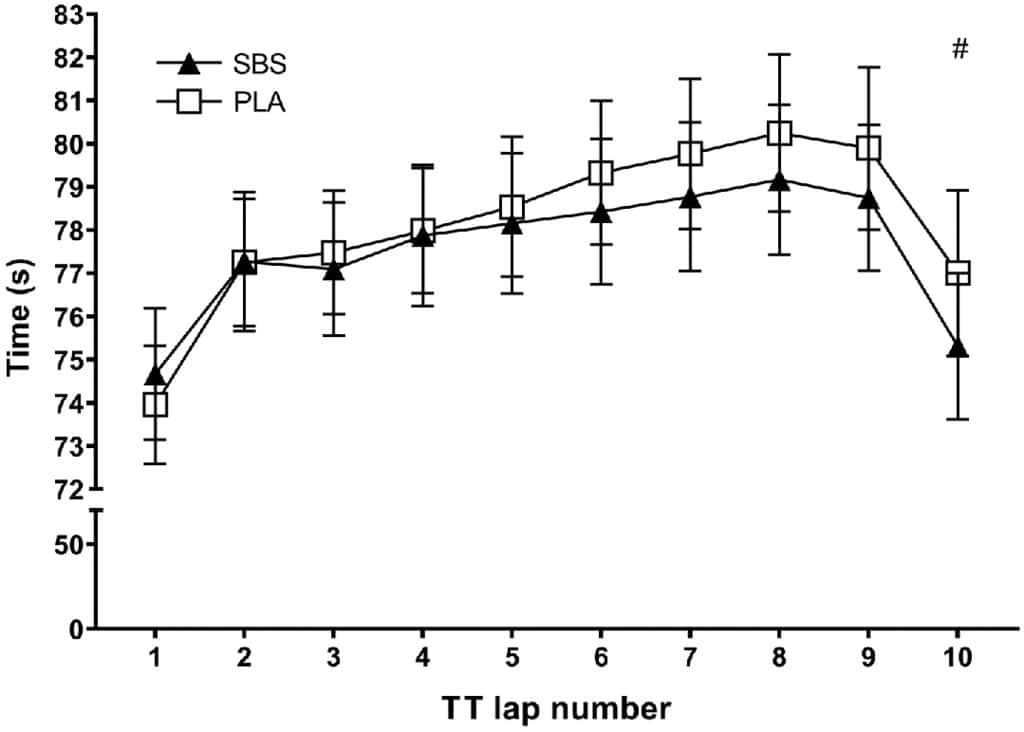
Sodium plays a role in the transport of glucose
Ensuring that there is adequate sodium levels is crucial for facilitating the transport of glucose and ensuring cells have the energy required to sustain high intensity exercise and optimal performance.[27]
However, sodium supplementation requires stronger scientific backing to make a strong conclusion about its efficacy in improving athletic outcomes.
Best sources of Sodium
Sodium is readily available in most commercial and home-cooked foods, making it easy to consume too much.
However, due to the risk of consuming too much sodium, it’s recommended to eat whole foods such as fresh fruits and vegetables, whole grains, and products with low salt content.
