
Carly Hanna
BSc (Human Nutrition and Psychology)
While coeliac disease is considered a gastrointestinal disorder, it can also have effects on other areas of the body if not addressed and treated.
The associated health risks that come with coeliac disease are complex, and in this 2-part series we will look at the 11 most common health issues that can be caused by coeliac disease.
Nutrient deficiencies
Due to the diminished ability of the gastrointestinal system to absorb nutrients, individuals with coeliac disease are at higher risk for vitamin and mineral deficiencies.
The most common nutrient deficiencies in coeliac disease are:
- iron
- folic acid
- vitamin B12
- calcium
- zinc
- vitamin D
RELATED — Vitamin D: The sunshine hormone for stronger bones
This is because gluten-free food alternatives may not have the same amount of micronutrients that their gluten foods have.
In this table we can see the overview of nutrient deficiencies in the general population and those with coeliac disease.
Coeliac disease | General population | |
Iron | 6-82% | 17% |
Folic acid | 11-75% | 4-14% |
Vitamin B12 | 5-19% | 7-17% |
Vitamin D | 0-70% | 50% |
Calcium | 0-41% | 0% |
Zinc | 67% | No data available |
Table based on Narrative Review: Nutrient Deficiencies in Adults and Children with Treated and Untreated Celiac Disease. (2020)
Osteoporosis
The prevalence of osteoporosis in men and women with coeliac disease is up to 20%.[1] Having osteoporosis means that there is an increased risk for fractures and broken bones.
The risk of osteoporosis can increase due to nutrient deficiencies such as folic acid, calcium, and vitamin D. This is because calcium and vitamin D are essential for bone health.
A life-long gluten free diet can improve bone mineral density
This is especially so for childhood onset of coeliac disease as our bone mineral density increases up until about 25 years of age.[2]
Not eating gluten can allow the small intestine to heal and absorb nutrients as much as possible.
This means that if we eat enough calcium for our requirements, we can decrease our risk of a calcium deficiency and osteoporosis.
Fertility issues
Although evidence is still preliminary, some studies show that having untreated coeliac disease can cause:
- infertility and recurrent miscarriages
- pregnancy complications (e.g. premature births)
- late menarche (late-onset puberty)
- early menopause
- amenorrhoea (absent menstrual periods)[1]
RELATED — Menopause: Guide to Signs and Symptoms
Some evidence suggests that this is only the case for women aged 25–29 years old, who have a 41% higher risk of fertility issues than those without coeliac disease.[3]
Coeliac disease is often a disease that is screened for when there is unexplained fertility. Those with coeliac disease who wish to conceive need to be extra considerate of their nutrition to make sure they are getting enough nutrients for pregnancy.[4]
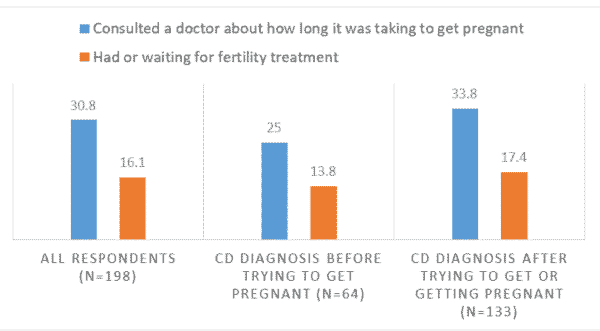
Source: Coeliac New Zealand
While the link between fertility issues and coeliac disease are still not exactly known, the probable mechanism could be that those with coeliac have altered hormonal levels and/or lower body mass. This will affect menstruation and fertility.[3]
Mental health issues
Having coeliac disease has been shown to correlate with an increase in mental health condition prevalence and severity such as:
- depression
- anxiety
- suicide
- eating disorders
RELATED — Understanding Eating Disorders: History, Types and Statistics
This can be due to a multitude of reasons, but most commonly due to the burden or dietary restriction on their personal, social and cultural wellbeing.[1]
Depression
Depression is characterised by feelings of low mood, lack of pleasure in activities there were enjoyable previously, sleeping and/or appetite changes, and feelings of sadness and/or hopelessness.
Depression is the most common psychiatric symptom comorbid with autoimmune diseases, such as coeliac disease.
RELATED — Introduction to: Depression
The biological explanation for this is that depression is associated with high levels of anti-inflammatory markers, which is also presented in coeliac disease.
The relationship between depression and coeliac disease can be bi-directional, meaning that one condition can come before the other.[5]
Depression is also commonly associated with anxiety.
Anxiety
Following a gluten-free diet can put strain on one’s mental health and social relationships.
This can be due to worrying about if foods contain gluten, how they will navigate social situations surrounding food, and fear of physical symptoms such as needing to go to the bathroom.
Anxiety can be a normal experience in response to a physical health condition. This is especially so in the initial stages of coeliac disease diagnosis.[5]
However, if anxiety starts to interfere with your daily functioning and wellbeing, this may indicate that it is more unhelpful than helpful.
Suicide Risk
Mental health conditions, such as depression, anxiety, eating disorders, can all increase the risk of suicide. Equally, having a physical health condition, such as coeliac disease, can also increase the risk of suicide.
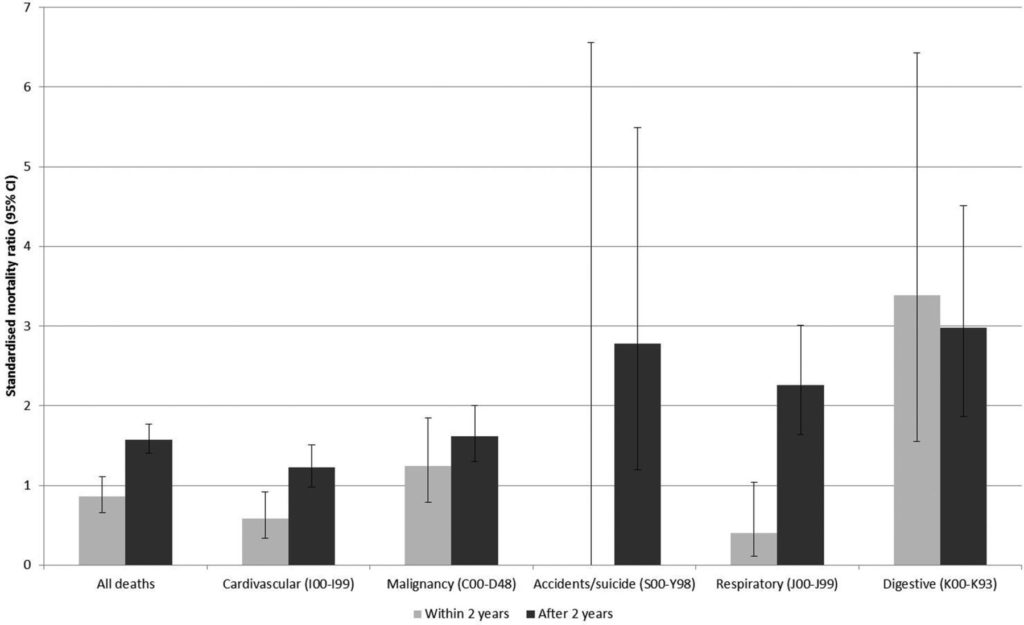
Source: Holmes, G. Mortality in coeliac disease: a population-based cohort study from a single centre in Southern Derbyshire, UK. (2018)
Individuals with coeliac disease have a 50% increased risk of suicide
This was recorded in a Swedish study when compared to the general population; a common presentation of this was also high inflammation markers.[6]
Eating Disorders
With any physical health condition that affects diet, there is always an increased risk for eating disorders. Other predisposing factors can include perfectionism, feelings of inadequacy and social insecurity.
Bulimia nervosa is the most common eating disorder associated with coeliac disease.[5]
Addison’s disease (insufficient adrenal hormones)
Addison’s disease, also known as adrenal insufficiency, is when the adrenal glands produce either too much or too little cortisol (stress hormone).
Symptoms of Addisons’s disease can overlap with symptoms of coeliac disease, such as:
- fatigue
- nausea
- dizziness[7]
Research has shown that those with coeliac disease have up to an 11% increased risk for Addison’s disease.[8] Those with Addison’s disease also have an increased risk of coeliac disease.