Food Source | Concentration (mg per 100g) |
Green olives | 300 |
Original cottage cheese | 136 |
Celery | 51 |
Carrot | 50 |
Cow’s milk | 40 |
Plain Greek yoghurt | 35 |
Spinach | 24 |
Cabbage | 16 |
Passionfruit | 10 |
Lettuce | 10 |
Mango | 7 |
White quinoa | 5 |
White button mushrooms | 4 |
Tomato | 2 |
Avoiding eating processed foods high in sodium, such as processed meats, potato chips, tomato sauce, and fast food.[28]
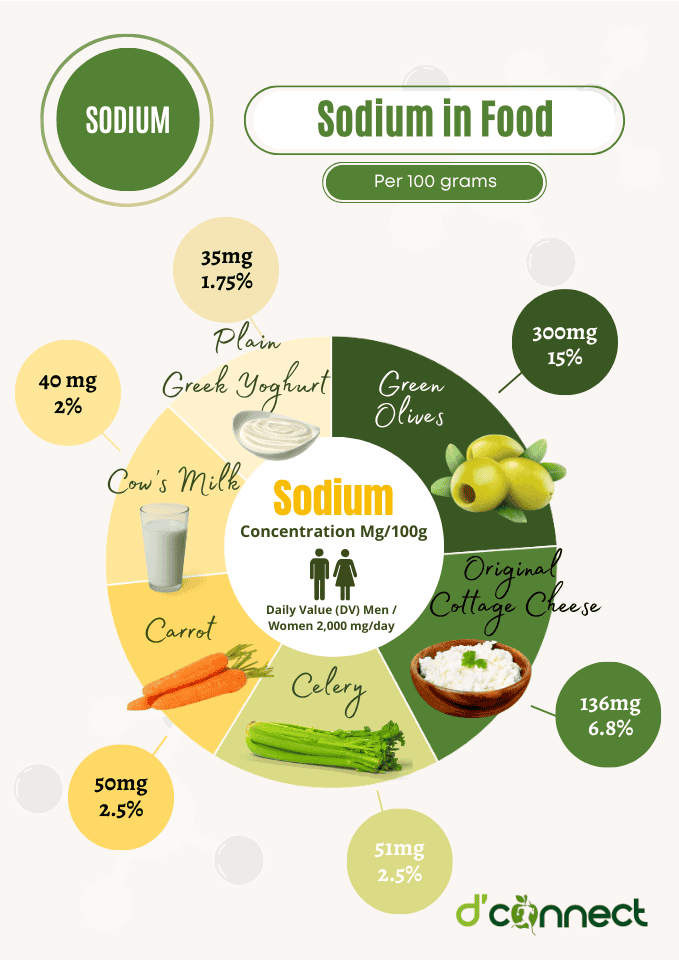
When purchasing packaged foods, review the nutrition label and select items low in salt.
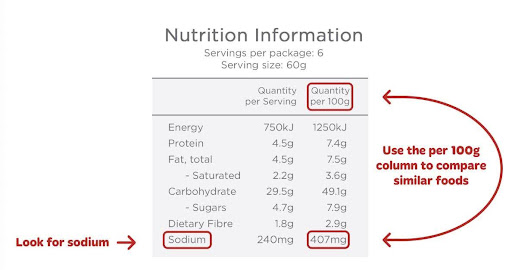
- Low-salt foods: less than 120 mg sodium per 100g.
- Medium-salt foods: 120-160 mg sodium per 100g.
- High-salt foods: more than 600 mg sodium per 100g.[29]
Daily requirements and recommended intake
The daily requirements shred below are from the Nutrient Reference Values (NRV) for Australia and New Zealand as well as the Ministry of Health.[30]
Age Group | Adequate Intake (mg/day) | Adequate intake (mmol/day) |
Infants (0-6 months) | 120 | 5.2 |
Infants (7-12 months) | 170 | 7.4 |
Children and Adolescents | – | – |
1-3 years | 200-400 | 9-17 |
4-8 years | 300-600 | 13-26 |
9-13 years | 400-800 | 17-34 |
14-18 years | 460-920 | 20-40 |
Adults | – | – |
Men (>18 years) | 460-920 | 20-40 |
Women (>18 years) | 460-920 | 20-40 |
Pregnancy | – | – |
14-18 years | 460-920 | 20-40 |
19-30 years | 460-920 | 20-40 |
31-50 years | 460-920 | 20-40 |
Lactation | – | – |
14-18 years | 460-920 | 20-40 |
19-30 years | 460-920 | 20-40 |
31-50 years | 460-920 | 20-40 |
Please note that daily requirements are different from the suggested dietary target, which at the moment is 2000 mg/day for men and women.
How to take Sodium as a supplement
Sodium is often included into many multivitamin supplements as well as standalone sodium supplements.
Different types of sodium supplements are:
- Powdered
- Capsules
- Tablets
- Liquid
Since there is no established upper limit for sodium intake, determining the safest maximum amount of sodium to consume remains uncertain.
Therefore, it is important to consult and seek guidance from a healthcare professional before incorporating sodium supplements into your routine.
Sodium supplementation may be necessary for some individuals, a balanced diet rich in whole foods is the best way to meet nutritional needs.