While it is unclear if one disease causes the other, it is believed that both of these diseases have shared genetic traits, including variants of the HLA DQ2 and DQ8 genes.[8]
These genes are important for autoimmune function and for the body to recognise proteins that are self and non-self.
Related Questions
1. What is life expectancy when diagnosed with coeliac disease?
Those with coeliac disease have a normal life expectancy, provided they manage their treatment by going on a life-long gluten free diet.
2. What genes can make me more likely to develop coeliac disease?
The risk of developing coeliac disease is higher if you have the HLA-DQA1 and HLA-DQB1 genes, which are involved in the body’s immune system.[9]
3. What organ is most affected by coeliac disease?
Coeliac disease affects the small intestine the most as it is unable to absorb nutrients from food.
4. What cancers are associated with coeliac disease?
Non-hodgkin’s lymphoma, enteropathy-associated T-cell lymphoma (EATL), and adenocarcinoma are the cancers most associated with coeliac disease; however this is quite rare.[10]
Let us know in the comments below if you have any questions, and also feel free to share this article with a friend or family member who might be experiencing digestive issues since gluten sensitivity often goes undiagnosed.
Having passion for mental health and nutrition, Carly’s goal is to become a registered psychologist with a focus on self-care – food, exercise, and sleep. She has a special interest in various mental health disorders, plant-based diets, and the relationship between food and mood…
If you would like to learn more about Carly, see Expert: Carly Hanna.
References
(1) Laurikka P, Kivelä L, Kurppa K, Kaukinen K. Systemic consequences of coeliac disease. Alimentary Pharmacology & Therapeutics. 2022 Jul;56:S64-72. https://onlinelibrary.wiley.com/doi/full/10.1111/apt.16912
(2) Kreutz, Johanna M, et al. “Narrative Review: Nutrient Deficiencies in Adults and Children with Treated and Untreated Celiac Disease.” Nutrients, vol. 12, no. 2, 2020, p. 500–, https://doi.org/10.3390/nu12020500
(3) Infertility and Coeliac Disease. Coeliac UK. Accessed online 16/04/23. Retrieved from https://www.coeliac.org.uk/information-and-support/coeliac-disease/conditions-linked-to-coeliac-disease/infertility-and-coeliac-disease/#:~:text=Women%20with%20coeliac%20disease%20may,a%20lower%20body%20mass%20index.
(4) Rees, Catherine. Coeliac Disease and Fertility in New Zealand Women. Coeliac New Zealand. Accessed online 16/04/23.
(5) Cossu, Giulia et al. “Coeliac disease and psychiatric comorbidity: epidemiology, pathophysiological mechanisms, quality-of-life, and gluten-free diet effects.” International review of psychiatry (Abingdon, England) vol. 29,5 (2017): 489-503. doi:10.1080/09540261.2017.1314952
(6) Ludvigsson JF, Sellgren C, Runeson B, Långström N, Lichtenstein P. Increased suicide risk in coeliac disease—a Swedish nationwide cohort study. Digestive and Liver Disease. 2011 Aug 1;43(8):616-22. https://doi.org/10.1016/j.dld.2011.02.009
(7) Associated Conditions. Coeliac Australia. Accessed online 16/04/23.
(8) Elfström P, Montgomery SM, Kämpe O, Ekbom A, Ludvigsson JF. Risk of primary adrenal insufficiency in patients with celiac disease. The Journal of Clinical Endocrinology & Metabolism. 2007 Sep 1;92(9):3595-8.
(9) Celiac Disease. MedlinePlus. Accessed online 16/04/23. Retrieved from https://medlineplus.gov/genetics/condition/celiac-disease/#:~:text=The%20risk%20of%20developing%20celiac,leukocyte%20antigen%20(HLA)%20complex%20.
(10) Celiac Disease and Cancer. Beyond Celiac. Accessed online 16/04/23. Retrieved from https://www.beyondceliac.org/celiac-disease/related-conditions/cancer/#:~:text=There%20are%203%20types%20of,celiac%20disease%20is%20quite%20rare.