Common signs and symptoms of Sodium deficiency
Some patients with mild hyponatremia can often be asymptomatic, as the condition worsens, noticeable symptoms can develop.
Sodium risk and side effects
Excessive sodium intake can result in hypernatremia, also known as elevated serum sodium levels. This is defined as a serum sodium concentration >145 mEq/L.[33] This occurs due to high concentrations of sodium causing water to exit the cells, resulting in a shift in the osmotic pressure (force governing cellular movement).[20]
Excessive sodium consumption is linked to high blood pressure, a major risk factor for heart diseases like heart attack and stroke.
Possible interactions with herbs and supplements
Certain herbal supplements such as nettle, burdock root, hawthorn and dandelion may contain elevated sodium levels.
RELATED — Dandelion (Taraxacum officinale)
While these are generally considered beneficial for various health purposes, it’s important to be mindful of their sodium content, especially when incorporating them into your routine.
If consumed alongside sodium-rich foods, supplements, or packaged foods, it can lead to an overconsumption of sodium.
Other supplements like potassium, magnesium, iron, and vitamin D, can also be consumed in conjunction with sodium but their interaction with sodium can vary.[36,37,38]
Therefore, it’s advisable to seek guidance or advice from a healthcare professional or dietician before adding them into your routine.
Possible interactions with medication
There are a few medications that do not typically contain high levels of sodium, instead they directly affect sodium levels.
These are:
- Diuretics (decrease sodium reabsorption which causes an increase in sodium and water excretion)[39]
- Blood pressure medication
- Steroids
- Antidepressants
- Antiepileptic drugs
- Antipsychotics
All these medications can affect either sodium absorption and/or sodium levels. It would be best to seek professional medical advice first before taking sodium supplements.
Summary
Key Takeaway — In this illustration we have outlined the most important information that you should know about Sodium.
Related Questions
1. Can intermittent fasting disrupt sodium levels?
Intermittent fasting may alter sodium levels due to fluid intake and electrolyte balance changes. Imbalances can be caused if not managed with appropriate hydration and nutrition.
2. What is the best type of salt / highest quality?
Himalayan pink salt is the highest quality of salt as it contains over 80 minerals and trace elements including calcium, magnesium, potassium, copper and iron.
RELATED — Copper: Heart, Hair and Skin Health
3. Where does New Zealand salt come from / where is it produced?
Most of New Zealand salt comes from Lake Grassmere/Kapara Te Hau, where seawater evaporates, concentrating the salt for harvest through a natural process.
For similar articles, see our section of Nutrients, where you will find more information on vitamins, such as vitamin D, and minerals such as calcium.
Hannah is currently pursuing a Bachelor of Science degree majoring in Nutrition, with aspirations of advancing to Masters in Nutrition and Dietetics in the future. Her academic journey has fueled her interests in childhood nutrition, supplemental nutrition, and the intricacies of nutritional marketing.
Personally committed to living a healthier lifestyle, Hannah’s journey has sparked her interest in empowering others to make more informed dietary choices and advocating for better nutritional awareness.
References
(1) Shrimanker, I., Bhattarai, S. (2023). Electrolytes. National Center for Biotechnology Information. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK541123/
(2) Kaushik, S., Kumar, R., Kain, P. (2018). Salt an Essential Nutrient: Advances in Understanding Saly Taste Detection Using Drosophila as a Model System. https://doi.org/10.1177/1179069518806894
(3) Dalziel, L. (2008). Mandatory Iodine Fortification. Retrieved from https://www.beehive.govt.nz/feature/mandatory-iodine-fortification
(4) Weeks, M. E. (1932). The discovery of the elements. IX. Three alkali metals: Potassium, sodium, and lithium. Journal of Chemical Education, 9(6), 1035. https://doi.org/10.1021/ed009p1035
(5) Veniamakis, E., Kaplanis, G., Voulgaris, P., & Nikolaidis, P. T. (2022). Effects of Sodium Intake on Health and Performance in Endurance and Ultra-Endurance Sports. International journal of environmental research and public health, 19(6), 3651. https://doi.org/10.3390/ijerph19063651
(6) Adrogué, H. J., Tucker, B. M,. Madias, N. E. (2022). Diagnosis and Management of Hyponatremia: A Review. JAMA, 328(3):280–291. https://doi.org/10.1001/jama.2022.11176
(7) Strazzullo, P., Leclercq, C. (2014). Sodium. Advances in nutrition, 5(2),188-190. https://doi.org/10.3945/an.113.005215
(8) Jaques, D. A., Ponte, B. (2023). Dietary Sodium and Human Health. Nutrients, 15(17), 3696.
(9) Valentine, V. (2007). The Importance of Salt in the Athlete’s Diet. Current Sports Medicine Reports, 6(4), 237-240. Retrieved from https://journals.lww.com/acsm-csmr/fulltext/2007/08000/the_importance_of_salt _in_the_athlete_s_diet.9.aspx
(10) Falhammar, H., Skov, J., Calissendorff, J., et al. (2020). Associations Between Antihypertensive Medications and Severe Hyponatremia: A Swedish Population–Based Case–Control Study. The Journal of Clinical Endocrinology & Metabolism, 105(10), e3846. https://doi.org/10.1001/jamainternmed.2020.5258
(11) Hwang, K. S., Kim, G. H. (2010). Thiazide-induced hyponatremia. Electrolyte & blood pressure, 8(1), 51–57. https://doi.org/10.5049/EBP.2010.8.1.51
(12) Mente, A., O’Donnell, M., Yusuf, S. (2021). Sodium Intake and Health: What Should We Recommend Based on the Current Evidence?. Nutrients, 13(9), 3232. https://doi.org/10.3390/nu13093232
(13) Nijst, P., Verbrugge, F. H., Grieten, L., et al. (2015). The Pathophysiological Role of Interstitial Sodium in Heart Failure. Journal of the American College of Cardiology, 65(4), 378-388. https://doi.org/10.1016/j.jacc.2014.11.025
(14) Ginès, P., Guevara, M. (2008). Hyponatremia in Cirrhosis: Pathogenesis, clinical significance, and management. Hepatology, 48(3), 1002-1010. https://doi.org/10.1002/hep.22418
(15) Kovesdy, C, P. (2012). Significance of hypo- and hypernatremia in chronic kidney disease. Nephrology Dialysis Transplantation 27(3), 891-898. https://doi.org/10.1093/ndt/gfs038
(16) Kumar, S. S., Nagesh, V. K., Hunter, J., et al. (2021). A Case of severe Hypontremia in a Patient With Primary Adrenal Insufficiency. Cureus, 13(9), e17946. https://doi.org/10.7759/cureus.17946
(17) Bernal, A., Zafra, A. M., Simón, J. M., et al. (2023). Sodium Homeostasis, a Balance Necessary for Life. Nutrients, 15(2), 395. https://doi.org/10.3390/nu15020395
(18) Bhagavan, N. V. (2002). Water, Electrolytes, and Acid-Base Balance. Medical Biochemistry, 929–938. https://doi.org/10.1016/b978-012095440-7/50041-x
(19) Noda, M., Matsuda, T. (2022). Central regulation of body fluid homeostasis. Proceedings of the Japan Academy. Series B, Physical and biological sciences, 98(7), 283–324. https://doi.org/10.2183/pjab.98.016
(20) Callahan, A., Leonard, H., Powell, T. (2020). Vitamins and Minerals Involved In Fluid And Electrolyte Balance. Nutrition Science and Everyday Application v 10. Retrieved from https://openoregon.pressbooks.pub/nutritionscience/chapter/8d-vitamins-miner als-fluid-electrolyte-balance/
(21) Svetkey, L, P., Sacks, F. M., Obarzanek, E., et al. (1999). The DASH Diet, Sodium Intake and Blood Pressure Trial (DASH-Sodium). Journal of the Academy of Nutrition and Dietetics, 99(8), S96-S204.
(22) O’Donnell, M., Mente, A., Yusuf, S. (2015). Sodium intake and cardiovascular health. Circulation Res, 116(6), 1046-1057. https://doi.org/10.1161/CIRCRESAHA.116.303771
(23) U.S. Food and Drug Administration. (n.d.). Sodium in Your Diet. Retrieved from https://www.fda.gov/food/nutrition-education-resources-materials/sodium-yourdiet
(24) Agócs, R., Sugár, D., Szabó, A. J. (2020). Is too much salt harmful? Yes. Paediatric nephrology, 35(9), 1777–1785. https://doi.org/10.1007/s00467-019-04387-4
(25) Teucher, B., Dainty, J. R., Spinks, C. A., Majsak-Newman, G., et al. (2008). Sodium and Bone Health: Impact of Moderately High and Low Salt Intakes on Calcium Metabolism in Postmenopausal Women. Journal of Bone and Mineral Research, 23(9), 1477-1485. https://doi.org/10.1359/jbmr.080408
(26) Teucher, B., Fairweather-Tait, S. (2003). Dietary sodium as a risk factor for osteoporosis: where is the evidence? Proceedings of the Nutrition Society, 62(4), 859–866. https://doi.org/10.1079/PNS2003300
(27) Krustrup, P., Ermidis, G., Mohr, M. (2022). Sodium bicarbonate intake improves high-intensity intermittent exercise performance in trained young men. Journal of the International Society of Sports Nutrition, 12(1). https://doi.org/10.1186/s12970-015-0087-6
(28) Sodium added to Food. (2021). Ministry for Primary Industries. Retrieved from https://www.mpi.govt.nz/food-safety-home/nutrients-added-food/sodium-added-to-food/#:~:text=Avoid%20high%2Dsodium%20foods&text=These%20include%3A,as%20tomato%20and%20soy%20sauce
(29) Are you eating too much salt? (n.d.). Heart Foundation. Retrieved from https://www.heartfoundation.org.nz/wellbeing/healthy-eating/nutrition-facts/salt-and-blood-pressure#different-types-of-salt
(30) Nutrient reference values for Australia and New Zealand including recommended dietary intakes. (2006). Retrieved from https://www.nhmrc.gov.au/about-us/publications/nutrient-reference-values-aust ralia-and-new-zealand-including-recommended-dietary-intakes
(31) Reynolds, R. M., Padfield, P. L., Seckl, J. R. (2006). Disorders of sodium balance. BMJ, 332(7543), 702–705. https://doi.org/10.1136/bmj.332.7543.702
(32) Kugler, J. P., Hustead, T. (2000). Hyponatremia and hypernatremia in the elderly. American family physician, 61(12), 3623–3630. Retrieved from https://pubmed.ncbi.nlm.nih.gov/10892634/
(33) Al-Absi, A., Gosmanova, E. O., Wall, B. M. (2012). A clinical approach to the treatment of chronic hypernatremia. American Journal of Kidney Diseases, 60(6), 1032–1038. https://doi.org/10.1053/j.ajkd.2012.06.025
(34) Dong, O. M. (2018). Excessive dietary sodium intake and elevated blood pressure: a review of current prevention and management strategies and the emerging role of pharmaconutrigenetics. BMJ Nutrition, Prevention & Health. https://doi.org/10.1136/bmjnph-2018-000004
(35) Kotchen, T. A., Kotchen, J. M. (1997). Dietary Sodium and blood pressure: interactions with other nutrients. The American Journal of Clinical Nutrition 65(2), 708S-711S. https://doi.org/10.1093/ajcn/65.2.708S
(36) Harvard Health Publishing. (n.d.). Nutrition’s dynamic duos. Harvard Health Publishing. Retrieved from https://www.health.harvard.edu/newsletter_article/Nutritions-dynamic-duos
(37) Healthy diet. (n.d.). World Health Organization. Retrieved from https://www.who.int/news-room/fact-sheets/detail/healthy-diet
(38) Yetley, E. A. (2007) Multivitamin and multimineral dietary supplements: definitions, characterization, bioavailability, and drug interactions. The American Journal of Clinical Nutrition, 85(1), 269S-276S. https://doi.org/10.1093/ajcn/85.1.269S
(39) Louden, J. D. (2015). Regulation of fluid and electrolyte balance. Anaesthesia & Intensive Care Medicine 16(6), 278-285. https://doi.org/10.1016/j.mpaic.2015.03.007





